Fig. 11.1
Amputation levels for isolated digital amputations (according to Gosset and Michon)
11.1.1.1 At the Level of the 3rd Phalanx
The amputation is always definitive; we distinguish 4 zones (Fig. 11.2).
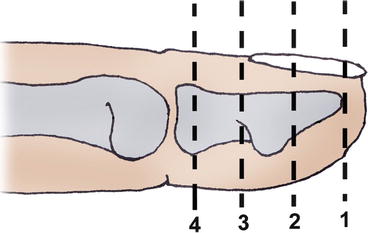
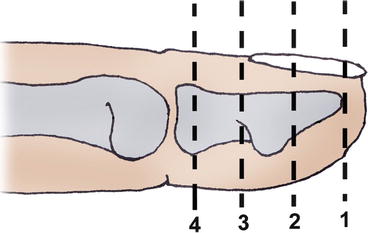
Fig. 11.2
Topography of the distal amputations at the level of the 3rd phalanx (zones 1 to 4)
In zones 1, 2, and 3, we keep the length of the 3rd phalanx that’s left.
In zone 4, it isn’t necessary to keep the base of the 3rd phalanx. We regularize the head of the 2nd phalanx (Fig. 11.3).
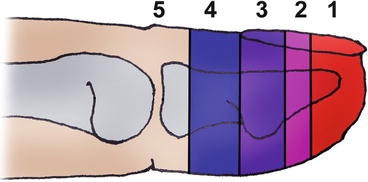
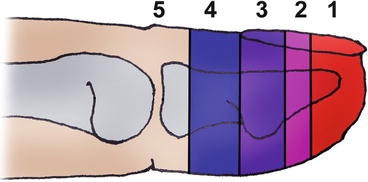
Fig. 11.3
Level and indication of the definitive amputations of the distal phalanx (long finger). 1 Preservation of the nail and pulp reconstruction with a sensorial flap. 2 Preservation of the nail to be discussed. 3 Preservation of the 3rd phalanx: eventual reconstruction with a sensorial flap, nail sterilization. 4 Preservation of the 3rd phalanx to be discussed, nail preservation. 5 Preservation of the 3rd phalanx contraindicated, amputation at the head of the 2nd phalanx
11.1.1.2 At the Level of the 2nd and 1st Phalanges
The amputation will be realized at the head of the phalanges or through the diaphyseal segment.
11.1.1.3 At the Level of the Metacarpophalangeal Joints
We try to keep the head of the metacarpal to keep the bone length and therefore keep the architecture of the metacarpal arch (integrity of the palm’s width).
For the 3rd and 4th fingers, a new commissure is created. We can then realize a proximal resection of the segment or a digital translocation if a functional discomfort appears (or with an esthetic purpose).
11.1.1.4 At the Level of the Metacarpals (Proximal)
The amputation will never be realized as an emergency, except if the damage is too important.
11.1.2 Amputation of the Thumb
The thumb is, functionally, the most important finger of the hand; therefore, we can’t apply the same rules than for the long fingers. Everything will be done to keep as much length as possible, even if it leads to joint stiffness (arthrodesis).
11.1.3 Poly-digital Amputations
In this case, everything will be done to keep as much stump length as possible, in a functional purpose.
11.1.4 Transmetacarpal Amputations
We will also try to keep as much length as possible.
11.2 Rehabilitation and Orthotic Treatment
The rehabilitation usually starts early to avoid eventual stiffness and regain the optimal function of the hand.
The priority goal is to regain the physiological joint amplitudes (without disturbing the tissue healing).
Once the scars are closed, we can add scar remodeling and sensorial exercises. We also start functional reintegration for the stump not to be excluded.
We’ll have to watch carefully for pain to avoid the complex regional pain syndrome (CRPS).
11.2.1 Rehabilitation Protocol (Fig. 11.4) [3]

Fig. 11.4
Rehabilitation protocol
11.2.1.1 Cutaneous Healing Phase (d0 to d21)
In this phase, the patient still has bandages, so the rehabilitation is limited. It’s important to fight against pain and stiffness.
The patient must do some self-rehabilitation exercises at home.
We have to be alert for signs of CPRS (if inadequate treatment), phantom pain, or neuromas.
Fight Against Pain
Analgesic Electrotherapy: 100 Hz (TENS) or 1 Hz
The active electrode is placed as close as possible to the painful area and the other at the level of the corresponding vertebral level. The intensity will be regulated so that the patient feels a tingling sensation, not a muscular contraction.
Transcutaneous Vibratory Stimulation (Fig. 11.5) [2]

Fig. 11.5
Transcutaneous vibratory stimulation on the stump
It will start early, through the bandages, as it has an analgesic effect and prevents painful and sensorial neuromas.
For an analgesic effect, we use low-frequency vibrations (100 Hz) and with a low amplitude on the painful area. If the patient feels pain when contacting with the vibration, we’ll use it far from the painful area. We’ll try increasing the amplitude of the vibrations and getting closer to the painful area little by little, without creating any pain. We consider the result satisfying with a 100 Hz frequency and maximum amplitude.
The transcutaneous vibratory stimulation also has a proprioceptive action that creates an illusory sensation of movement by stimulating the cutaneous mechanoreceptors and exciting the muscle spindles. This will replace the lack of use of the hand and keep the movements intact. The active movements will be regained easier.
The early stimulation of the stump allows a better acceptance of the treatment when we remove the bandage. It also lowers the anxiety toward the trauma and its consequences.
Fight Against Vasomotor Disorders
Circulatory massage once the scar is closed (Fig. 11.6a).
Fig. 11.6
(a) Scar massage of the stump, (b) pressotherapy, (c) cryotherapy
Pressotherapy with disto-proximal compression to drain the superior limb (Fig. 11.6b)
Cryotherapy (Fig. 11.6c)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








