10 American neuromuscular therapy
History
As detailed in Chapter 2, neuromuscular therapy (NMT) evolved out of the work of a number of clinicians working in both Europe and the USA.1 The ‘evolutionary’ development of NMT produced some confusion regarding the name itself. In its earlier stages, American ‘NMT’ represented neuromuscular ‘therapy’, whereas, in Europe, the preferred term had been neuromuscular ‘technique’. In the past decade, as a number of methods emerged, practitioners began to use these two terms interchangeably. Distinctions between the various NMT methods still exist, although there is less separation with regards to the use of the terms ‘therapy’ and ‘technique’, apart from osteopathic training in the UK, where the ‘T’ element of NMT refers to ‘technique’.
The first American protocols of NMT, developed in the late 1970s and early 1980s were based largely on the methods devised and taught by the late Raymond Nimmo (DeLany 1999). Nimmo’s research into the pathological influences and relevance, as well as the therapeutic implications of treating ‘noxious pain points’ mirrors closely that of his contemporary, Janet Travell, in relation to her research into myofascial trigger points. Nimmo’s protocols were subsequently modified and expanded by Paul St John, who studied with Nimmo, and then by St John and Judith (Walker) DeLany, who worked together in the 1980s. Both St John and DeLany have continued expanding their separate NMT programmes over the last decade.
While the American protocols of NMT were initially based on that of Nimmo, the platform of application was strongly influenced by the writings and research of Travell & Simons (1983, 1992), Vannerson & Nimmo (1971), Cailliet (1977), Chaitow (1980) and others. Both St John’s and DeLany’s variations on Nimmo’s protocols resulted in revisions of previous concepts and methodology, leading to significant changes in recommended treatment techniques. St John incorporated structural homeostasis of the body and cranium as the basis of his St John Method™, while DeLany took a broader view in NMT American version™ (Chaitow & DeLany 2000, 2002, 2008), where she utilized a systematic approach with attention paid to biochemical, biomechanical and psychosocial factors.
Platform of NMT American version™
Homeostasis incorporates the processes through which the various functions of the body, including everything from postural adjustments to the chemical compositions of the body’s fluids, are maintained in balance (Stedman 1998). It is through this goal of equilibrium that the body deals with the many stresses and demands placed upon it in daily life, accomplishing this through adaptation and compensation. If stresses are excessive, or if compensation mechanisms have been compromised or overloaded, the adverse effects of decompensation, where frank disease and degeneration occur, are likely to emerge (Chaitow & DeLany 2008).
Categories
The broad foundation of NMT American version™ is based on the assessment of three categories capable of adaptation that, on a constant basis, modify, adjust to and compensate for the stresses of life (Table 10.1). Within the three categories – biomechanical, biochemical and psychosocial – are to be found subdivisions of most of the major influences on health, with a number of these features being commonly involved in causing or intensifying pain (Chaitow 1996, 2003, Chaitow & DeLany 2000, 2008). In addressing these categories, it is acknowledged that there can be local and/or global (systemic) causes of pain and dysfunction, as well as numerous perpetuating factors, that, if left untreated, may cause ‘mysterious’ recurrence of the condition (Simons et al 1999). Local, global and perpetuating factors should all be considered in a thorough recovery programme. These include Chaitow & DeLany (2000, 2008), amongst others, locally dysfunctional states such as:
as well as the following global factors that affect the whole body systemically:
• genetic predisposition (e.g. connective tissue factors leading to hypermobility) and inborn anomalies (e.g. short leg)
• nutritional deficiencies and imbalances
• toxicity (exogenous and endogenous)
• infections (chronic or acute)
• endocrine (hormonal) imbalances and deficiencies (especially thyroid)
• global (systemic) inflammation
• stress (physical or psychological)
• trauma (abrupt as well as cumulative)
• posture (both static and dynamic and including patterns of misuse and muscle substitution)
Table 10.1 Major influences on health that are commonly involved in causing or intensifying pain can be broadly classified into three categories. The examples given can be readily seen as not only individually problematic, but to profoundly interact with each other and create a cascade of effects.
| Biomechanical | Biochemical | Psychosocial |
|---|---|---|
| Trauma | Inflammation | Stress |
| Postural | Dehydration | Guilt |
| Muscular (including trigger points) | Nutritional | Fear |
| Congenital | Hormonal | Anxiety |
| ‘Wear and tear’ | Ischaemia | Emotions |
| Joint dysfunction | Toxicity | Litigation |
| Overuse, misuse, disuse, abuse | Immune response | Depression |
| Neural entrapment and/or compression | Somatization |
The original six factors of NMT
Although the current approach of NMT American version™ encompasses consideration of many additional factors beyond the classic six, the original six still remain the primary focus of the approach. When working with a person in chronic pain, these six subdivisions derived from the local and global lists above should be addressed systematically to assess for and, hopefully, reduce underlying causes of discomfort and/or dysfunction. If assessment of one or more of these factors is omitted, the person may plateau or regress in his or her recovery. These particular six factors should be considered, assessed for, and clinically addressed (if needed) by the practitioner in all patients (Chaitow & DeLany 2000, 2008). If the practitioner is without skill or licence in one or more of these foundational tools, it is suggested that the patient be referred to another practitioner who is suitably trained and licensed in the subject. If progress is not seen within a few treatments, or if pain, fatigue, or other primary symptoms return, other factors (hormonal, organ or bone health, toxicity, etc.) should be considered. The six factors, as noted by DeLany (2002), are:
Ischaemia – a state in which the current oxygen/blood supply is inadequate for the current physiological needs of tissue. Causes of ischaemia can be pathological (narrowed artery or thrombus), biochemical (vasoconstriction by the body to reduce flow to a particular area), anatomical (tendon obstruction of blood flow) or as a result of overuse or facilitation. Ischaemia reduces the level of oxygen, nutrients and waste removal and the tension produced by the resultant muscle shortening can alter joint mechanics and/or entrap neural structures. Ischaemia, and its resultant local energy crisis, can also lead to the production of trigger points (Simons et al 1999).
Trigger points (TrPs) – localized areas within muscle bellies (central TrPs) or at myotendinous or periosteal attachments (attachment TrPs) which, when sufficiently provoked, produce a referral pattern to a target zone. The referral pattern may include pain, tingling, numbness, itching, burning or other sensations. In addition to its location (central or attachment), a TrP can be classified as to its state of activity (active or latent) as well as whether it is primary, key or satellite. (See also trigger point formation theories, described in detail in Ch. 3.)
Neural interferences – compression (by osseous structures) or entrapment (by myofascial tissues) of neural structures may result in muscle contraction disturbances, vasomotion, pain impulses, reflex mechanisms and disturbances in sympathetic activity. Since neurovascular structures course along fascial structures (sheaths, planes, etc.), entrapment by fascial distortions is common. Release of the fascia and mobilization of the neural structures should be components of the manual protocols.
Postural and biomechanical dysfunctions – repeated postural and biomechanical insults over a period of time, combined with the somatic effects of emotional and psychological origin, will often present altered patterns of tense, shortened, bunched, fatigued and, ultimately, fibrotic tissues with resultant alterations from healthy postural positioning. Muscle substitution occurs, with resultant alterations in firing patterns that can escalate to further dysfunctional use. Although structural assessment (postural analysis) has inherent value, it fails to consider patterns of use that may not be displayed in static position. Dynamic pronation, alterations in gait, and other use patterns should be assessed and corrected due to their ability to perpetuate obvious and very subtle dysfunctions.
Nutritional factors – nutritional deficiencies/imbalances, sensitivities, allergies and stimulants all play roles in myofascial health as well as hormonal, emotional and mental health. The author of this chapter considers the nutritional component to be the most important factor in health. Excess or lack of those that provide energy (protein, carbohydrate, fat) as well as those that support metabolism (vitamins, minerals, water) can have a significant impact on health and chronic pain.
Emotional well-being – the degree and type of the emotional and stress loads the individual is carrying can influence various systems of the body. Hormones and neurotransmitters are chemical messengers of the body that are strongly affected by stress, thought and emotions. Likewise, they can impact mental, physical and emotional response to stress, with resultant cascades of further chemical interfaces. Ultimately, if excessive or prolonged, these factors can result in distress and disease.
Application of NMT
Clinical application of NMT
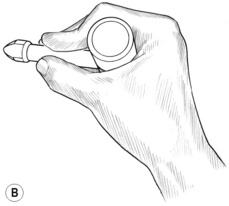
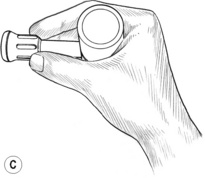
Application of dry techniques is generally followed by manipulation or lightly lubricated gliding, which is aimed at increasing blood flow and ‘flushing’ tissues while simultaneously evaluating for ischaemic bands and/or trigger points. Static digital pressure is subsequently employed in order to release ischaemic bands and for treatment of trigger points, and is usually applied after several repetitions of gliding or other forms of manipulation of the tissues have been completed. Pressure bars may be used instead of (or in addition to) finger or thumb compression (Fig. 10.1B,C) in certain areas; however, precautions apply and proper training is suggested. Manually applied gliding strokes are usually repeated after applications of compression, friction or pressure bar techniques.
NMT techniques
• Skin rolling and tissue lifting techniques can be applied to soften the fascia associated with the skin and underlying muscles. The skin can be grasped and lifted, thereby creating mechanical tension on the subcutaneous fascia, which assists in changing the state of the fascia’s ground substance from a ‘gel’ to a ‘sol’ (Oschman 1997) due to its thixotropic properties (DeLany 2000a). The tissue can also be rolled between the fingers and thumb. Subcutaneous tissue layers and/or muscle bellies may be grasped and lifted, then manipulated between the fingers and thumb, if tolerable, thereby stretching fascia and separating fascial layers. Any of these may result in increased blood and/or lymph flow. Areas where the skin is adherent are often an indication that the underlying muscles need further treatment.
• Effleurage (gliding stroke) is an important and powerful component of the NMT American version™. It warms the fascia, flushes blood through the tissues, and therefore increases oxygenation and perfusion of nutrients while simultaneously eliminating waste products from the tissues (Yates 1989). During the gliding process, the practitioner will discover contracted bands, nodules and tender points unique to that individual. Gliding repeatedly on these bands often reduces their size and tenacity, lessening the time and effort needed to modify or eliminate them. Clinical experience indicates that the best results tend to come from gliding on the tissues several times, then working somewhere else and returning to glide again. The direction of application of glides may be either with or across the direction of the muscle fibres, and usually involves a combination of both. Following the course of lymphatic flow is particularly suggested if tissues are congested. Unless contraindicated (by inflammation, oedema, etc.), a moist hot pack can be placed on the tissues between gliding repetitions to enhance the effects further. A short time of rest of the tissues is usual before additional gliding. This allows circulatory and drainage functions to flush the tissues further. Tenderness and ischaemia are commonly reduced rapidly in this way.
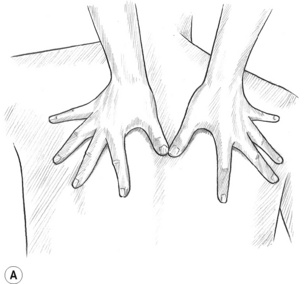
• To glide on the tissues most effectively, the practitioner’s fingers, spread slightly, support and stabilize the hands (Fig. 10.1A) while the thumbs are (most often) the treatment tools. The hand and forearm move as a unit, with the wrist being stable. Little or no motion is allowed in the wrist joints or the thumb joints. Excessive movement in the wrist or thumb may lead to joint problems and inflammation of the practitioner’s forearms, wrists and hands. A proper and stable hand position helps avoid practitioner injury. When two-handed glides are used, the thumbs are side by side (almost parallel), or one ahead of the other, with the tips of the thumbs leading the glide.2 When the distal tips of the thumbs are touching during the glide and the medial side of the thumbs lead the stroke, excessive strain is placed on the thumb joints and practitioner injury is a considerable risk.
• When dealing with tissue that is not excessively tender or sensitive, the ‘glide’ should cover 3–4 inches per second (speed of application is reduced for comfort if tissues are sensitive), which is significantly faster than the thumb stroke used in Lief’s NMT. It is important to develop a moderate gliding speed in order to ensure adequate opportunity for simultaneous palpation of muscles. Too rapid a movement may cause unnecessary discomfort and may also skim over congestion in the tissues, missing vital information sources. Movement that is too slow may displace the tissues, making identification of an individual muscle difficult. A moderate speed will allow for repetitions that significantly increase blood flow and, at the same time, palpation of bands or nodules of ischaemia within the tissues.3
• Compression techniques can be used to press soft tissues against a bone or underlying muscle (flat compression), or the non-lubricated tissues may be lifted and grasped between the finger(s) and thumb (pincer compression). Pincer compression can be broadly applied with flattened fingers (like a clothes’ peg; see Fig. 10.2A) or precisely applied with curved fingers (resembling a ‘C’ clamp; see Fig. 10.2D).
• Static compression (also called TrP pressure release, ischaemic compression or sustained pressure) applies pressure to tissues without movement of the fingers or thumb. Tissues that are ischaemic or those that contain TrPs usually respond well to static compression (see below regarding use of static pressure). For those that are extremely tender, pressure must be modified so as not to be excessive.
• Compression with manipulation can be applied by lifting the tissues and then rolling, bending or twisting them between the fingers and thumb. It is an effective way of mechanically distressing the connective tissue and altering its ground substance from a gel to a sol (DeLany 2000b), and may also help to separate the fibres and increase blood flow. Generally, this technique is used after the tissue tenderness has been decreased by the use of gliding strokes and static compression. It can follow those techniques or be used before TrP pressure release.
• Friction techniques can usually be applied to myofascial tissues with variations, depending on the condition of the tissues and the desired results. It is most often used to soften fibrotic tissues and to alter the quality of adhesions. Friction techniques may include those applied transversely (cross-fibre friction, strumming, snapping or transverse friction) or those applied with the fibre direction (longitudinal friction). If tissues are tender, caution should be exercised as tenderness may be indicative of inflammation. If significant tenderness is present or if application of friction results in tenderness, ice may be applied for 10–15 minutes. Friction on that particular tissue should then be avoided until no evidence of inflammation is present.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree