Allograft Prosthetic Composites for Femoral Revision
Hesham Abdelbary
Allan E. Gross
Case
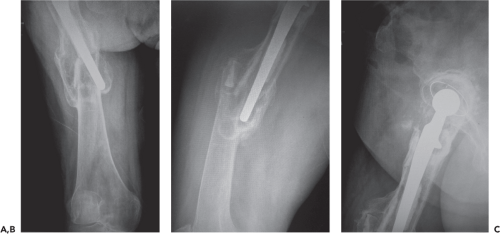
A healthy 50-year-old community ambulator presented to our clinic with significant hip pain and radiographs shown in (Fig. 126.1). The original surgery was a cemented THR that lasted for 15 years until the patient suffered a periprosthetic fracture. This fracture was managed nonoperatively and healed in a malunited position with significant valgus, procurvatum, and shortening of 3 cm. As shown in the radiographs, there is significant bone loss of the proximal femur secondary to severe osteolysis and mechanical loosening of the femoral component; the femoral isthmus is obliterated secondary to the malunion and the extensive osteolysis. Therefore, using standard revision techniques that rely on an intact isthmus for distal fixation of the femoral implant will be suboptimal in this scenario.
Introduction
One of the major challenges that revision hip surgeons can encounter is massive segmental bone loss of the proximal femur with disruption of the isthmus. These massive defects can compromise standard revision options that require an intact isthmus for press-fit distal fixation of the femoral component. Such extensive bone loss can be caused by stress shielding, massive osteolysis from wear debris, mechanical loosening, infections requiring multiple revisions as well as periprosthetic fractures, especially Vancouver B3 variants (1).
There are four main surgical options available to manage circumferential bone loss of the proximal femur that extends into or distal to the isthmus; (1) modular endoprosthesis, (2) allograft-prosthetic composite (APC), (3) impaction grafting,
and (4) resection arthroplasty. Due to the significant poor functional outcomes associated with resection arthroplasty, it is reserved as a palliative procedure for pain relief after multiple failures of other reconstructive options. The remarkable advances in modular implant designs combined with their technically less demanding surgeries, when compared to allograft reconstruction, have expanded the use of modular endoprostheses and made them more popular among revision surgeons. However, these endoprostheses fail to restore proximal femoral bone stock, which remains one of the primary goals for revision hip surgery, especially in the younger age groups. In the situation where there is loss of isthmus, fixation of endoprosthesis can only be achieved by cementing into the residual host femur, or by concomitant ipsilateral knee replacement. Both of these solutions are not favorable because of high risk for instability and mechanical failure, as well as greater loss of host bone stock. Therefore reconstruction techniques using allografts should be considered as valuable alternatives in our arsenal to reconstruct massive defects of the proximal femur.
and (4) resection arthroplasty. Due to the significant poor functional outcomes associated with resection arthroplasty, it is reserved as a palliative procedure for pain relief after multiple failures of other reconstructive options. The remarkable advances in modular implant designs combined with their technically less demanding surgeries, when compared to allograft reconstruction, have expanded the use of modular endoprostheses and made them more popular among revision surgeons. However, these endoprostheses fail to restore proximal femoral bone stock, which remains one of the primary goals for revision hip surgery, especially in the younger age groups. In the situation where there is loss of isthmus, fixation of endoprosthesis can only be achieved by cementing into the residual host femur, or by concomitant ipsilateral knee replacement. Both of these solutions are not favorable because of high risk for instability and mechanical failure, as well as greater loss of host bone stock. Therefore reconstruction techniques using allografts should be considered as valuable alternatives in our arsenal to reconstruct massive defects of the proximal femur.
Allograft reconstructions provide the potential to preserve and enhance the patient’s bone stock for possible future revision surgeries. They also allow for the preservation of important muscle and tendon attachments to the proximal femur for a better functional outcome. Although impaction grafting has shown some success in patients with femoral bone loss, it is best used in the setting of contained or limited circumferential bone loss that only involves the calcar and the lesser trochanter (LT) but does not extend into the diaphysis unless, once again, the cortical tube of the proximal femur is intact (2). In the setting of substantial segmental bone loss, impaction grafting has been associated with a higher risk for component subsidence, loosening and an increased risk for periprosthetic fractures (3).
Our group has successfully used APC reconstruction in revision hip surgery since 1984 (4). The concept of APC reconstruction combines the use of a long-stem femoral prosthesis that is positioned and firmly secured within a proximal femoral allograft (PFA) with a pressurized cement mantle (5). This allograft is secured distally within the host femur using an oblique or a step-cut osteotomy that can be augmented with a plate or cerclage wires to achieve the necessary initial stability required for healing of the allograft to the native femur to occur.
Indications and Contraindications
Numerous systems have been established to classify femoral defects. Some of these classification systems provide useful guidance with regard to the type of prosthetic reconstruction that the bone can support as well as the need for allograft reconstruction of the proximal femur. Two useful and commonly used classifications are the Paprosky and Gross systems (2). Based on these two systems, there are two main indications for considering the use of APC to reconstruct proximal femoral defects; (1) Paprosky type III B and type IV—with segmental bone loss that extends into the diaphysis and damages supportive isthmus required for distal fixation, and (2) Gross type IV—with full circumferential uncontained defects greater than 5 cm in length, extending into and involving the diaphysis. Indications for APC reconstruction can be extended to the setting of Vancouver B3 periprosthetic fracture with Paprosky type III B or IV bone loss or Gross type IV femoral defects. A relative indication for APC use is in the oncologic setting of proximal femoral excision for a malignancy (6).
APC is contraindicated in patients who are medically unwell and cannot tolerate the length of the procedure (proximal femoral replacement with an endoprosthesis is a quicker operation), as well as in those who are unable to comply with the required postoperative rehabilitation program which requires an extended period of protected weight bearing to allow for healing of the allograft to the remaining host femur and for soft tissue attachment to the allograft to occur. The presence of active infection is another absolute contraindication for this procedure, although our group demonstrated the safe use of APC in second-stage treatment of infected hip arthroplasty with massive proximal femoral bone loss after the eradication of infection, with survivorship of 93% at 10 years (7). There is no reconstruction technique for massive bone defects around the proximal femur that provides a perfect or risk-free solution to the patient. Therefore, it is important to be aware of the limitations associated with each available surgical option, and to tailor the choice of reconstruction to the individual clinical scenario. This chapter will discuss the surgical technique of APC reconstruction and will highlight the potential challenges and complications associated with it.
Surgical Technique
This surgical procedure can be divided into FIVE major parts:
Surgical approach
Initial preparation of the PFA
Trial reduction prior to fixation of prosthesis to PFA
Final preparation of APC and fixation of prosthesis to the PFA
Fixation of APC to host femur
I. Surgical approach
Our preferred surgical approach for this procedure is the modified trochanteric slide, where the trochanter is osteotomized and translated anteriorly while attached to a continuous soft tissue sleeve of abductors proximally and vastus lateralis distally (Fig. 126.2A,B). The modified trochanteric slide is performed as described in Chapter 103. This is a very extensile approach that provides excellent exposure to the acetabulum and femur. The continuous soft tissue sleeve to the trochanter aims to maintain a higher rate of union by preserving its vascularity. The distal attachment of the vastus lateralis also controls migration of the trochanteric fragment by neutralizing proximal shear forces (8). For this approach, 1 cm of the posterior GT attached is left attached to the femur in order to preserve attachments of the short external rotators and posterior capsule, which improves hip stability and decrease the risk for posterior dislocations (9). In the situation where the greater trochanter is too osteolytic or has been thinned secondary to multiple revisions, a slide
can still be performed in a similar fashion with a continuous soft tissue sleeve of the abductors and vastus lateralis mobilized anteriorly as one unit while still preserving the attachments of posterior soft tissue structures to the proximal femur.
can still be performed in a similar fashion with a continuous soft tissue sleeve of the abductors and vastus lateralis mobilized anteriorly as one unit while still preserving the attachments of posterior soft tissue structures to the proximal femur.
The next step is to extend the exposure of the proximal femur to allow for intraoperative visualization of the junction between the deficient and healthy host bone, which will be the anatomic location for the femoral osteotomy. Careful preoperative planning and consideration of important factors; such as the length of bone defect, location of deformity, and distal extent of the femoral prosthesis or cement mantle should help determine the level of the osteotomy (10). Exposing the rest of the femur is achieved posterolaterally by sweeping the fibers of the vastus lateralis off the lateral intermuscular septum with careful cauterization of perforator vessels arising from the femoral profunda. Great care should be taken to avoid retraction of perforator branches behind the intermuscular septum and causing uncontrolled bleeding in the posterior compartment. The proximal deficient femur is then split longitudinally in the coronal plane down to the predetermined level of healthy host bone that does not require replacement by the allograft. Please see Fig. 126.2B in attachment. At the level of healthy femur, transverse cuts are made anteriorly and posteriorly, each extending about a quarter of the way around the femur, leaving the medial cortex of the femur intact to be used as the step cut or oblique osteotomy. Although, a step-cut osteotomy may offer more rotational stability, an oblique osteotomy allows for easier adjustments of the version without making major changes to the osteotomy. The oblique osteotomy should be as long as possible with a minimum of 2 cm in length, while the step cut should be 2 × 2 cm (4,8). There are instances where there is a mismatch between the medullary sizes of the host bone and the allograft that leads to the telescoping of the graft into the host femur. This intussusception makes the step-cut or oblique osteotomy unnecessary, and can achieve stability between the graft and host femur secondary to good press-fit fixation.
The proximal femur is opened as a book while preserving all soft tissue attachments to each fragment to maintain their vascularity. These fragments will eventually be wrapped around the final APC construct as vascularized onlay grafts to enhance union of the graft–host junction (4). An anterior capsulectomy is then performed to allow for the dislocation of the femoral head and extraction of the old femoral component. The old cement mantle and fibrous tissue can be removed under direct visualization. The distal host femur is reamed gently over a guidewire to open the canal enough for a loose fit of the femoral stem. Any autograft bone obtained during the removal of the implant or from host bone reaming should be saved for the host–allograft bone junction at the end of the procedure.
II. Initial preparation of the PFA
We recommend conducting this part of the procedure on a separate sterile surgical table by a second surgical team, in order to enhance operative efficiency. A whole intact PFA
should be ordered from the bone bank with enough length to bypass the host proximal femoral defect by approximately 5 cm to allow for graft adjustment and limb lengthening if necessary (10). We prefer using deep-frozen allografts stored at −80°C and irradiated with 2.5 Mrad to lower the immunogenic and infection risk. This dose of irradiation does not substantially affect graft strength (4). Other groups in the literature reported using nonirradiated fresh allografts stored just above 0°C to help preserve osteocyte viability and biomechanical properties.
should be ordered from the bone bank with enough length to bypass the host proximal femoral defect by approximately 5 cm to allow for graft adjustment and limb lengthening if necessary (10). We prefer using deep-frozen allografts stored at −80°C and irradiated with 2.5 Mrad to lower the immunogenic and infection risk. This dose of irradiation does not substantially affect graft strength (4). Other groups in the literature reported using nonirradiated fresh allografts stored just above 0°C to help preserve osteocyte viability and biomechanical properties.
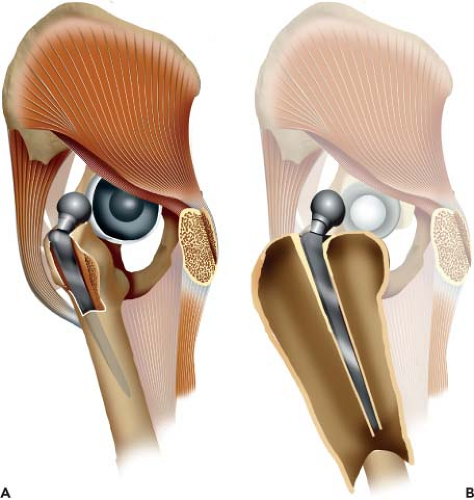
The allograft should be brought into the operating room at the beginning of the case and only unwrapped after the surgeon has ruled-out infection. If there is any suggestion for infection at the time of surgery, the revision procedure should be staged. The allograft should be swabbed for aerobic and anaerobic cultures before immersing it in warm 50% Betadine solution. After thawing the allograft, the femoral head is excised at the base of the LT to facilitate the insertion of the femoral implant and allow room for adjusting version. Please note that limb lengthening is achieved by the length of the allograft bellow the LT and not via its neck cut. The graft’s GT is then excised but a bed of cancellous bone is left to allow for the reattachment of the host trochanter. Please see illustration on power point slide (Fig. 126.3) The excised femoral head and GT are morselized and saved as allograft for the latter part of the procedure.
 Figure 126.3. The black line depicts the trajectory of recommended trochanteric cut of the allograft. The two land marks are vastus lateralis ridge distally and piriformis fossa proximally. |
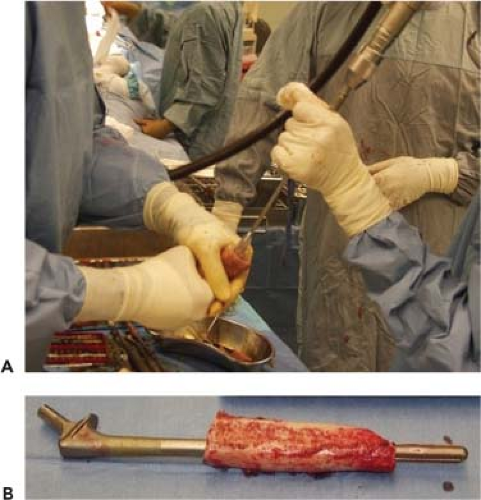 Figure 126.4. A trial with 300-mm long smooth-tapered femoral stem with a 13- to 14-mm diameter is most commonly used to allow for cementation into the allograft. |
The PFA is then secured in vice grip and sequentially reamed to accommodate a good fit for a femoral prosthesis with cement mantle of at least 2 mm. In order to decrease the risk for graft resorption and stress shielding, over reaming the allograft to accommodate a larger femoral component that matches the almost always wider distal host femur should be avoided (2). We most commonly use a 300-mm long implant with a 13 to 14 mm diameter, which does not usually provide a distal press fit. The femoral stem is also smooth and tapered to allow for cementation into the allograft (Fig. 126.4A,B). The trial femoral stem is then inserted into the PFA to formulate the provisional APC.
III. Trial reduction prior to fixation of prosthesis to PFA
This is a critical step of the procedure since it guides important modifications and adjustments to the allograft–prosthesis construct before committing to the final product. During trialing, it is important to assess the following factors; (1) stability of the hip joint, (2) restoration of leg length and soft tissue tensioning, (3) appropriate version and offset, (4) stability and alignment of the osteotomy at the APC–host femur junction.
At this stage, any acetabular reconstruction required should be done first so that the length of the femoral allograft can be determined accurately. We prefer using an outrigger device that consists of a Steinmann pin, which is inserted into the iliac crest as a reference point, and a metal arm that measures the distance from the pin to another reference point marked on the femur. This device, which measures leg length and offset, is secured and calibrated at the beginning of the procedure before dislocating the hip joint (Fig. 126.5A). To determine the appropriate length of the allograft, the trial
femoral implant selected in step II is first inserted into the host canal without the allograft, and then reduced into the acetabulum. The trial stem should bypass the graft–host junction by a minimum of 5 cm3



femoral implant selected in step II is first inserted into the host canal without the allograft, and then reduced into the acetabulum. The trial stem should bypass the graft–host junction by a minimum of 5 cm3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree