Allograft Osteochondral Plugs
William Bugbee
Fresh osteochondral allografts are becoming increasingly popular in articular cartilage reconstruction in the knee. The ability to restore diseased or damaged cartilage with mature hyaline cartilage tissue is attractive, and the surgical technique for implanting plugs or dowel-type grafts in simple femoral condyle lesions is fairly straightforward. A large body of basic science and clinical outcome data support the use of fresh osteochondral allografts in clinical practice (3).
INDICATIONS/CONTRAINDICATIONS
Fresh osteochondral allografts possess the ability to restore a wide spectrum of articular and osteoarticular pathology, as a result, the clinical indications cover a broad range of pathology. As is true for other restorative procedures, in addition to evaluating the particular articular lesion, the careful assessment of the entire joint, as well as the individual, is important. Many proposed treatment algorithms suggest the use of allografts for large lesions (>2 or 3 cm) or for salvage in difficult reconstructive situations where bone loss is also present. In our experience, allografts can be considered as a primary treatment option for osteochondral lesions greater than 2 cm (approximately) in diameter, as is typically seen in osteochondritis dissecans (OCD) and osteonecrosis. Fresh allografts are also useful as a salvage procedure when other cartilage-restorative procedures, such as microfracture, osteoarticular transfer system (OATS), and autologous chondrocyte implantation, have been unsuccessful.
Additionally, allografts often are used for salvage reconstruction of post traumatic defects of the tibial plateau or the femoral condyle. Other indications for allografting in the knee include treatment of patellofemoral chondrosis or arthrosis and in very select cases of unicompartmental tibiofemoral arthrosis (Table 33-1).
Relative contraindications to the allografting procedure include uncorrected joint instability or uncorrected malalignment of the limb. An allograft may be considered in combination or as part of a staged procedure in these settings. Allografting should not be considered an alternative to prosthetic arthroplasty in an individual with symptoms and acceptable age and activity level for prosthetic replacement. In the younger individual, bipolar and multicompartmental allografting have been modestly successful. The presence of inflammatory disease or crystal-induced arthropathy is considered a relative contraindication, as well as is any unexplained synovitis. The use of fresh osteochondral allografts in individuals with altered bone metabolism, such as is seen in chronic steroid use, smoking, or even nonsteroidal anti-inflammatory agents, has not been studied extensively. Unlike other cartilage procedures, relative size of the lesion (large or small) is not considered a contraindication to allografting.
PREOPERATIVE PLANNING
Common to all fresh allografting procedures is matching the donor with recipient. This is done on the basis of size. In the knee, an anteroposterior radiograph with a magnification marker is used, and a measurement
of the medial-lateral dimension of the tibia, just below the joint surface, is made (Fig. 33-1). This corrected measurement is used, and the tissue bank makes a direct measurement on the donor tibial plateau. Alternatively, a measurement of the affected condyle can be performed. A match is considered acceptable at ± 2 mm; however, it should be noted that there is a significant variability in anatomythat is not reflected in size measurements. In particular, in treating OCD, the pathologic condyle typically is larger, wider, and flatter; therefore, a larger donor generally should be used. When using allograft plugs or dowels, one is generally safe with a larger donor. Small donor condyles lead to problems with matching radius of curvature, particularly for grafts over 20 mm in diameter. Most femoral condyle lesions can be treated using dowel-type grafts. Commercially available instruments (Arthrex, Naples, FL) simplify the preparation, harvesting, and insertion of these grafts, which may be up to 35 mm in size (Fig. 33-2). Perhaps the most important step in preoperative planning is understanding that one is using human tissue and performing a transplantation. Respect for the donation process, understanding the recovery, processing, and safety issues are minimum requirements necessary for the surgeon wishing to use fresh allograft tissue.
of the medial-lateral dimension of the tibia, just below the joint surface, is made (Fig. 33-1). This corrected measurement is used, and the tissue bank makes a direct measurement on the donor tibial plateau. Alternatively, a measurement of the affected condyle can be performed. A match is considered acceptable at ± 2 mm; however, it should be noted that there is a significant variability in anatomythat is not reflected in size measurements. In particular, in treating OCD, the pathologic condyle typically is larger, wider, and flatter; therefore, a larger donor generally should be used. When using allograft plugs or dowels, one is generally safe with a larger donor. Small donor condyles lead to problems with matching radius of curvature, particularly for grafts over 20 mm in diameter. Most femoral condyle lesions can be treated using dowel-type grafts. Commercially available instruments (Arthrex, Naples, FL) simplify the preparation, harvesting, and insertion of these grafts, which may be up to 35 mm in size (Fig. 33-2). Perhaps the most important step in preoperative planning is understanding that one is using human tissue and performing a transplantation. Respect for the donation process, understanding the recovery, processing, and safety issues are minimum requirements necessary for the surgeon wishing to use fresh allograft tissue.
TABLE 33-1. Major Indications for Fresh Osteochondral Allografting of the Femoral Condyle | |||||
|---|---|---|---|---|---|
|
SURGERY
For most femoral condyle lesions, allografting can be performed through a miniarthrotomy. In most situations, a diagnostic arthroscopy has been performed recently and is not a necessary component of the allografting procedure. However, if there are any unanswered questions regarding meniscal status, or the status of the other compartments, a diagnostic arthroscopy can be performed prior to the allografting procedure. Examination under anesthesia is done in the standard fashion, as is the diagnostic arthroscopy when the surgeon feels this is indicated. Only rarely do we perform arthroscopy, as adequate data have typically been collected prior to beginning the process of graft acquisition.
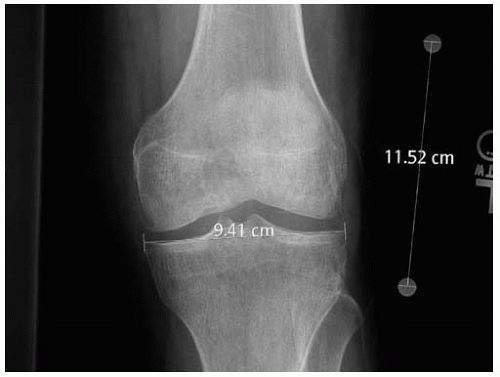 FIGURE 33-1 Radiographic technique for graft sizing. In this example the corrected tibial width is 81 mm (9.41 × 10/11.52). |
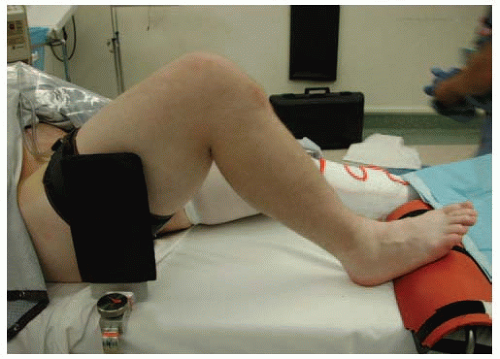
Patient Positioning
The patient is positioned supine, with a tourniquet on the thigh. A leg holder is valuable in this procedure to position the leg in between 70 and 100 degrees of flexion, and to access the lesion (Fig. 33-3). At least one surgical assistant is necessary to provide adequate retraction and leg position for working through the mobile window of the small arthrotomy.
Technique
The fresh graft is inspected to confirm the adequacy of the size match and quality of the tissue prior to opening the knee joint. It is important to keep the graft moist during the procedure; generally, it is left in the packaging media when not being instrumented.
A midline incision is made with the knee in flexion from the center of the patella to the tip of the tibial tubercle. This incision is preferred in anticipation of further surgery in the patient’s lifetime. This incision is elevated subcutaneously, either medially or laterally to the patellar tendon, depending on the location of the lesion (either medial or lateral). A retinacular incision is then made from the superior aspect of the patella inferiorly. Great care is taken to enter the joint and to incise the fat pad without disrupting the anterior horn of the meniscus. In some cases in which the lesion is posterior or very large, the meniscus must be detached and reflected; generally, this can be done safely, leaving a small cuff of tissue adjacent to the anterior attachment of the meniscus for later repair. This is most common for large OCD lesions of the lateral femoral condyle.
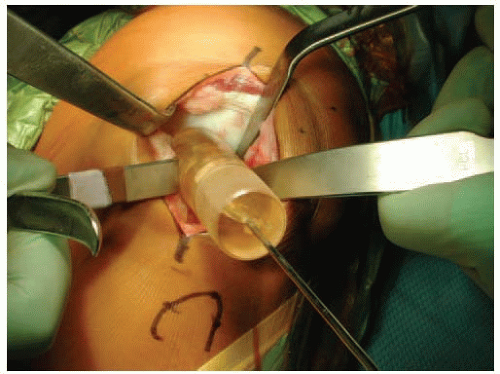
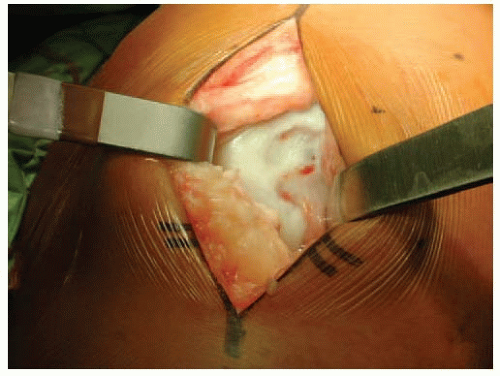 FIGURE 33-4 Miniarthrotomy with Z retractor and bent Hohman in notch, exposing the OCD lesion of the medial femoral condyle. |
Once the joint capsule and synovium have been incised and the joint has been entered, retractors are placed medially and laterally. Care is taken in the positioning of the retractor within the notch to protect the cruciate ligaments and the articular cartilage. This notch retractor is essential to adequate mobilization of the patella. The knee is then flexed and/or extended until the proper degree of flexion is noted that presents the lesion into the arthrotomy site (Fig. 33-4). Excessive degrees of flexion limit the ability to mobilize the patella. If access is difficult, extending the arthrotomy proximal is warranted. The lesion then is inspected and palpated with a probe to determine the extent, margins, and maximum size. After a size determination is made, a guidewire is driven into the center of the lesion, perpendicular to the curvature of the articular surface. It is critical to place the guidewire perpendicular to the joint surface. The size of the proposed graft is determined using sizing dowels (Fig. 33-5), the remaining articular cartilage is scored, and a coring drill is used to remove the remaining articular cartilage and 3 to 4 mm of subchondral bone (Figs. 33-6 and 33-7




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree