Allograft Cartilage Transplantation
Eric C. McCarty
R. David Rabalais
Kenneth G. Swan Jr.
Richard Williams
Brian C. Domby
DEFINITION
Articular cartilage lesions are focal, usually isolated, cartilage defects that may be either symptomatic or incidentally found.
Osteochondritis dissecans is an osteochondral lesion that occurs in adolescents and, therefore, may have different management ramifications from lesions in adults.
Lesions can be partial- or full-thickness, down to subchondral bone, or through subchondral bone.
Lesions can be secondary to trauma or atraumatic, as is the case for osteochondritis dissecans.
Cases with a traumatic etiology may have associated ligamentous or meniscal injury.
Small full-thickness chondral defects may heal adequately with mechanically inferior fibrocartilage (primarily type I collagen), but larger defects often require cartilage transplant surgery to replace the damaged chondral surface.
ANATOMY
Articular cartilage is composed primarily of type II collagen.
Chondrocytes that produce the extracellular matrix are of mesenchymal stem cell origin.
Osteochondral lesions may occur in all three compartments of the knee.
Chondral defects after a patellar dislocation typically are found on the medial patellar facet or lateral trochlea.
Classically, osteochondritis dissecans occurs at the lateral aspect of the medial femoral condyle.
PATHOGENESIS
Osteochondral lesions may be traumatic or may have no known history of trauma (osteonecrosis).
Traumatic lesions may be caused by compaction, as with an anterior cruciate ligament tear and lateral-based osteochondral injury, or by a shearing mechanism, as seen with patellar dislocations.
Atraumatic lesions may be found in young persons, as is the case with osteochondritis dissecans, or in elderly persons, as seen with degenerative lesions.
The etiology of osteochondritis dissecans is uncertain. Traumatic, inflammatory, developmental, and ischemic causes have all been proposed but not proven.
NATURAL HISTORY
Few controlled, prospective outcome studies have been published.
The natural history for juveniles with nondisplaced osteochondritis dissecans is very favorable.
Those diagnosed as adults have a less favorable prognosis. In a study by Linden and Malmo,9 81% of patients had tricompartmental gonarthrosis at an average of 33 years follow-up.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients with focal osteochondral lesions typically are active and young, ranging in age from adolescence to middle age.
Often, the history does not include a specific traumatic episode. History and physical findings can be subtle.
Presentation is variable; it may mimic meniscal pathology, with intermittent pain and swelling.
Condylar defects may present with high-impact loading complaints, whereas patellofemoral defects may produce anterior knee pain-type complaints, with stairs and prolonged sitting causing symptoms.
Patients with large cartilage lesions who are candidates for osteochondral allograft transplant surgery may have a history of previous knee surgery and previous attempts at cartilage regeneration by other methods (eg, microfracture, autologous chondrocyte implantation, osteochondral autograft transplant). Many have underlying bony changes or deficient subchondral bone.
Physical findings can be nonspecific and may include joint effusion and painful range of motion.
Tenderness at the defect, on either the condyle, patellar facets, or trochlea, may be elicited.
In the case of patellofemoral defects, patellar mobility and apprehension must be assessed.
Ligament integrity must be determined.
Mechanical alignment must be assessed, and appropriate imaging studies obtained.
Failure to identify and address ligamentous deficiency or mechanical malalignment will lead to compromise of restorative cartilage procedures.
Physical examination of the knee should note the following:
Chronic or recurrent effusion associated with, although not predictive of, a chondral lesion
Pain at extremes of range of motion (ie, forced flexion or forced extension) may indicate meniscal pathology. An extension block may indicate a displaced meniscus tear or loose body. Osteochondral defects may cause decreased flexion via effusion or may have normal range of motion.
An isolated lesion may have point tenderness, although it often is difficult to palpate.
Increased patellar mobility may indicate generalized ligamentous laxity, increasing suspicion for patellar instability.
Mechanical axis views should be obtained if there is any malalignment noted on gait and stance analysis.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Anteroposterior, lateral, and sunrise views are mandatory to determine overall knee condition, rule out diffuse degenerative arthritis, and assess patellar position within the trochlea.
Large chondral defects may not be visible on plain radiographs or may have a small radiodense bone fragment attached.
“Notch views” may better define more central lesions.
Long-leg mechanical axis views are mandatory in patients with malalignment on physical examination and should be considered in all candidates for osteochondral autograft transfer.
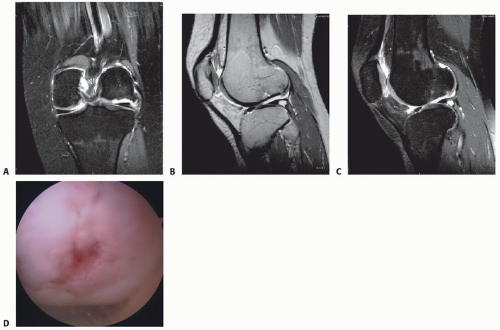
MRI is the best modality to determine the presence, size, and location of cartilage lesions, as well as to determine the integrity of menisci and ligaments. It will also offer information about the supporting bone surrounding the lesion (FIG 1A-C).
Arthroscopy remains the gold standard for evaluation of articular cartilage lesions (FIG 1D).
DIFFERENTIAL DIAGNOSIS
Meniscal tear
Degenerative arthritis
Patellar instability
Bone contusion
Avascular necrosis
Undiagnosed ligamentous injury
NONOPERATIVE MANAGEMENT
Patients with asymptomatic osteochondral lesions (often found incidentally on standard knee arthroscopy) may be candidates for nonoperative treatment.
Long-term studies may indicate an increased risk for degenerative arthritis with conservative management,9 but no randomized controlled studies exist.
Nonoperative treatment should consist of physical therapy to obtain or maintain painless, full range of motion.
Aggravating impact activities should be avoided.
Patients may participate in sports as tolerated.
Unloader braces or shoe wedges may help alleviate mild symptoms.
SURGICAL MANAGEMENT
Osteochondral allograft transplantation often is a two-stage procedure.
The magnitude of the lesion and, occasionally, the diagnosis itself often are not appreciated until first-look arthroscopy (FIG 2).
Size and location of the cartilage lesion is determined.
Lesions 1 cm (>2 cm2) in diameter or larger are considered for allograft transplant. Smaller lesions may be amenable to microfracture or autograft cartilage transplant with single or
multiple plugs. (Lesions with deficient subchondral bone are also considered for allograft transplant.)
The remainder of the knee is inspected to ensure this is not a diffuse cartilage process and to examine the integrity of the cruciate ligaments and menisci.
Preoperative Planning
Mechanical alignment must be assessed and, if necessary, osteotomy planned for.
Templated radiographs are obtained for appropriate allograft sizing based on the medial-lateral dimension of the lesion.
The patient must be informed that there is no way to predict when an appropriate-sized donor will become available and that a moderate waiting period (weeks to months) may be required before surgery can be done.
Fresh osteochondral allografts are used. Frozen chondral grafts are associated with poor chondrocyte viability and are unacceptable.
Allografts are harvested within 24 hours of donor death.
Because of concerns of disease transmission, tissue is now stored at 4° C for a minimum of 14 days and maximum of 28 days to allow for bacterial cultures and viral testing to be analyzed13 preserved for up to 4 days at 4° C.
Chondrocyte viability likely declines after 14 days6 and allografts generally should be implanted by 28 days.11,15,14
After 28 days, chondrocyte viability significantly declines.6
Tissue matching and immunologic suppression are unnecessary with osteochondral grafts.
Donors are screened with a multifactorial process promoted by the American Association of Tissue Banks to minimize the risk of disease transmission. The allograft is tested for hepatitis B virus (HBV), hepatitis C virus (HCV), HIV, and syphilis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree