Is Advanced Imaging Necessary Before Surgical Repair
John M. Baca, DPMa∗jbaca@wpahs.org, Colin Zdenek, DPMa, Alan R. Catanzariti, DPMa and Robert W. Mendicino, DPMbc, aDivision of Foot & Ankle Surgery, West Penn Hospital, 4800 Friendship Avenue, Pittsburgh, PA 15224, USA; bDepartment of Orthopoedics, OhioHealth Orthopedic Surgeons, 4343 All Seasons Drive, Suite 140, Hilliard, OH 43026, USA; cFoot & Ankle Surgical Residency, West Penn Hospital, 4800 Friendship Avenue, Pittsburgh, PA 15224, USA
Posterior tibial tendon dysfunction (tendinitis, tendinosis, or rupture) and adult acquired flatfoot deformity can manifest with a wide array of bony and soft tissue abnormalities visible on plain radiographs, ultrasound, and magnetic resonance imaging. Imaging abnormalities include various combinations of malalignment, anatomic variants, and enthesopathic and tendinopathic changes. A thorough understanding of differences between anatomic and pathologic presentations of structures in various imaging modalities is an essential tool for clinical and surgical planning.
Key points
Posterior tibial tendon (PTT) dysfunction (tendinitis, tendinosis, or rupture) and adult acquired flatfoot deformity can manifest with a wide array of bony and soft tissue abnormalities visible on plain radiographs, ultrasound, and magnetic resonance imaging (MRI). Imaging abnormalities include various combinations of malalignment, anatomic variants, and enthesopathic and tendinopathic changes.1–3 A thorough understanding of differences between anatomic and pathologic presentations of structures in various imaging modalities is an essential tool for clinical and surgical planning.
Plain radiographs
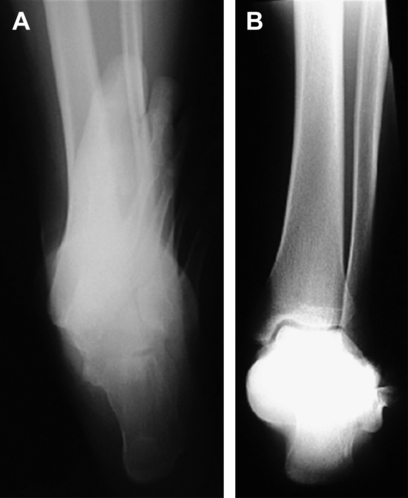
Abnormal bony position observed with plain radiographs may give clues to longstanding insufficiency of the PTT. Malalignment and angular deformity on radiographs often correlate to soft tissue abnormalities identified on ultrasound and MRI.1 Three weight-bearing views (lateral, anteroposterior, medial oblique) of the foot are generally necessary to evaluate for signs of PTT dysfunction. Ankle views are necessary to evaluate for valgus deformity, especially with advanced deformity (Fig. 1). Additional hindfoot alignment views (calcaneal axial, long-leg axial) may be beneficial to ascertain the frontal plane relationship of the tibia, talus, and calcaneus (Fig. 2).
Flattening of the plantar arch on a lateral weight-bearing view may be observed through evaluating the calcaneal inclination angle. Although variation normally ranges from 11° to 38°, it is considered low when it is less than 20°.4,5 Attenuation and weakness of the surrounding supporting soft tissue structures may lead to increased talar declination of the long axis of the talus below the long axis of the navicular. Talar declination, normally 21°(±4°), is measured using the lateral talar axis and the weight-bearing surface.1,4
Secondary to the unopposed force of the peroneal tendons, mainly the peroneus brevis, hindfoot valgus and forefoot abduction may be appreciated.5 Greater than a 6° angulation of the long axis of the calcaneus away from midline relative to the long axis of the tibia in the frontal plane defines hindfoot valgus.4,6 Uncovering of the head of the talus as the navicular moves away from midline in the transverse plane is the result of forefoot abduction. Talar head uncovering is considered abnormal if more than 15% of the head is exposed.6
Hypertrophic change and bony irregularity may also be noted at the navicular attachment of the PTT, which suggests enthesopathy.1 Another sign of posterior tibialis tendinopathy is a tibial spur, which may be visible adjacent to the tendon in the retromalleolar groove.1,6 Congenital navicular abnormalities may also predispose patients to tendinopathy. A true accessory navicular is present in approximatley 4% of the population7; however, accessory naviculars are present in a much higher percentage of patients with posterior tibialis tendon disorders.8 Accessory navicular variants (types 2 and 3) are visible on MRI similar to plain radiographs.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree