Flexible Adult Flatfoot
Soft Tissue Procedures
Jeremy L. Walters, DPM∗jeremylwalters@gmail.com and Samuel S. Mendicino, DPM, West Houston Medical and Surgical Residency Program PMSR/RRA, West Houston Medical Center, 12121 Richmond Avenue, Suite 417, Houston, TX 77082, USA
Classically, adult posterior tibial tendon dysfunction (PTTD) was considered primarily a tendon rupture and was treated as such with soft tissue repair alone. The understanding that PTTD involves more than simply an inflammatory condition or tendon rupture but also a muscle imbalance, leading to a flatfoot, osteoarthritis, and peritalar subluxation, led to surgeons advocating osseous procedures as well. The advancements in knowledge of the pathomechanics of the deformity have modified the role that soft tissue repair plays in surgical treatment, but the importance of soft tissue restoration in flatfoot repair should not be overlooked.
PT tendon tenolysis and augmentation
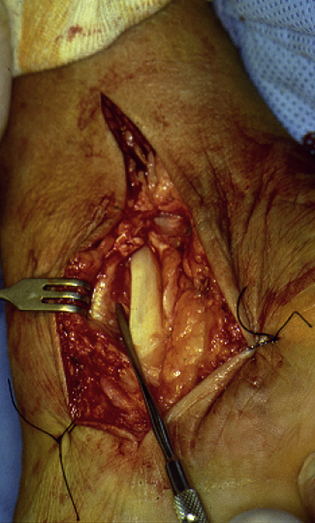
Originally, this condition was considered primarily a tendon rupture, and the same principles were applied to PTTD that were used for other tendon injuries. Tenolysis with synovectomy may be helpful in patients with pain and swelling of the PT tendon who fail to respond to conservative and nonoperative management and have not experienced an acute rupture or tear (Fig. 1).1–3 Teasdall and Johnson1 reported 74% success with a 30-month follow-up but believed debridement alone should be reserved for patients without a progressive deformity. Funk and colleagues4 looked at tenosynovectomy with and without repair of a split tendon tear and found 89% of patients with absent or minor pain.
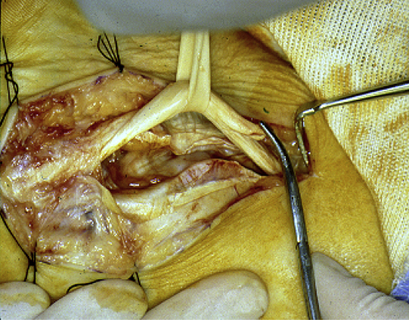
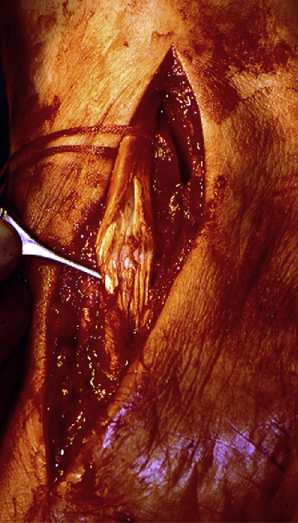
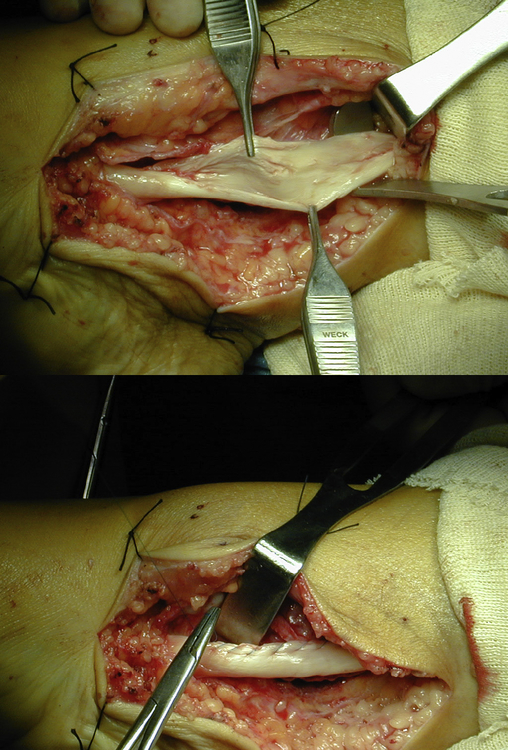
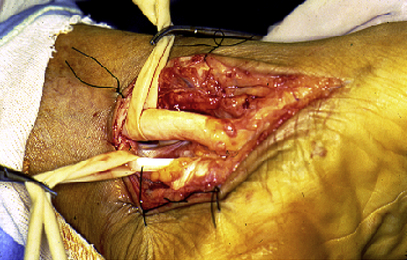
For the patient with an acute midsubstance rupture, primary repair with or without soft tissue support should be considered (Fig. 2).5 In the longitudinal tear with minimal lengthening or weakness, tendon debulking with entubulation may be performed (Fig. 3). This treatment may be further supported by tendon augmentation, transfer, or the use of orthobiological substitutes (Fig. 4).
Flexor digitorum longus transfer
Flexor digitorum longus (FDL) tendon transfer has long been advocated in the treatment of Johnson and Strom stage 2 adult flatfoot deformity and is performed after primary tendon repair.6–10 For an FDL transfer to be the most effective, or functional, 2 important patient characteristics need to exist. First, a flexible deformity must be present. The FDL tendon cannot overcome a fixed hindfoot valgus if less than 15° of subtalar inversion is present. Second, a patient needs to show a minimum adduction to lock the midtarsal joint, thus permitting heel raise. The choice of FDL as the tendon transfer for PTTD is logical for many reasons. The FDL originates from the posterior tibia adjacent to the PT tendon, without any vital neurovascular structures from the flexor retinaculum to the navicular tuberosity (Fig. 5). The FDL also constitutes an in-phase transfer, which is always preferable in tendon transfers.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree