Fig. 11.1
Positive Matles’ sign of the near Achilles tendon confirming rupture as represented by the inability of the foot to stay passively plantarflexed
11.1 Surgical Treatment of Acute Achilles Tendon Ruptures
The acutely ruptured Achilles can be repaired by open, “mini-open,” and percutaneous techniques. Research has shown that open repair has lower incidence of re-rupture but greater wound complications. Predominantly, a medial longitudinal approach for an open procedure is utilized. The surgery is performed with the patient in the prone position and can be performed without a tourniquet and with local anesthesia or regional block. The frayed tendons’ ends are debrided (Fig. 11.2). Krackow suture technique on both ruptured ends is used to re-approximate the ruptured Achilles tendon with the foot maintained in a plantarflexed position generally with #2 suture (Fig. 11.3).1 Additional reinforcement can be performed with smaller gauge suture such as 2–0, and subcutaneous tissues are closed in layers, avoiding tension over the tendon and skin (Fig. 11.4). Both open and percutaneous techniques can be performed with absorbable or nonabsorbable sutures, with the former more prevalent in Europe and the latter more common in North America. Granuloma and suture reaction can occur regardless of suture material.5 Percutaneous and “mini-open” techniques may be beneficial in females and those with history of keloid formation.3,4 The re-rupture incidence and nerve entrapment occurrence are higher with these techniques as compared to open repair. Maffulli et al. modified the traditional percutaneous technique to avoid sural nerve entrapment. They biased the proximal percutaneous incisions more medially (Fig. 11.5).4 Gaps larger than 5 cm that cannot be bridged by turn-down flaps or gastrocnemius recession may need to be addressed by flexor tendon (usually FHL) or peroneus brevis transfer, the latter of which may be better in athletic patients though not yet critically studied.4,5 Postoperatively, the ruptured Achilles tendon is protected by a below-knee cast/boot, or an anterior splint to prevent dorsiflexion, with the foot in equinus, and kept non-weight-bearing for approximately 2 weeks. Randomized study comparing non-weight-bearing of 1 week versus 3 weeks showed no difference.2 Progression to weight-bearing occurs with gradual reduction of equinus over the next several weeks, often in a boot with heel wedges that can be gradually decreased. Physical therapy consists of progressive strengthening (initially with surgical tubing and/or a towel at 3 weeks) including single-legged heel raises. A heel cushion (6-mm heel lift) may be maintained (bilaterally) for 6 or more months post-op. Return to daily activities takes at least 8–12 weeks with return to sports occurring at 12–26 weeks. A detailed physical therapy regimen is found in Chap. 18 [Rehabilitation].
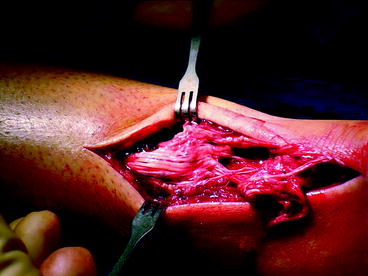

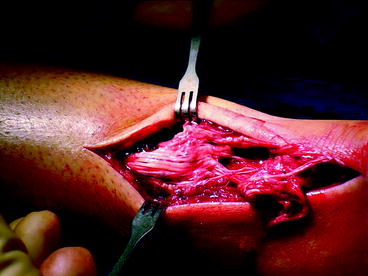
Fig. 11.2
Achilles tendon rupture
Fig. 11.3
Krackow suture technique
Fig. 11.4
(a) Repaired tendon. (b) Skin suture

Fig. 11.5
Modified percutaneous Achilles tendon repair incisions as described by Carmont and Maffulli4
11.2 Miscellaneous Foot and Ankle Tendon Ruptures
Other ankle tendon ruptures such as with peroneal tendons can occur acutely particularly with inversion ankle injuries in sports.6–12 These are discussed in detail, elsewhere in this text, as well as surgical treatment of chronic Achilles tendinopathy. Acute tendon ruptures of the anterior and posterior tibial tendons, though somewhat rare in sports, are often dealt with surgically. This usually involves primary repair, generally using suture anchors for avulsion type injuries. Though tibialis anterior ruptures with significant gapping, it can be repaired with transfer of extensor hallucis longus (EHL) (and tenodesis of the distal stump to the extensor hallucis brevis [EHB]); loss of dorsiflexion strength may be an issue in athletes. A free graft of “doubled” EHB (first extensor tendon of extensor digitorum brevis) can be used to bridge the defect (Figs. 11.6 and 11.7). Similarly, transfer of flexor digitorum longus (FDL) for posterior tibial tendon tears may not be ideal in athletic patients, and direct repair should be attempted when possible.