I. INTRODUCTION. Spine trauma needs to be understood in the context of the overall care of the patient. It is often present in the polytraumatized patient, complicating their hospital care as well as resulting in worsened outcomes at all stages.
A. Initial evaluation and management. Optimal outcome following acute spinal injury depends on early recognition of injury and appropriate management to prevent further injury. Adherence to principles of advanced trauma life support (ATLS) makes it mandatory that all patients with a mechanism of injury compatible with spinal injury should be assumed to have a spinal cord injury until proven otherwise. Any history of loss of consciousness or presenting complaints of numbness, tingling, or weakness should alert the practitioner to the presence of a possible spinal cord injury. Additionally complaints of pain along a radicular dermatome or any bilateral pain or weakness should be clues to the possibility of a spinal cord injury. Brachial plexus injury or other peripheral nerve injuries should be considered diagnoses of exclusion in the setting of trauma. A detailed physical examination is required and includes cranial nerve function including swallowing and phonation where possible. Manual motor testing of the upper and lower extremities, sensory testing of the upper and lower extremities, reflex testing including the documentation of presence or absence of pathologic reflexes including Hoffmann and Babinski. Although a great deal of information may be established from a gait examination, it will be a rare instance where it will be useful in the acute trauma setting. In the neurologic examination, a detailed rectal examination is critical in defining the patient’s neurologic status to include the presence or absence of rectal tone as well as peri-anal sensation. Finally a detailed physical examination will require inspection and palpation of the entire spinal column looking for open wounds or ecchymosis, as well as palpations of any step-offs or deformities. A careful physical examination can identify ligamentous disruption in the spine, particularly in patients who may not be able to have an MRI for more detailed imaging.
B. Imaging studies
- Radiographs
a. Standard radiographic evaluation of the cervical spine includes the lateral, open-mouth odontoid, and anterior–posterior plain radiographs. Lateral view will detect up to 85% of significant cervical spine injuries provided that the occipitocervical and cervicothoracic junctions are visualized. Missed fractures at the cervicothoracic junction may occur despite apparently normal lateral radiograph.1 Orthogonal oblique views do not increase the sensitivity of plain film evaluation and add radiation exposure and cost to the examination. Anterior–posterior and lateral radiographs of the thoracic and lumbar segments are indicated as screening films in the presence of pain or abnormal physical examination findings in these regions and in cognitively impaired patients who cannot cooperate in physical examination, including obtunded patients. Noncontinuous spinal trauma is common with incidence rates up to 19% reported,2 and the presence of an injury anywhere in the spine should prompt radiographic evaluation of the entire spine.
b. Important points to consider in interpreting plain radiographs include the following:
- Any alteration in the alignment of the vertebral bodies. Straightening of the cervical spine can result from muscle spasms or from positioning the patient’s head in slight flexion.
- Any step-off in the line of the posterior intervertebral facet joints.
- Any increase in the width of the retropharyngeal space in front of the vertebral bodies (normal is 4 to 6 mm at C3 and 15 to 20 mm at C6). This rule does not apply in a crying child.
- Any fracture lines in the bodies or in the posterior elements.
- Any increase of distance between two spinous processes.
- Any displacement of the spinous process on the cephalad side, which is toward the side of any unilateral dislocation on the anteroposterior film.
- Any indication that the body of one vertebra has moved forward in relation to another on the lateral roentgenogram because such movement usually indicates a dislocation or fracture–dislocation of one or both joint facets at that level. If the amount of displacement is more than half the width of the vertebral body, the dislocation is bilateral and the spine is extremely unstable.
2. CT scanning can provide rapid and detailed assessment of the spine. This should include high-resolution imaging (2- to 3-mm collimation and 1.5-mm pitch) from the occiput to T1 with sagittal and coronal reconstructions. Several studies have demonstrated high levels of sensitivity (90%) and specificity (100%) of screening CT scanning in polytrauma patients.3–5 CT scan represents an evolving standard of care in the evaluation of cervical spine and cervicothoracic junction injuries for cervical injuries,6,7 CT scanning represents the standard of care in all patients when
a. Poorly visualized areas are encountered on plain films.
b. Visualization of T1 is not improved with gentle downward traction on the arms, swimmer’s views, or oblique views.
c. Fractures or dislocations are identified elsewhere in the spine.
d. In patients who are intubated, as plain films will miss up to 17% of injuries to the upper cervical spine in the presence of an endotracheal tube.
3. Magnetic resonance imaging (MRI) is less sensitive, less specific, and less cost effective than the plain film series or screening CT for the identification and evaluation of cervical fracture.8 However, MRI is extremely sensitive and specific for the evaluation of the paravertebral soft tissues, including the spinal cord, intervertebral discs, and ligamentous structures.9 With the use of MRI increasing, the incidence of identifying noncontiguous fractures has increased to 41% versus the standard reported 10-15%. Patients with abnormal neurologic findings, particularly incomplete injuries, should undergo MRI scanning of the relevant spinal segment(s) to visualize the spinal cord and nerve roots.
4. Dynamic fluoroscopy. Passive flexion and extension stressing of the cervical spine, performed by an experienced physician under fluoroscopy, has a reported sensitivity of 92.3% and specificity of 98.8% for detecting significant ligamentous injuries and instability of the cervical spine.10 Although some centers support the use of this technique in clearing the spine of unconscious patients, the risk of neurologic deterioration may outweigh its benefits, especially given the widespread availability of CT and MRI imaging.10
C. Clearance of spine in trauma patients. Although protection of the spine is mandatory at all stages of managing the traumatized patient, clearance of the spine should take place only after potential life-threatening injuries have been stabilized.
- In the cognitively intact patient who is not under the effect of drugs or alcohol and who is cooperative, clinical clearance of the spine may be possible. While case reports of bony and ligamentous spinal injuries in such patients do exist, unstable spinal injuries and neurologic deterioration in these patients have not been reported. Accordingly routine radiographic evaluation in such cases is not indicated. However, the physical examination findings of neck or back pain, neurologic abnormalities, bruising, spinal deformity, pain with active range of motion or significant distracting nonspinal injuries should prompt further investigation.11
- Obtunded or uncooperative patients as well as alert patients with physical examination findings consistent with spinal injury should be maintained on spinal precautions until thorough clinical and radiographic evaluation of the spine has been completed, which should occur in a fairly rapid fashion. A prospective study of consecutive blunt trauma patients admitted to a single institution demonstrated 99.75% sensitivity for CT scan in its ability to clear clinically significant cervical spine injuries. Although the recommendation is that CT be used as a sole modality to radiographically clear the cervical spine in obtunded trauma patients, there is separate clinical evidence to suggest that the spondylotic cervical spine may present a specific clinical category where CT scanning is unreliable in determining stability and will miss clinically significant injuries. In the obtunded or unreliable patient, CT scan has a negative predictive value up to 90.9% for ligamentous injury and a negative predictive value of 100% for instability in the nonspondylotic patient.7
- In a prospective cohort study comparing the Canadian C-spine rule versus the Nexus low-risk criteria in patients with trauma, the sensitivity and specificity of CCR were at 99.4% and 40.4%, respectively. The CCR mandates that any patient with a high-risk factor, including age greater than 65, in trauma or dangerous mechanism, or complaints of paresthesias in extremities will proceed to imaging studies. Any patient without a high-risk factor that instead has a low-risk factor allowing for safe assessment of range of motion including simple rear-end motor vehicle collision, or sitting position in the Emergency Department, or ambulatory at any time, or delayed onset of neck pain, or absence of midline cervical spine tenderness may proceed to range of motion examination including the ability to rotate the neck actively 45° to the left and to the right, which would indicate a cleared cervical spine in the awake, alert, and cooperative patient.
D. Fracture stability. Stability as described by White and Panjabi12 refers to the spine’s ability to maintain patterns of displacement and movement under normal physiologic loads without incapacitating pain, progressive deformity, or increasing neurologic deficit. The isolated but unstable spine fracture at the spinal cord level results in complicated management throughout the patient’s hospital and posthospital course. Stable fractures are important to recognize in that they are often a marker for other injuries, particularly intrathoracic or intraabdominal injury.
- Acute spinal instability most directly impacts the spine’s ability to protect neural elements including spinal nerves and the spinal cord from further injury, and may be clinically manifested as neurologic deficit or severe intractable pain.
- Glacial instability represents the spine’s tendency to deform over time and is manifested by clinical deformity as well as progressive debilitating pain.
a. Osteoporosis is an underlying medical condition that may result in glacial instability in an otherwise apparently stable fracture pattern.
3. Radiographic and anatomic features. Determination of instability varies with the injured spinal segments with the occipitocervical junction having different characteristics radiographically and anatomically indicating instability when compared with the subaxial cervical spine, the cervicothoracic junction, the thoracic spine, the thoracolumbar junction, the lumbar spine, and the lumbosacral spine. Each region has unique characteristics and will be discussed as a separate section. Additionally the spinal cord represents a distinct entity within the spine with unique injury characteristics and will be discussed as a separate section of the spine.
II. FRACTURES, DISLOCATIONS, AND FRACTURE–DISLOCATIONS
A. Craniocervical junction. The craniocervical junction, or occipitocervical junction, represents a unique combination of osteologic and ligamentous structures allowing a tremendous range of motion in flexion and extension at the occipital condyles and C1, with a tremendous range of rotation at the junction of C1 and C2, and a transition zone between the unconstrained motion at the occipital to C2 levels and the more constrained subaxial cervical spine occurring osteologically through C2.
- Craniocervical junction injury patterns.
a. Craniocervical dislocation. Craniocervical dislocations or occipitocervical dislocations represent a loss of ligamentous integrity between the occiput, C1, and C2. This is best identified by the Harris lines13,14 with a measurement of greater than 14 mm indicating a craniocervical dislocation.* The key feature in understanding these injuries is that the ligamentous constraints linking the occiput to C2 are destroyed in this injury pattern, resulting in global instability. The exact displacement of the skull relative to the Dens may be quite fluid and variable depending on the time imaging is obtained. Prior work classifying the dislocation pattern based on location of the occiput relative to C2 is not useful for determining either prognosis of injury or treatment modalities as any of the displacement patterns represents global instability. The basion to the tip of the dens interval is less than 12 mm in 95% of patients. Greater than 12 mm is considered abnormal. The basion-axial interval is the basion to the posterior dens and is between 4 and 12 mm in 98% of patients. Greater than 12 mm indicates anterior subluxation; less than 4 mm is a posterior subluxation.
- Clinical features. Wallenberg syndrome is lower cranial deficits (Fig. 12-1). Horner syndrome, cerebellar ataxia. Bell cruciate paralysis and contralateral loss of pain and temperature.15,16

Figure 12-1. Right cranial nerve VI palsy. From Tasman W, Jaeger E. The Wills Eye Hospital Atlas of Clinical Ophthalmology, 2e. Philadelphia, PA: Lippincott Williams & Wilkins; 2001, with permission.
ii. Additional imaging studies. CT angiogram to evaluate the vertebral artery given the relative tethering of the vertebral artery around the craniocervical junction is indicated. An MRI including the brain stem and cervical spine is necessary to evaluate for any concurrent cord or brain stem injury as well as for the presence of traumatic dural tear.
iii. Acute management. Sandbag placement around the head with consideration of halo vest placement, as well as airway control to include early elective intubation. Often these injuries are so severe that the patient will present with intubation from the field, but if this has not occurred retropharyngeal swelling can predictably become so severe as to require emergent intubation, which would be associated with a high mortality rate.
iv. Operative intervention. In a patient who is otherwise medically stable, the standard of care should be considered and an occiput to C2 posterior instrumented spinal fusion would include. Upright radiographs should be obtained before discharge.
v. Morbidity and mortality. Cranial-cervical dislocations in general have historically been associated with a greater than 50% mortality rate, although the promulgation of ATLS techniques and broader penetration of advanced emergency medical services may be contributing to an increased survival of these injuries. Additionally this injury pattern can represent a spectrum as described by Bellabarba et al.,15 with a craniocervical sprain representing a less severe form of this injury.
2. Occipital condyle fractures
a. Type I represents an impaction fracture with bilateral impaction fractures representing an axially unstable fracture pattern.
b. Type II is an extension of basilar skull fracture and is typically a stable injury.
c. Type III represents an alar ligament avulsion and is potentially highly unstable.17,18 A 50% missed injury rate is associated with craniocervical dislocations with one-third of these having neurologic worsening while in the hospital.15,19
3. C1 ring injuries
a. Atlas fractures. Fractures of the atlas include relatively trivial fractures such as posterior ring fractures associated with hyperextension injuries, as well as unstable injury patterns such as the burst fracture or “Jefferson” fracture (Figs. 12-2 and 12-3), as well as the lateral mass fracture separation.
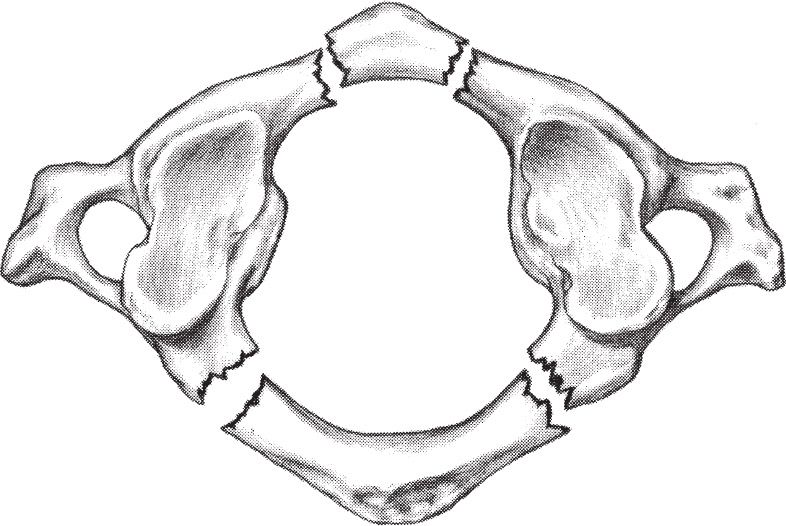
Figure 12-2. Jefferson fracture.
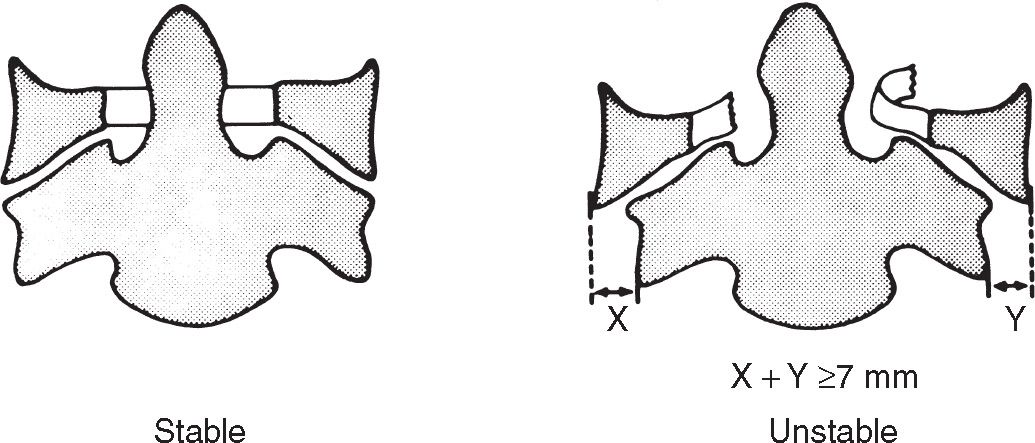
Figure 12-3. Jefferson fractures. When a comminuted fracture of C1 shows bilateral overhang of the lateral masses that total 7 mm or more, rupture of the transverse ligament has probably occurred, rendering the spine unstable. From White AA III, Panjabi MM. Clinical Biomechanics of the Spine. Philadelphia, PA: JB Lippincott; 1978:203, with permission.
- Imaging. The key imaging study for assessing the C1 ring injuries is the open-mouth odontoid view that may be approximated with the coronal plane reconstruction of a thin-cut CT scan. This is used to assess the integrity of the transverse atlantal ligament, which is a key stabilizer of this level. Separation of the lateral masses of greater than 6.9 mm is an indicator of rupture of the transverse atlantal ligament and an unstable fracture pattern. Additionally the vertebral artery is at risk for injury, and a CT angiogram is an important study to obtain in order to evaluate any acute injury. Late instability at this level, if left untreated, will put the patient at risk for a thrombotic cerebrovascular accident.
- Treatment. Acute management of these injuries consists of reduction, typically in a halo vest, and operative stabilization of unstable injuries. Nondisplaced fractures may be treated in a cervical collar or a halo as long as close follow-up is obtained. Although fracture union may be achieved with nonoperative means, there can be resultant atlantoaxial instability that will put the patient at risk for late neurologic deterioration. A fracture separation of the lateral mass will result in progressive torticollis if left untreated. Upright radiographs should be obtained before discharge.
a. Odontoid. The most common fracture of the second cervical vertebra is a fracture of the odontoid. This column of bone is necessary for rotation at the craniocervical junction. The appropriate mechanics of C1 and C2 are primarily ligamentous restraints including the transverse atlantal ligament as well as the apical ligaments and an expanse of the posterior longitudinal ligament, which, when combined, make the cruciate ligaments across the dorsal portion of the dens. Additionally the tectorial membrane, a continuing expanse of the posterior longitudinal ligament, provides stability between the occiput and C2.
- Fracture classification (Fig. 12-4).
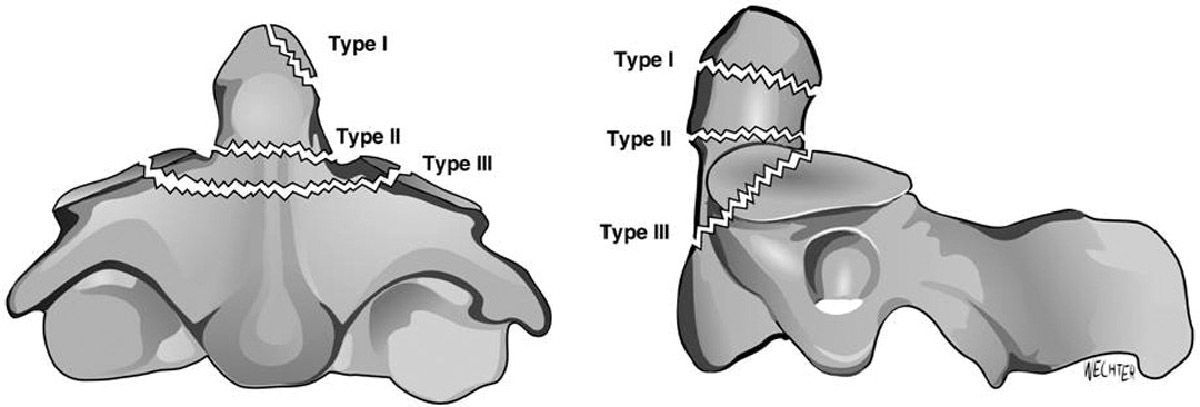
Figure 12-4. Odontoid fractures shown in AP and lateral views. Type I is an oblique fracture through the upper part of the odontoid caused by alar ligament avulsion. Type II is through the base of the odontoid. Type III is through the upper portion of the vertebral body.
- Type I odontoid fracture involves the attachment of the apical ligament and represents a potentially unstable craniocervical junction injury. Most commonly this is actually a nonfused ossicle and an incidental finding. In the acute trauma setting, an occult craniocervical junction injury must be ruled out.
- Type II odontoid fracture typically involves the midportion of the odontoid and may be subdivided into Type IIA, IIB, and IIC,20 with ramifications for operative intervention.* The hallmark of the Type II odontoid fracture is that it is at high risk for nonunion. The significance of this nonunion needs to be considered in management planning. Low-energy odontoid fractures, typically encountered in the elderly with minor trauma, may be quite tolerant of a nonunion that is otherwise stable in flexion and extension and does not cause debilitating pain. A stable pseudarthrosis is the common result of nonoperative management of these fractures in this patient population. Given the relatively high risk of perioperative mortality and perioperative morbidity in the elderly patient with an odontoid fracture, a stable pseudarthrosis may be considered a good end result of treatment. Unstable fractures that result in debilitating pain, progressive deformity, or neurologic deficit, or risk for progressive neurologic deficit, are best treated operatively regardless of patient’s age or comorbidities. These injury patterns are often associated with upper cervical cord injuries and also have the potential for vertebral artery injury, and so MRI as well as CT angiography is indicated. Upright radiographs should be obtained before discharge.
b. Traumatic spondylolisthesis (Fig. 12-5) of the axis (Hangman fracture). Mechanically this represents a separation of the posterior ring from the vertebral body of C2, typically occurring through the pars that represents a transition zone at C2 from the craniocervical junction to the subaxial cervical spine.
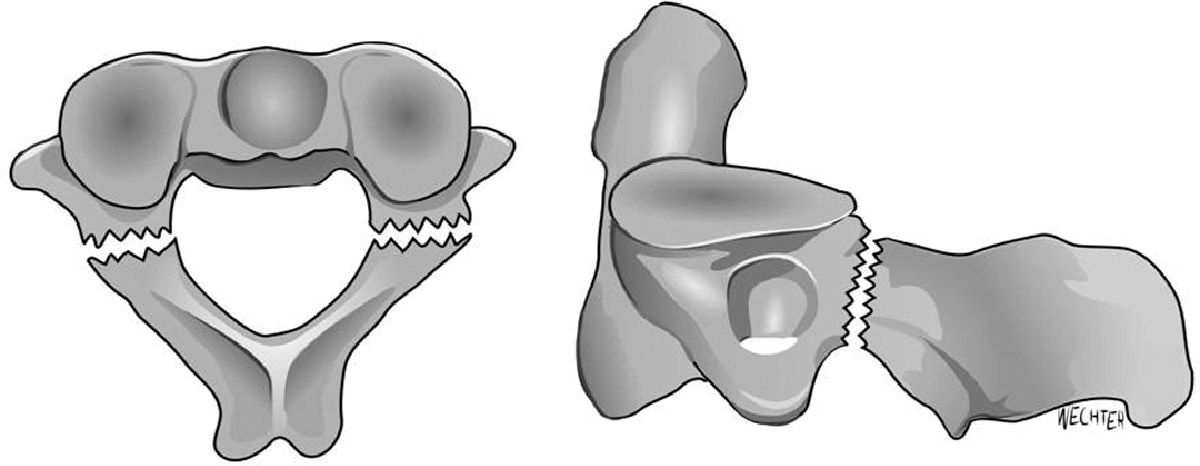
Figure 12-5. Effendi Type I fracture. From Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am. 1985;67:217–226, with permission.
- Type I fractures through the pars are uncommonly associated with spinal cord injury and typically may be treated in a closed fashion with a cervical collar or halo thoracic brace.
- Type II fractures that involve a portion of the body of C2 are more commonly associated with spinal cord injury due to the translation of the partially intact ring across the spinal canal. This injury commonly may also be treated in a closed fashion. It should be noted that the status of the C2-3 disc is critical in determining appropriate treatment modality as the Type IIA fracture will tend to displace in traction because of the torn posterior longitudinal ligament and posterior disc.
- Type III injury will be grossly unstable in traction.
B. Subaxial cervical spine. The subaxial cervical spine begins at the C2-3 articulations and extends down to the cervicothoracic junction that is essentially the rostral aspect of C7.
- Classification.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








