Chapter 19
Isai Gopalakrishnan Bowline MD amd Akhtar Ashfaq MD
Case:
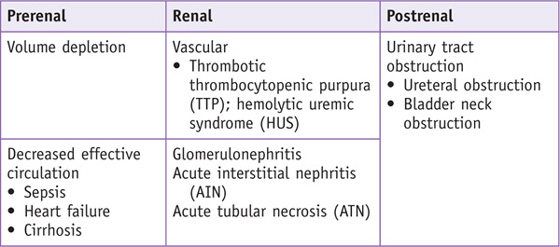
Differential Diagnosis
Speaking Intelligently
• Evaluate AKI with a systematic approach to reverse any potential causes, minimize any further injury, and initiate appropriate therapy.
• Determine whether the elevated serum creatinine is due to an acute insult or whether the creatinine is chronically elevated; our patients are often unaware of any previous disease, and it is helpful to look at their past creatinine values.
• Classify the patient based on urine output.
• Anuria is defined as a urine output less than 100 mL/day; anuria is rare and suggests complete obstruction, ATN, or a vascular event.
• Oliguria is defined as urine output less than 400 mL/day; oliguria is commonly seen with AKI, and patients with oliguria should be evaluated closely because fluid overload and electrolyte abnormalities can occur rapidly.
• When evaluating for prerenal azotemia, it is important to inquire about volume loss.
• Has the patient had any diarrhea, vomiting, or burns, or is he or she taking diuretics?
• Hypovolemia can cause profound renal failure especially in the setting of certain medications (nonsteroidal anti-inflammatory drugs [NSAIDs], angiotensin-converting enzyme [ACE] inhibitors or angiotensin II receptor blockers [ARBs]) and conditions (renal artery stenosis) that limit the kidneys’ ability to compensate for hypovolemia.
• Evaluate for any signs of infection that may also result in hypovolemia. Has the patient had any cough, congestion, diarrhea, dysuria, fevers, or chills?
• Review the patient’s medical history for any cardiac conditions that may reduce cardiac output and forward flow to the kidneys.
• Inquire about liver disease, which may result in decreased renal perfusion as a consequence of arterial vasodilation in the splanchnic circulation.
• Eliminating postrenal etiologies involves assessing urine output.
• Ask the patient about urgency, hesitancy, incontinence, and frequency of urination; each of these can be a symptom of incomplete bladder emptying.
• Inquire about hematuria; gross hematuria can be a sign of stone disease or malignancy, and blood clots can lead to obstruction.
• Review medications for use of anticholinergic medications that may cause urinary retention.
• Consider etiologies that precipitate intrinsic renal disease.
• Review the patient’s medical history for systemic diseases that affect the kidney, such as systemic lupus erythematosus (SLE), diabetes, hypertension, HIV infection, or hepatitis C.
• Inquire about recent trauma, which can precipitate rhabdomyolysis.
• Consider atheroembolic disease in patients with recent endovascular procedures.
• Inquire about symptoms of fever, rash, and arthralgias to support the diagnosis of interstitial nephritis.
• Review medications that may potentially cause ATN, such as the aminoglycosides.
• Physical assessment of volume status is very important in evaluating the cause of AKI.
• Vital signs are crucial; look for hypotension and tachycardia to support the diagnosis of prerenal azotemia.
• Central venous pressure (CVP) tracings and wedge pressures can give a more definitive assessment of volume status.
• Dry mucous membranes and hyperthermia support hypovolemia as a diagnosis.
• Distended neck veins, S3 gallop, bibasilar crackles, and edema support the diagnosis of heart failure with resultant renal hypoperfusion.
• Stigmata of cirrhosis may support the diagnosis of hepatorenal syndrome. Periorbital, sacral, and lower extremity edema can be signs of glomerular diseases.
• Examine the skin thoroughly to evaluate for any rash that may hint at an allergic interstitial nephritis.
• Blue toes with palpable pulses and livedo reticularis support the diagnosis of atheroembolic disease.
• Be mindful of physical exam findings associated with the systemic diseases that have renal manifestations, such as the malar rash of SLE. A palpable bladder, enlarged prostate, or palpable pelvic masses are suggestive of obstruction.
Only gold members can continue reading.
Log In or
Register to continue
Related
Stay updated, free articles. Join our Telegram channel
Join