Acetabular Fractures: The Kocher-Langenbeck Approach
Berton R. Moed
Indications/Contraindications
Displaced fractures of the acetabulum resulting in joint incongruity or instability are best treated by open reduction and internal fixation (ORIF). Contraindications to surgery are ill defined and not absolute. Important concerns include preexisting patient factors, such as poor general medical status and osteopenia, and factors that relate to overall patient prognosis, such as advanced age and associated injuries. All of these conditions must be considered with the knowledge that with nonoperative treatment in the face of joint incongruity or instability or both, the prognosis for hip-joint function is poor.
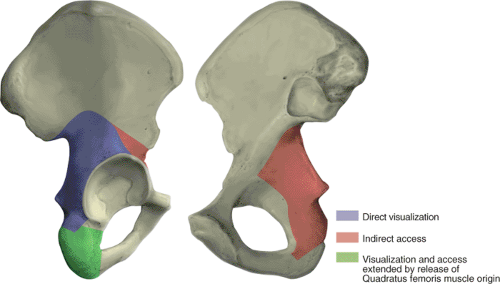
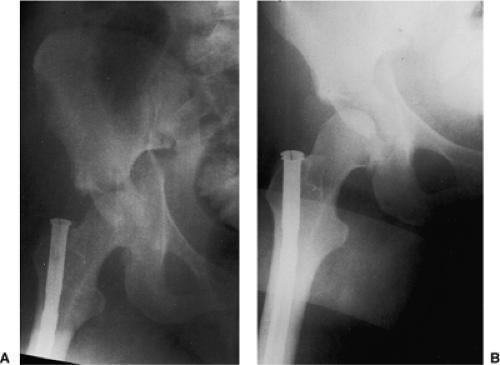
In choosing the appropriate surgical approach, the surgeon has an objective to select the least extensive exposure that allows sufficient bony access for anatomic joint reconstruction. The Kocher-Langenbeck approach provides direct visualization of the entire lateral aspect of the posterior column of the acetabulum (Fig. 41.1) (1). Indirect access to the true pelvis and to the anterior column can be attained by the palpating finger or through the use of special instruments (Figs. 41.1, 41.2 and 41.3) (1). Therefore, the Kocher-Langenbeck approach is applied in the treatment of fractures with the main displacement involving the posterior column. In the classification of Letournel and Judet (Table 41.1), this group consists of six fracture types: posterior wall, posterior column, posterior column and wall, transverse, transverse and posterior wall, and T-shaped. The Kocher-Langenbeck approach is the surgical exposure of choice for the first three types, in which the
fracture extent is limited to the posterior wall or column or both. For the transverse, transverse and posterior wall, and T-shaped fractures, some decision making is required. All three of these fracture types have a transverse fracture line as a common component. As a general guideline, if the fracture is less than 15 days old and the transverse component is located at (juxta-) or below (infra-) the level of the roof (tectum) of the acetabulum (therefore not involving the weight-bearing area of the acetabulum), the Kocher-Langenbeck approach is indicated (1). Otherwise, an alternative exposure, such as the extended iliofemoral approach, should be used. For acute juxtatectal- and infratectal-level transverse and T-shaped fractures, in which the major displacement occurs anteriorly at the pelvic brim and only minor posterior displacement, the ilioinguinal approach is perhaps the best choice.
fracture extent is limited to the posterior wall or column or both. For the transverse, transverse and posterior wall, and T-shaped fractures, some decision making is required. All three of these fracture types have a transverse fracture line as a common component. As a general guideline, if the fracture is less than 15 days old and the transverse component is located at (juxta-) or below (infra-) the level of the roof (tectum) of the acetabulum (therefore not involving the weight-bearing area of the acetabulum), the Kocher-Langenbeck approach is indicated (1). Otherwise, an alternative exposure, such as the extended iliofemoral approach, should be used. For acute juxtatectal- and infratectal-level transverse and T-shaped fractures, in which the major displacement occurs anteriorly at the pelvic brim and only minor posterior displacement, the ilioinguinal approach is perhaps the best choice.
The status of the local soft tissues is an important additional consideration. Acetabular fracture surgery through a compromised soft-tissue envelope is ill advised because of the increased risk of infection. Closed, degloving, soft-tissue injuries over the trochanteric region associated with underlying hematoma formation and fat necrosis (the Morel-Lavalle lesion) or open wounds may require debridement followed by delayed wound closure (1). The fracture pattern should be reassessed to determine whether reduction and fixation can be accomplished by using an alternative surgical approach located outside of the zone of soft-tissue injury. Another treatment option is to delay surgery until wound healing. This delay, as noted previously, may preclude use of the Kocher-Langenbeck approach.
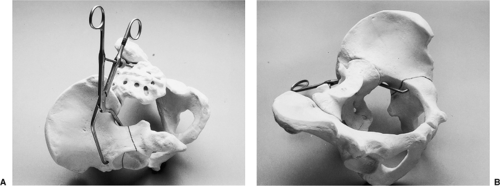
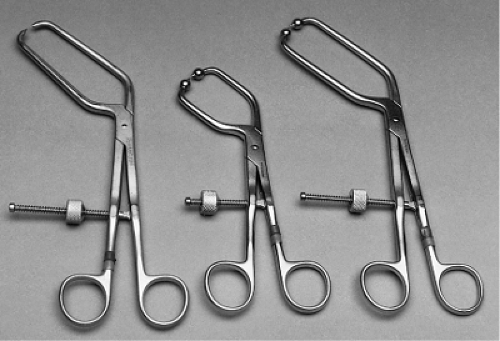 Figure 41.2. Examples of available special instruments that permit intrapelvic and anterior column access. |
Preoperative Planning
In most cases, patients with an acetabulum fracture have sustained high-energy trauma. Therefore, examination of the injured limb, even in those with an apparent isolated injury, should be just one part of a comprehensive and systematic approach. Associated injuries can be life or limb threatening. The Advanced Trauma Life Support evaluation sequence should be followed (Table 41.2). Detailed examination of the hip and lower extremity is performed during the secondary survey. As previously noted, soft-tissue injury has important implications regarding subsequent surgery; therefore, the soft tissues should be evaluated carefully. The incidence of preoperative, posttraumatic, sciatic-nerve injury was reported as being as high as 31% (2). Other peripheral nerves, such as the femoral and obturator nerves, also may be injured. A complete and clearly documented neurologic examination is extremely important both for patient prognosis and for medical-legal concerns. Preoperatively, this evaluation should be repeated periodically.
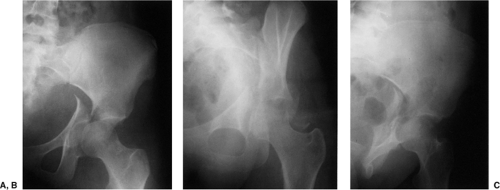
The initial anteroposterior (AP) x-ray of the pelvis is obtained during the secondary survey and can provide substantial diagnostic information regarding fracture type, as well as indicate a need for emergency treatment (Fig. 41.4). This x-ray must be supplemented by further studies to define completely the acetabular fracture pattern. The three necessary additional plain x-rays (Fig. 41.5) are centered on the affected hip and include an AP and
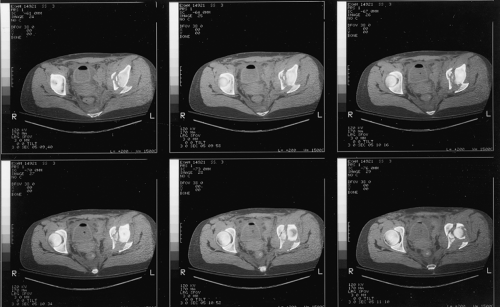
two 45-degree oblique views (the internal or obturator oblique view and the external or iliac oblique view) (1). Although these four plain x-rays usually provide all the information needed to define the acetabular fracture type, the standard two-dimensional computed tomography (CT) scan can supply important additional information and is indispensable for preoperative planning (Fig. 41.6). The eventual universal availability of high-quality three-dimensional CT reconstructions may eliminate much of the mystery associated with the radiographic interpretation of acetabulum fractures (Fig. 41.7). However, except for the AP
hip x-ray, which in most cases provides the same information as the AP pelvis examination, the plain and two-dimensional CT radiographic studies continue to be indispensable and should be viewed concurrently to make the definitive fracture diagnosis (1).
two 45-degree oblique views (the internal or obturator oblique view and the external or iliac oblique view) (1). Although these four plain x-rays usually provide all the information needed to define the acetabular fracture type, the standard two-dimensional computed tomography (CT) scan can supply important additional information and is indispensable for preoperative planning (Fig. 41.6). The eventual universal availability of high-quality three-dimensional CT reconstructions may eliminate much of the mystery associated with the radiographic interpretation of acetabulum fractures (Fig. 41.7). However, except for the AP
hip x-ray, which in most cases provides the same information as the AP pelvis examination, the plain and two-dimensional CT radiographic studies continue to be indispensable and should be viewed concurrently to make the definitive fracture diagnosis (1).
Table 41.1. Acetabular Fracture Classification | |||||
|---|---|---|---|---|---|
|
Table 41.2. Advanced-Trauma Life-Support Evaluation Sequence | ||||||
|---|---|---|---|---|---|---|
|
Table 41.3. Indications for Emergency Acetabular Fracture Fixation | |||||||
|---|---|---|---|---|---|---|---|
|
After careful physical examination and radiographic study, the appropriate surgical approach can be determined. The indications for emergency fracture fixation are uncommon (Table 41.3). Operative treatment is generally delayed 3 to 5 days to allow stabilization of the patient’s general status and for preoperative planning. My preference is to use preoperative, skeletal, femoral-pin traction both to maintain an unstable hip in a located position and to prevent further femoral head articular-surface damage from abrasion by the raw acetabular bony fracture surfaces (Fig. 41.8). Significant intraoperative blood loss can occur.
Two to four units of blood should be made available, depending on the extent of the fracture pattern. The use of an autologous blood-transfusion system, such as the cell saver, may decrease the need for intraoperative, homologous, banked-blood transfusion.
Two to four units of blood should be made available, depending on the extent of the fracture pattern. The use of an autologous blood-transfusion system, such as the cell saver, may decrease the need for intraoperative, homologous, banked-blood transfusion.
Surgery
Patient Positioning
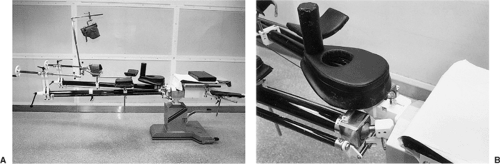
Acetabular fracture fixation using the Kocher-Langenbeck approach can be performed with the patient in either the lateral or the prone position. Orthopedic surgeons from North America are more familiar with and perhaps more comfortable using lateral positioning with the affected extremity draped free, as in hip arthroplasty surgery (Fig. 41.9). However, the Kocher-Langenbeck approach is most effective with the patient placed prone on a fracture table. The benefits of the prone position are realized by maintaining the femoral head in a reduced position. Gravity becomes a help rather than a hindrance in fracture exposure and reduction. The fracture table provides controlled traction and limb positioning, further assisting in fracture reduction. Traction is applied through use of a distal femoral pin with the knee flexed to approximately 90 degrees (Fig. 41.10). This angle of knee flexion places the sciatic nerve in a relaxed position, minimizing the risk of intraoperative sciatic-nerve injury. An unscrubbed assistant is required for intraoperative adjustment of the table.
With the patient placed prone, chest rolls should be used to elevate the head and to avoid excessive abdominal pressure. The fracture table generates the added risk of injury (i.e., pudendal nerve palsy) from pressure against the perineal post. The Judet fracture table, an updated version of which is now available from Orthopedic Systems, Inc. (Union City, CA), adequately addresses these concerns (Figs. 41.10 and 41.11).
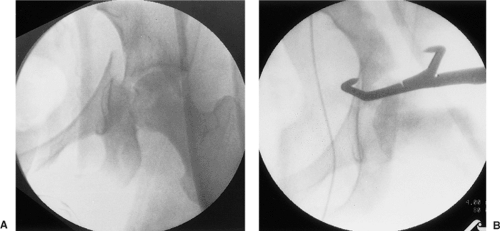
No matter what the patient position, use of a radiolucent operating table is advisable. Intraoperative c-arm fluoroscopy can then be used to assess fracture reduction and hardware location (Fig. 41.12). Before the sterile preparation and draping of the patient, the hip area should be quickly scanned with the c-arm to ensure adequate fluoroscopic visualization.
Surgical Procedure
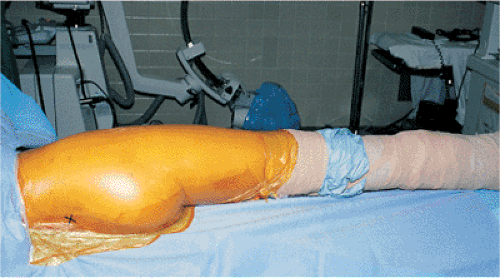
With the patient in the lateral position and the limb draped free, the sterile field is similar to that in hip arthroplasty surgery but extended posteriorly to include the region of the posterior–superior iliac spine (Fig. 41.13). With the patient prone on the fracture table, the sterile field consists of the buttock and the posterior and lateral aspects of the thigh (Fig. 41.14).
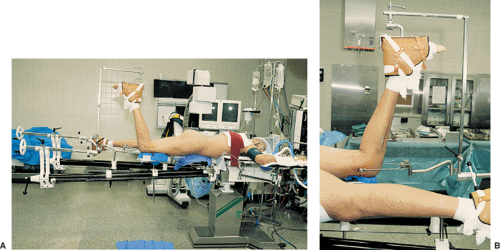 Figure 41.10. Patient in the prone position for surgery on the right hip (A) with a detailed view of the affected limb and femoral pin position (B). |
The skin incision (Fig. 41.15) is centered over the greater trochanter. The proximal branch of the incision is directed toward the posterior–superior iliac spine, ending approximately 6 cm short of this bony landmark. Distally, the incision extends approximately 15 cm along the midlateral aspect of the thigh. This skin incision is carried through the subcutaneous tissue and superficial fascia onto the fascia lata of the lateral thigh (the iliotibial tract) and the thin, deep fascia overlying the gluteus maximus muscle (Fig. 41.16).
The fascia lata is then divided in line with the skin incision, beginning at the distal aspect of the wound, continuing proximally toward the greater tuberosity, and ending at the first sighting of the gluteus maximus muscle fibers as they insert into the iliotibial tract (Fig. 41.17). The trochanteric bursa of the gluteus maximus (a large bursa between the
tendon of this muscle and the posterolateral surface of the greater trochanter) is incised, allowing clear visualization of the insertion area of the gluteus maximus muscle and access to the undersurface of this muscle (Figs. 41.18 and 41.19). Beginning the deep dissection in this way, at the distal branch of the Kocher-Langenbeck incision, the surgeon facilitates the next step: splitting of the gluteus maximus muscle.
tendon of this muscle and the posterolateral surface of the greater trochanter) is incised, allowing clear visualization of the insertion area of the gluteus maximus muscle and access to the undersurface of this muscle (Figs. 41.18 and 41.19). Beginning the deep dissection in this way, at the distal branch of the Kocher-Langenbeck incision, the surgeon facilitates the next step: splitting of the gluteus maximus muscle.
 Get Clinical Tree app for offline access 
|