Gastrocnemius and Soleus Rotational Muscle Flaps: Soft-Tissue Coverage
Randy Sherman
Sharad Rhaban
Indications/Contraindications
A muscle flap is indicated when vital structures such as bones, joints, tendons, or hardware are exposed and require coverage. In the lower leg and particularly the tibia, a muscle flap must be well vascularized and durable. Of all the local rotational flaps, the gastrocnemius is one of the most reliable. The gastrocnemius is a broad muscle with a single proximal vascular pedicle, which is well protected in the popliteal fossa. The gastrocnemius muscle or myocutaneous rotational flap is used for the procedure of choice for soft-tissue coverage of complex open wounds about the knee and proximal third of the tibia and fibula. The use of this flap is indicated in the following circumstances: (a) coverage of acute, grade IIIB, open, tibial fractures with or without hardware involving exposure of the knee joint, capsule, fracture site, or exposed cortex (Fig. 46.1); (b) obliteration of dead space and wound closure after radical debridement of osteomyelitic wounds in this region as well as infected nonunions (Fig. 46.2); (c) coverage of exposed total-knee arthroplasties or pre-arthroplasty tissue augmentation in densely scarred wound beds (Fig. 46.3); and (d) limb salvage and coverage of endoprostheses or allograft material after resection of musculoskeletal neoplasms (Fig. 46.4).
The soleus muscle, without a myocutaneous correlate, has a much more limited area of rotation and is used primarily for small, medially based, open wounds in the middle third of the leg. Indications include coverage of acute open fractures and chronic osteomyelitic wounds (Fig. 46.5).
Contraindications to the use of a gastrocnemius flap include vascular compromise of the muscle itself by disruption of the sural artery pedicle, compromise of the popliteal artery from which it emanates, or occlusion of the proximal arterial tree. Significant local trauma to the muscle itself, although rare, prevents its successful rotation.
 Figure 46.1. Grade IIIB open tibial-plateau fracture with exposed knee joint after internal fixation and unsuccessful attempt at primary wound closure. |
 Figure 46.2. Dead space involving skin, subcutaneous tissue, muscle, and bone in a proximal-third infected nonunion. |
 Figure 46.3. Scarred, atrophic, prepatella skin in an elderly patient after removal of an infected total-knee arthroplasty. |
 Figure 46.4. A 10-year-old girl immediately after tumor extirpation of a proximal tibial osteosarcoma and placement of endoprosthesis after loss of anterior skin. |
 Figure 46.5. Middle-third grade IIIB open-tibial fracture with a bony sequestrum and loss of overlying soft tissue. |
Recipient-site contraindications include a wound in the proximal third region in which its size and dimension are too large for coverage by the gastrocnemius muscle. Similarly, injury to the substance of the soleus muscle will hinder its ability to be transposed. Vascular compromise to the soleus muscle is extremely rare because of its segmental inflow. Because of minor perforators that exit from the posterior tibial artery distally, the surgeon must take great care to assure adequate vascularity to the most distal aspect of the soleus muscle when a large transposition is undertaken. As with the gastrocnemius, a large anterior or laterally located wound in the middle third of the leg may not be completely covered by the soleus muscle (Fig. 46.6), and free tissue transfer may be a better option.
 Figure 46.6. Large, grade IIIB, open, middle-third tibial fracture cannot be closed by a local soleus flap and requires free tissue transfer. |
As with any muscle-coverage procedure, infection or tumor recurrence is best avoided by thorough debridement or excision before wound closure. No muscle flap will successfully combat retained sequestrum or loose infected hardware, which act as nidi for continued infection.
Preoperative Planning
A thorough examination of the patient is crucial when planning either a gastrocnemius or soleus muscle flap for coverage of a complex open wound. Radiographs should be viewed with particular attention paid to fracture location and the presence or absence of internal fixation devices. For acute fractures, if an external fixator is indicated, the surgeon should anticipate the need for subsequent soft-tissue closure and construct the frame to allow unrestricted transposition of the muscles from the posterior to a medial or anterior plane. The zone of injury around the fracture site should be recognized because aggressive or radical debridement may significantly alter the dimensions of the wound (Fig. 46.7). Clinical examination of the leg should be made, with particular attention paid to would length, width, and depth. Other factors such as induration, discoloration, ecchymosis, and cellulitis must be considered.
A detailed vascular examination with palpation of the dorsalis pedis and posterior tibial pulses for arterial inflow, as well as Doppler examination for venous outflow, should be documented. Arteriography may be indicated if pulses are absent or diminished (Fig. 46.8). The function of the posterior compartment muscles should be assessed whenever possible. Sensory examination of the foot must be documented, with particular attention given to the posterior tibial, sural, and saphenous nerves. The surgical incisions can be planned in conjunction with the need for additional debridement and internal or external fixation of the fracture.
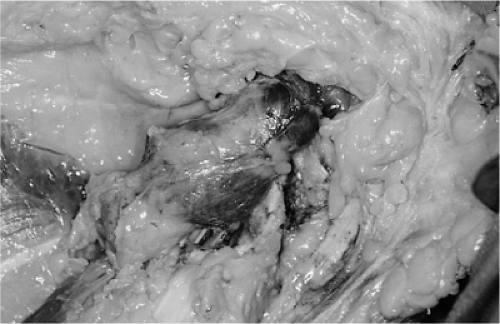 Figure 46.7. Large amount of retained titanium from a previously removed, infected, total-knee arthroplasty. |
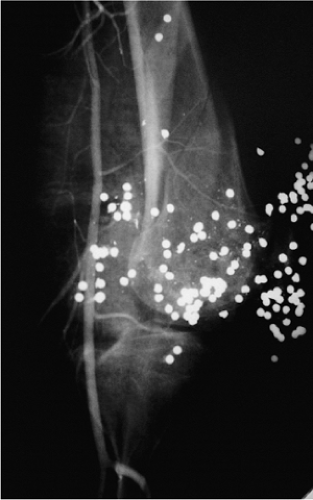 Figure 46.8. Angiogram demonstrating patency of the popliteal artery and continuity of the sural arteries despite the fracture comminution and retained gunshot pellets. |
 Figure 46.9. Completed debridement of infected fracture of the knee with removal of all nonviable soft tissue and bony sequestrum. |
Surgery
Gastrocnemius
A muscle flap procedure is undertaken only after complete and definitive debridement of a traumatic or infected wound has been completed or a tumor has been extirpated (Fig. 46.9). A tourniquet is placed on the thigh, and the entire leg is prepped and draped. The approach to the gastrocnemius muscle can be made through perpendicular, oblique, or parallel incisions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









