Fractures
Zachary V. Roberts
Milton L. Chip Routt
Sterile Instruments/Equipment
- Large and small pointed bone reduction clamps (Weber clamps)
- Assorted pelvic reduction clamps
- Femoral distractor
- Plate bender
- Implants
- Long 3.5-mm screws
- Long 4.5-mm screws
- Long 7.0-mm cannulated screws
- Mini-fragment screws for free osteochondral fragments
- 3.5-mm reconstruction plates
- Long 3.5-mm screws
- K-wires and wire driver/drill
Patient Positioning
(For additional details, see the chapter (1))
Prone
- Radiolucent table.
- Chest rolls are made from two blankets folded into thirds without wrinkles.
- Gel rolls are not radiolucent.
- Prep the leg free, clean and scrub the perineum with alcohol, and drape out with plastic adhesive drapes prior to the betadine prep.
- After prepping, towel out the surgical field and drape.
Supine
- Radiolucent table.
- Two blanket bump under the sacrum to allow access for iliosacral screw placement if needed.
- Prep down to the table, from the genitalia to the xiphoid process. Include the lower rib cage in surgical field.
Surgical Approaches
Kocher-Langenbeck
- The Kocher-Langenbeck approach is the most common approach used for treating acetabular fractures involving the posterior wall and column.
- Incision comprises an oblique limb from the posterior superior iliac spine (PSIS) to the greater trochanter and a vertical limb that continues distally over the lateral aspect of the femur.
- The vertical limb is made first by incising the skin and subcutaneous fat to identify the fascia of the iliotibial (IT) band.
- The IT band is then incised longitudinally from distal to proximal until fibers of the gluteus maximus are encountered at the level of the greater trochanter.
- The oblique limb of the incision is then begun at the cranial portion of the vertical limb and continued in a direction toward the PSIS.
- The fascia overlying the gluteus maximus is identified and incised, and the muscle fibers are split bluntly.
- The orientation of the oblique limb should parallel the gluteus maximus muscle fibers, allowing this muscle to be split more easily.
- The fascia overlying the gluteus maximus is identified and incised, and the muscle fibers are split bluntly.
- The superior gluteal neurovascular bundle and its major branches can be identified by palpation in the interval between the gluteus medius and the gluteus maximus and should be preserved if possible.
- Identify the sciatic nerve dorsal to the quadratus femoris.
- Displaced fracture fragments will often distort or disrupt the anatomy of the piriformis, gemelli, and obturator internus tendon, making identification of the sciatic nerve difficult in this traumatized zone.
- With the sciatic nerve identified, debride the trochanteric bursa.
- Identify and tenotomize the piriformis and obturator internus.
- Place a retention suture in these tendons for later repair.
- Follow the obturator internus tendon to the lesser sciatic notch.
- With the knee flexed, retract the obturator internus tendon and sciatic nerve.
- Debride the injured superior and inferior gemelli muscles from the lateral ischium.
- The caudal portion of the gluteus minimus is often significantly damaged and should be debrided back to the level of the caudal branch of the superior gluteal neurovascular bundle.
- This debridement will improve exposure to the supra-acetabular region of the ilium.
- This can also minimize the risk of postoperative heterotopic ossification development.1
- This debridement will improve exposure to the supra-acetabular region of the ilium.
Ilioinguinal approach
- The surface landmarks for the incision are the pubic symphysis, anterior superior iliac spine (ASIS), and the iliac crest.
- The incision begins 1 to 2 cm cranial to the pubic symphysis, extends toward the ASIS, and follows the iliac crest to the level of the gluteus medius pillar, where it continues cranially for several centimeters.
- Identify the fascia along the length of the incision; also identify and preserve the spermatic cord/round ligament and external inguinal ring.
- Which window is opened first is a matter of preference.
- Important considerations include the location of major fracture components; whether certain windows are needed to visualize, clean, clamp, or apply fixation to fracture components; and, finally, anticipated bleeding issues.
- The iliac window is frequently associated with significant fracture bleeding upon exposure (particularly when there is iliac wing comminution), and often this bleeding is controlled only by fracture reduction.
- Thus, if the middle or Stoppa windows are needed for the reduction or fixation, it is reasonable to expose them first.
- The fracture often must be cleaned to obtain anatomic reduction; however, this should be the last step of the exposure.
- Debridement of clot from fracture planes tends to produce bleeding from the cancellous surfaces, which often can only be controlled by fracture reduction.
- Thus, be ready to implement the reduction and fixation plan immediately after cleaning the fracture to avoid excessive bleeding.
- Debridement of clot from fracture planes tends to produce bleeding from the cancellous surfaces, which often can only be controlled by fracture reduction.
Iliac window
- The common insertion of the abdominal obliques joins the origins of the tensor fascia lata and gluteus medius at the lateral edge of the iliac crest.
- This tendinous structure should be divided from ASIS to the gluteus medius pillar, leaving the abductor origin intact on the ilium.
- The gluteus medius pillar roughly marks the equator of the pelvic ring (in the supine position).
- Roughly at this landmark, the exposure may either be continued posteriorly along the iliac crest or extended cranially, splitting the fibers of the external oblique muscle.
- If the latter is performed, the transversus abdominis and internal obliques are released from their insertion using electrocautery, working from the inner table of the iliac crest outward.
- Roughly at this landmark, the exposure may either be continued posteriorly along the iliac crest or extended cranially, splitting the fibers of the external oblique muscle.
- Elevate the iliacus from the iliac fossa subperiosteally.
- Bleeding is often encountered from the nutrient vessel that enters the ilium just lateral to the pelvic brim and anterior to the sacroiliac joint.
- Bone wax may help provide hemostasis for bleeding associated with this nutrient foramen.
- Fractures in this region can also bleed vigorously.
- Bone wax may help provide hemostasis for bleeding associated with this nutrient foramen.
Middle window
- The external oblique fascia is incised from the ASIS to a point 1 cm cranial to the external inguinal ring and reflected inferiorly to identify the inguinal ligament.
- The internal oblique and transversus abdominis insertions on the inguinal ligament are incised along the length of the ligament with a 1-mm cuff to facilitate repair.
- This will expose the iliopectineal fascia, which needs to be carefully dissected and incised to open the middle window and allow mobilization of the iliac vessels and iliacus muscle.
- The iliopectineal fascia is an oblique fascial structure that spans the superior ramus and the inguinal ligament anteriorly.
- It becomes confluent with the periosteum of the ilium as it courses dorsally along the pelvic brim to the sacroiliac joint.
- It separates the lacuna vasorum containing the iliac vessels, lymphatics, and pectineus origin from the lacuna musculorum containing the iliopsoas and femoral nerve.
- It becomes confluent with the periosteum of the ilium as it courses dorsally along the pelvic brim to the sacroiliac joint.
- Adequate release of the iliopectineal fascia increases the utility of the iliac and Stoppa windows.
- The intact iliopectineal fascia will limit medial retraction of the iliacus while working in the iliac window and anterolateral retraction of the iliac vessels while working in the Stoppa window.
Stoppa window
- Use of this window requires the surgeon to stand on the opposite side of the patient than the side of injury and provides access to the quadrilateral surface, the upper surface of the superior ramus, and the pubic symphysis.
- The fascia between the rectus abdominis muscles is divided longitudinally in the midline.
- Frequently, one or both rectus abdominis muscles may be avulsed from their insertion on the pubis.
- If not, 2 to 3 cm of the insertion can be elevated from the anterior surface of the pubis to increase exposure.
- As long as the distal insertion is left intact, it can be repaired easily to the contralateral side without tension.
- If not, 2 to 3 cm of the insertion can be elevated from the anterior surface of the pubis to increase exposure.
- Malleable retractors are used to retract the bladder.
- The periosteum overlying the superior ramus is incised and dissection proceeds medial to lateral in a subperiosteal fashion.
- Retropubic vascular anastomoses between the superficial and deep iliac vascular systems are common and should be identified, ligated, and divided in a controlled manner, if present.
- The obturator neurovascular bundle is tethered distally by the obturator membrane and thus limits the caudal extent of the Stoppa window’s exposure.
- The upper extend of the Stoppa window merges with the medial extent of the middle window after the iliopectineal fascia insertion is released from the pelvic brim.
Fracture Assessment Tips
- According to the system developed by Emile Letournel, acetabular fractures are classified by fracture morphology and location into elementary or associated fracture patterns.
- Collectively understanding the fracture morphology and the behavior of its component fragments is vital to developing and executing a successful operative plan.
- The pelvis fractures along predictable fault planes, producing several commonly recurring fracture fragments.
- Fragment displacement is often asymmetric along the fracture plane, being tethered at one edge by intact soft tissues that act as a point of rotation or hinge between the two fragments.
- These soft tissue hinges are helpful in that they can allow a strategically placed clamp to compress the entire fracture surface, despite its relatively large area.
- Likewise, indirect reduction of a secondary fragment may be accomplished upon reduction of the primary fragment, if intact soft tissues span the two.
- Fragment displacement is often asymmetric along the fracture plane, being tethered at one edge by intact soft tissues that act as a point of rotation or hinge between the two fragments.
Reduction and Fixation Techniques
The Posterior Wall Fragment
- It is the most common elementary acetabular fracture pattern but has extremely variable morphology.
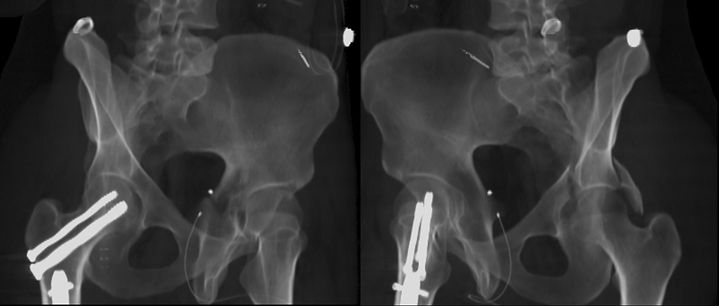
- It may be caused by axial load applied through an intact femur (Fig. 11-1), as in a posterior hip fracture dislocation, or it may be caused by avulsion mechanism in associated patterns (Fig. 11-2) where there is significant medial displacement of the femoral head relative to the posterior wall of the acetabulum.
Figure 11-1. The posterior wall component of this associated transverse and posterior wall acetabular fracture demonstrates the type of fracture that is “pushed off” by the femoral head during axial load, with tension failure of the caudal labrum and an intact cranial labrum.
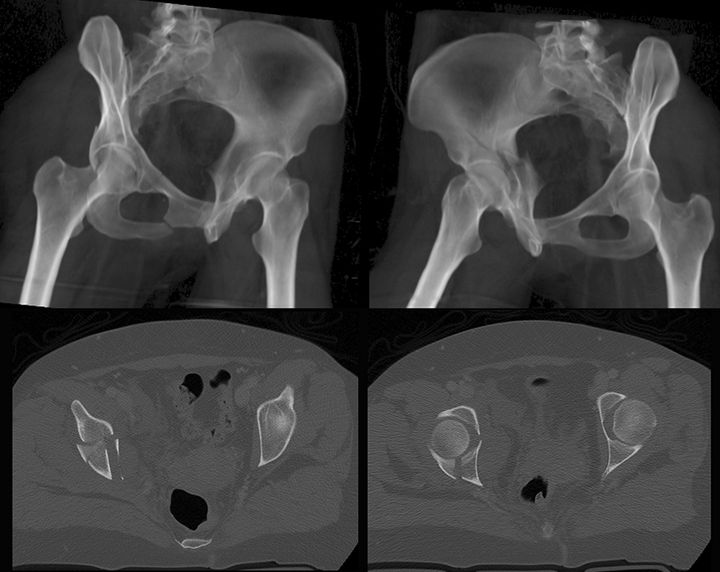
Figure 11-2. “Avulsion” posterior wall. In addition to having an incomplete anterior column component, this associated both-column acetabular fracture has a large posterior wall fracture component. In this type of posterior wall fracture, the fragment is avulsed from the intact ilium as the femoral head dislocates medially. The labrum and capsule are typically intact; however, the stability of the hip joint should be assessed after repair of the column components to determine the need for reduction and fixation of this posterior wall fragment.
![]()
- Posterior wall fracture fragments typically have an intact labral attachment.
- In fractures with a single dominant wall fragment produced by an axial force, this attachment is typically cranial, allowing the fragment to displace primarily by rotation around this tethered point (Fig. 11-3).

Figure 11-3. The CT scan demonstrates rotatory displacement of a “pushed-off” posterior wall fragment around an intact cranial labrum.
![]()
- Comminuted posterior wall fractures produced by axial force may have both cranial and caudal labral attachments, allowing the fragments to rotate open similar to a saloon door.
- Avulsion posterior wall fractures are usually found to have an intact labrum and a capsule.
- Marginal impaction is frequently present and can occur on the intact portion of the acetabulum or on the fractured wall (Fig. 11-4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree