Abnormalities of Rate and Rhythm
Bryan Cannon
NORMAL SINUS RHYTHM
The sinus node is located in the upper portion of the heart at the junction of the superior vena cava and the right atrium. Impulses that begin atrial contraction typically come from this position. For this reason, the normal P-wave axis is between 0 and 90 degrees (i.e., positive P waves in leads I and aVF). The sinus node is not a discrete structure but rather is an oblong structure along the lateral wall of the right atrium. Therefore, for normal subjects to have P waves with two different origins is not unusual. The P-wave axis and morphology may change such that the P wave varies from positive to negative in lead aVF. For the pacemaker to originate in the left atrium, rendering the P wave negative in lead I, is extremely rare, and an abnormal tachycardia focus must be excluded in this situation.
In sinus arrhythmia (also known as respiratory sinus arrhythmia), the P-wave axis remains normal, but the interval between P waves increases with inspiration and decreases with expiration. This phenomenon is related to changes in vagal tone and is entirely normal. This variation in rate rarely exceeds 100% (e.g., from a rate of 60 to 120 beats per minute); if it does, it may signify a pathologic process.
Sinus bradycardia is defined as a heart rate below the normal limits for age. The normal values for heart rate are listed in Table 287.1. Sinus bradycardia typically is associated with increased vagal tone and only rarely is related to a primary cardiac cause. The most common reason for sinus bradycardia is the athletic heart, a condition that may cause bradycardia in adolescents and requires no further workup if the patient is asymptomatic. Other reasons for sinus bradycardia include the presence of increased intracranial pressure, anorexia nervosa, gastric distention, pharyngeal stimulation, and drugs that potentiate bradycardia (e.g., digoxin, beta blockers, sedatives).
In an otherwise asymptomatic patient, sinus arrhythmia and sinus bradycardia require no further evaluation. However, excessive variation in the rate or constant sinus bradycardia even with activity may indicate an underlying abnormality.
TABLE 287.1. HEART RATES IN NORMAL INFANTS AND CHILDREN | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||
ABNORMALITIES IN SINUS RHYTHM: WOLFF-PARKINSON-WHITE SYNDROME AND LONG QT INTERVAL
On any routine electrocardiogram (ECG), the tracing should be examined for the possible presence of two disorders: Wolff-Parkinson-White syndrome and long QT interval. Automated pediatric ECG analysis programs often can miss these abnormalities. Both disorders may cause syncope or seizure-like activity in a previously well child. An ECG to evaluate for these disorders should be a part of the workup of a patient who presents with syncope or a nonfebrile seizure.
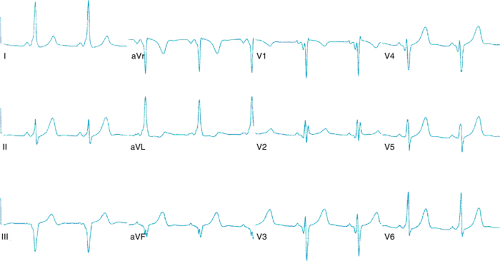
Wolff-Parkinson-White syndrome involves the constellation of three findings: a PR interval shorter than normal for age, a slurred upstroke of the QRS complex (i.e., a delta wave), and a QRS complex longer than normal for age (Fig. 287.1). There are frequently changes in the ST or T waves. These findings may not be present in all leads, and the midprecordial leads (V2 to V4) may be the most sensitive. Other clues to the presence of Wolff-Parkinson-White syndrome are left axis deviation, the absence of Q waves in lead V6, and abnormally wide Q waves in the limb leads. Patients with Wolff-Parkinson-White syndrome usually have structurally normal hearts, but the syndrome can be associated with congenital heart disease such as Ebstein anomaly of the tricuspid valve, corrected transposition of the great arteries, and hypertrophic cardiomyopathy. For this reason, an echocardiogram is indicated in patients with this disorder.
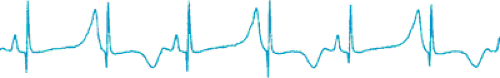
A prolonged QT interval is diagnosed when the corrected QT interval, or QTc, (i.e., QT interval in seconds divided by the square root of the previous RR interval in seconds) is longer than 0.44 in a child and 0.45 in an adolescent female patient. Patients with a prolonged QT interval may have prolonged QT syndrome. The T waves in these patients frequently appear flattened or abnormal. Patients with prolonged QT syndrome are at risk for having ventricular arrhythmias (particularly a form of polymorphic ventricular tachycardia called torsade de pointes) and sudden death. Patients with prolonged QT syndrome may have sinus bradycardia and occasionally have T-wave alternans (upright T wave alternating with a negative T wave in the same lead of an ECG tracing; Fig. 287.2). Treatment with beta blockers has been shown to decrease the risk of sudden death occurring in patients with prolonged QT syndrome. A number of medications (including erythromycin) can prolong the QT interval and should be avoided by these patients. Implantable cardioverter-defibrillator placement is indicated in those patients with ventricular tachycardia, recurrent syncope, or resuscitated sudden death. Prolonged QT syndrome frequently is familial, and several different ion channel defects have been identified. A prolonged QT interval also can result from medications or electrolyte imbalances, and these patients also may be predisposed to having ventricular arrhythmias.
ATRIOVENTRICULAR BLOCK
First-degree atrioventricular (AV) block is diagnosed when the PR interval is above normal limits for age. Normal PR intervals are less than 0.14 for children younger than 2 months of age, less than 0.16 for children between 2 months and 8 years, less than 0.18 in children older than 8 years of age, and less than 0.2 in older adolescents and adults. First-degree AV block typically is a benign condition resulting from increased vagal tone. It rarely progresses to a higher degree of block. No further evaluation is necessary in the asymptomatic patient.
Four types of second-degree AV block exist. The first type is Mobitz type I, also known as Wenckebach, which results in a progressive lengthening of the PR interval until a P wave is not conducted to the ventricle. It also may result from increased vagal tone. During sleep, this block can be a normal phenomenon. It does not require further evaluation unless it occurs while the patient is awake or it is associated with symptoms. Mobitz type II is failure to conduct to the ventricle with no associated progressive lengthening of the PR interval. This type of block always is abnormal and requires additional testing. Another form of second-degree AV block is 2:1 AV block, which occurs when every other P wave is not conducted. The final type is high-grade second-degree AV block, in which two or more consecutive P waves do not conduct to the ventricle but still some evidence of AV conduction exists.
In complete AV block, the P waves are entirely dissociated from the QRS complexes (Fig. 287.3). The P and QRS complexes typically are regular, but small variations in both can occur. Complete AV block can be congenital or acquired. Congenital complete AV block typically is associated with maternal collagen-vascular disease, but it also can be associated with congenital heart disease. Mothers with collagen-vascular disease frequently are asymptomatic, although some may have systemic lupus erythematosus or a similar disease. Women with clinical or subclinical disease have a high titer of anti-Ro (ss-A) or anti-La (ss-B) antibodies that cross the placenta and preferentially attack the AV node. Affected infants usually do not have other signs of collagen-vascular disease. Despite a low antibody titer, the complete AV block does not reverse in these infants. Some infants born with second-degree AV block may develop complete AV block within the first year of life, a finding implying that congenital AV block may be an evolving process.
Children with congenital complete AV block may not require immediate pacemaker therapy. As long as the ventricular rate consistently is greater than 55 beats per minute and no symptoms of congestive heart failure exist, these infants and children fare quite well. If congenital heart disease coexists in these patients, pacing often is instituted earlier. Patients with complex ventricular ectopy or a ventricular escape rhythm also may require consideration for early pacing. As children with congenital complete AV block grow, they may exhibit subtle symptoms such as frequent napping, mild growth failure, night terrors, or intolerance for exercise. They also may develop dilation of their left ventricle. If these findings occur, pacemakers typically are implanted. Because of a risk for late development of complications, these children all will require pacemakers sometime before they reach adulthood.
Complete AV block outside the newborn period often is associated with congenital heart disease, most commonly corrected transposition of the great arteries. It also may occur secondary to infectious causes such as Chagas or Lyme disease, with rheumatic diseases, or acutely in the setting of electrolyte disturbances.
Patients with prolonged QT syndrome can have congenital high-grade or complete AV block. Patients with the combination of long QT syndrome with second- or third-degree AV block are at high risk for sudden death. Implantation of a pacemaker or implantable cardioverter-defibrillator is indicated in these patients.
Complete AV block also can occur after cardiac surgery. These patients are at higher risk for sudden death and frequently have a very slow underlying escape rhythm. For this reason, implantation of pacemakers is indicated in these patients.
SUPRAVENTRICULAR ARRHYTHMIAS
Premature Atrial Contractions
A premature atrial contraction (PAC) is defined on an ECG as a premature P wave. In most instances, it has a different morphology and axis from those of the sinus P waves. Most PACs are conducted to the ventricles with a normal QRS. When the premature P wave occurs early, conduction to the ventricles may occur with a different QRS morphology than that of sinus rhythm (i.e., aberrantly conducted PAC). This occurrence may simulate a premature ventricular contraction (PVC). For any early QRS complex that has a morphology different from that of the sinus beats, the preceding T wave should be examined carefully for a hidden P wave. Occasionally, a premature P wave may occur so early that it does not conduct to the ventricles at all (i.e., block). This situation may simulate sinus bradycardia because the premature P wave may reset the sinus node, delaying the next expected sinus impulse. In situations of paroxysmal bradycardia, especially those in which conducted PACs are on the same tracing, the T wave should be searched carefully for the presence of hidden P waves. This phenomenon is an especially common finding in newborn infants. Many tracings similar to the one in Fig. 287.4 are interpreted as multiform PVCs with PACs and sinus bradycardia, when in fact most of these patients have only PACs, some of which conduct aberrantly and some of which block. Isolated PACs are benign and do not require further evaluation. If frequent PACs are noted on an ECG or on monitoring strips, a 24-hour Cardio Scan monitor should be considered to exclude episodes of atrial tachycardia.
Atrial Flutter
Atrial flutter is an uncommon arrhythmia in the pediatric population. It typically occurs in newborn infants and postoperatively in patients with congenital heart disease. Newborn infants present with tachycardia and typical “saw-toothed” flutter waves on ECG. The atrial rate can be between 300 and 600 beats per minute with variable conduction to the ventricles. If the ECG is difficult to interpret, adenosine can be given intravenously to block the AV node and reveal the flutter waves. Treatment is direct-current synchronized cardioversion with 0.5 to 1 watt-second/kg. Atrial overdrive pacing also can be used to terminate atrial flutter. Newborns who have atrial flutter typically have no structural heart disease and have no further problems after returning to normal sinus rhythm. A 24-hour Cardio Scan should be placed after cardioversion because rarely reentrant tachycardias or atrial tachycardias will initiate atrial flutter. If the patient has no recurrence of the atrial flutter or evidence of other arrhythmias, no further evaluation is necessary. Patients with atrial flutter after surgery for congenital heart disease (also know as intraatrial reentrant tachycardia) typically require long-term treatment to control their arrhythmias. The atrial rate typically is slower (100 to 250 beats per minute), and the ECG baseline may return to normal between successive P waves. Therefore, to examine the T wave and QRS complex for evidence of a hidden P wave in patients with congenital heart disease and tachycardia is important.
Supraventricular Tachycardia
Supraventricular tachycardia (SVT) is defined as an abnormally rapid rhythm that originates proximal to the bifurcation of the bundle of His, that is caused by an abnormal mechanism
(specifically excluding sinus tachycardia), and that does not have flutter waves on the surface ECG (Fig. 287.5). The two basic mechanisms for SVT are automatic focus and reentry. Automatic tachycardias such as atrial ectopic tachycardia result from abnormal impulse generation in the atria and are a rare cause of SVT. This arrhythmia often is incessant and may present with an abnormal P-wave axis and prolonged PR interval on ECG. The atrial rate in atrial ectopic tachycardia may vary with catecholamine state and frequently displays periods or “warming up” and “cooling down” rather than a paroxysmal onset and termination. Adenosine typically blocks the AV node with no effect on the atrial rate and does not terminate the tachycardia. Cardioversion and overdrive pacing may suppress the atrial ectopic tachycardia temporarily, only to have it quickly resume its initial rate. Atrial ectopic tachycardia may be controlled with antiarrhythmic medication or may be eliminated using cardiac catheterization with ablation techniques. The remainder of the discussion focuses on reentrant tachycardias.
(specifically excluding sinus tachycardia), and that does not have flutter waves on the surface ECG (Fig. 287.5). The two basic mechanisms for SVT are automatic focus and reentry. Automatic tachycardias such as atrial ectopic tachycardia result from abnormal impulse generation in the atria and are a rare cause of SVT. This arrhythmia often is incessant and may present with an abnormal P-wave axis and prolonged PR interval on ECG. The atrial rate in atrial ectopic tachycardia may vary with catecholamine state and frequently displays periods or “warming up” and “cooling down” rather than a paroxysmal onset and termination. Adenosine typically blocks the AV node with no effect on the atrial rate and does not terminate the tachycardia. Cardioversion and overdrive pacing may suppress the atrial ectopic tachycardia temporarily, only to have it quickly resume its initial rate. Atrial ectopic tachycardia may be controlled with antiarrhythmic medication or may be eliminated using cardiac catheterization with ablation techniques. The remainder of the discussion focuses on reentrant tachycardias.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree