1
English version
This text is divided into three sections. The first section is devoted to the diagnosis of shaken baby syndrome (revealing signs, risk factors, investigations to be performed, possible lesions, etc.) and ends with suggested diagnostic criteria based on the infant’s clinical history and lesions.
The second section looks at whether certain mechanisms, The second section looks at whether other mechanisms (some of which are often cited, such as being dropped often-cited(such as being dropped or the performance of resuscitation manoeuvres) can induce injuries similar to those seen in shaken baby syndrome. It also looks at whether certain factors can favour the occurrence of injuries.
The third and last section focuses on the consequences (according to French regulations and legislation) of a diagnosis of shaken baby syndrome.
1.1
Abbreviations
AHI
abusive head injury
CIVI
Commission d’indemnisation des victimes infraction pénale (offense Victim Compensation Commission)
CRIP
Cellule de recueil, de traitement et d’évaluation des informations préoccupantes (County Child Abuse Prevention Office)
EDH
extradural haematoma
ESAS
enlargement of the subarachnoid space
HI
head injury
ITT
temporary total incapacity
MRI
magnetic resonance imaging
OPP
ordonnance de placement provisoire (temporary care order)
RH
retinal haemorrhage
SBS
shaken baby syndrome
SDH
subdural haematoma
1.2
Participants
This public audition was organized by the SOFMER (the French Society for Physical and Rehabilitation Medicine), with the participation of the following bodies:
- •
National College of Lecturers in General Practice
- •
Inserm – The French National Institute of Health and Medical Research
- •
InVS – The Health Surveillance Institute
- •
The French Society for Anaesthesia and Resuscitation
- •
The French Society for Emergency Medicine
- •
The French Society for Forensic Medicine
- •
The French Society for Paediatric Neurosurgery
- •
The French Academy of Neuropediatrics
- •
The French Academy of Pediatrics
- •
The National Union of Associations of Families of Victims of Brain Injury (UNAFTC)
1.2.1
Funding
- •
The Provincial Liberal Professions Health Insurance Fund
- •
The General Directorate for Health
- •
France Traumatisme Crânien
- •
The French Society for Physical and Rehabilitation Medicine (SOFMER)
- •
The French-Language Society for Paediatric Handicap Research (SFERHE)
- •
The Île-de-France Liberal Professions Health Insurance Fund
1.2.2
Organizing Committee
- •
Dr Anne Laurent-Vannier, physical and rehabilitation medicine specialist, Saint-Maurice – Chairperson of the Organizing Committee
- •
Dr Juliette Bloch, epidemiologist, InVS, Saint-Maurice
- •
Thierry Boulouque, Division Commissioner, Head of the Child Protection Unit, Paris
- •
Dr Jeanne Caudron-Lora, emergency physician, Créteil
- •
Professor Brigitte Chabrol, paediatrician, Marseille
- •
Frédéric De Bels, HAS, Saint-Denis La Plaine
- •
Dr Patrice Dosquet, HAS, Saint-Denis La Plaine
- •
Françoise Forêt, Honorary Professor, National Union of Associations of Families of Victims of Brain Injury (UNAFTC), Paris
- •
Dr Jose Guarnieri, neurosurgeon, Valenciennes
- •
Professor Vincent Gautheron, physical and rehabilitation medicine specialist, Saint-Étienne
- •
Dr Cyril Gitiaux, paediatrician, Paris
- •
Anne-Sophie Jarnevic, magistrate, Chartres
- •
Thérèse Michel, social worker, Tours
- •
Professor Gilles Orliaguet, specialist in anaesthesia and resuscitation, Paris
- •
Dr Claude Rougeron, general practitioner, Anet
- •
Professor Michel Roussey, paediatrician, Rennes
- •
Yvon Tallec, magistrate, Paris
- •
Professor Gilles Tournel, forensic physician, Lille
- •
Dr Anne Tursz, Research Director, Inserm, Villejuif
1.2.3
Hearing Commission
- •
Dr Mireille Nathanson, paediatrician, Bondy – Co-Chairperson of the Hearing Commission
- •
Fabienne Quiriau, Director of the National Convention of Child Protection Associations (CNAPE), Paris – Co-Chairperson of the Hearing Commission
- •
Aurélie Assie, social worker, Paris Child Assistance Unit, Family Reception Service, Ecommoy
- •
Dr Joseph Burstyn, ophthalmologist, Paris
- •
Dr Christine Cans, paediatrician, Grenoble
- •
Dr Catherine Arnaud, paediatrician, Toulouse
- •
Violaine Chabardes, gendarme (police officer), Lyon
- •
Hélène Collignon, journalist, Paris
- •
Dr Marie Desurmont, forensic physician, Lille
- •
Isabelle Gagnaire, childcare nurse, Saint-Étienne
- •
Professor Nadine Girard, radiologist, Marseille
- •
Professor Etienne Javouhey, resuscitation specialist, Lyon
- •
Dr Anne Laurent-Vannier, physical and rehabilitation medicine specialist, Saint-Maurice
- •
Dr Caroline Mignot, paediatrician, Paris
- •
Philippe Lemaire, magistrate, Riom
- •
Dr Sylviane Peudenier, neuropaediatrician, Brest
- •
Dr Bruno Racle, paediatrician, Versonnex
- •
Dr Pascale Rolland-Santana, general practitioner, Paris
- •
Dr Thomas Roujeau, neurosurgeon, Paris
- •
Dr Nathalie Vabres, paediatrician, Nantes
- •
Roselyne Venot, police officer, Versailles
1.2.4
Literature review coordinators
- •
Dr Elisabeth Briand-Huchet, paediatrician, Clamart
- •
Jon Cook, anthropologist, Villejuif
1.2.5
Experts
- •
Professor Thierry Billette de Villemeur, paediatrician, Paris
- •
Professor Jean Chazal, neurosurgeon, Clermont-Ferrand
- •
Professor Catherine Christophe, radiologist, Brussels
- •
Dr Sabine Defoort-Dhellemmes, ophthalmologist, Lille
- •
Dr Gilles Fortin, paediatrician, Montreal
- •
Dr Caroline Rambaud, forensic physician, Garches
- •
Professor Jean-Sébastien Raul, neurosurgeon, Strasbourg
- •
Dr Caroline Rey-Salmon, paediatrician, Paris
- •
François Sottet, magistrate, Paris
- •
Elisabeth Vieux, honorary magistrate, Paris
- •
Professor Mathieu Vinchon, neurosurgeon, Lille
- •
Professor Rémy Willinger, Professor of Biomechanics, Strasbourg
Illustrations supplied by the Société Francophone d’Imagerie Pédiatrique et Prénatale (SFIPP).
1.3
Guidance report. Shaken baby syndrome: the diagnostic work-up
1.3.1
The definition of shaken baby syndrome
SBS is a type of inflicted, non-accidental or AHI caused by shaking . The syndrome mainly occurs in infants under 1 year of age. The three studies with the largest number of cases are King et al. in Canada in 2003 , Mireau in France in 2005 and the Canadian Paediatric Surveillance Program (PCSP) in 2008 . The median age was 4.6 and 5 months in King et al. and the PCSP , respectively, whereas the mean age reported by Mireau was 5.4 months (the youngest infants in the latter study were 1 month old).
The literature data mainly concern AHI and not just SBS. Hence, some of the answers below are related to AHI in general.
The incidence of SBS varies between 15 and 30 per 100,000 infants under 1 year of age . When related to the number of the births in France, one can estimate that 120 to 240 infants a year may be concerned by this form of abuse. However, there are no epidemiological data for France; Mireau suggested a figure of 180 to 200 cases a year .
The published figures almost certainly underestimate the true incidence:
- •
the figures are mainly related to the most severe cases, which are probably also underreported;
- •
the lack of an autopsy in all suspicious infant deaths rules out certain diagnoses in some cases;
- •
it is often difficult to differentiate between abusive and accidental head injuries.
Missed diagnoses increase the risk of recurrence of abuse, as mentioned by a few publications ; a recent, retrospective study of 112 children identified the recurrence of SBS (from two to 30 times, with an average of 10 times) in 55% of cases.
1.3.2
Which elements (clinical signs, context, risk factors, etc.) are or may be suggestive of a diagnosis of shaken baby syndrome or may lead to misdiagnosis?
1.3.2.1
Initial signs and symptoms
There is major clinical heterogeneity:
- •
in the most serious cases, the child is found dead. The procedures to be followed in this event are specified below;
- •
the child presents signs that immediately suggest serious neurological damage, prompting immediate treatment:
- ∘
convulsions,
- ∘
severe malaise described by the parents (“I thought that my child was going to die”, “my child stopped breathing”) or observed by the physician (serious consciousness disorders, respiratory pauses, bradycardia),
- ∘
impaired vigilance (extending to coma),
- ∘
severe apnoea: very specific for AHI vs. accidental HI (in the study by Maguire et al. , the positive predictive value is 93%),
- ∘
fixed upward gaze,
- ∘
signs suggesting acute intracranial hypertension or even imminent herniation: postural disorders (decortication or decerebration, episodes of hypertonia), bradycardia, arterial hypertension, respiratory rhythm disorders;
- ∘
- •
the child presents signs that suggest neurological damage:
- ∘
changes in muscle tone (axial hypotonia),
- ∘
poor contact (the child does not respond well to stimuli and/or no longer smiles),
- ∘
a decrease in the child’s capabilities,
- ∘
increased head circumference, with a sudden change in the percentile class in the growth chart (which emphasizes the value of keeping a regularly updated family health notebook),
- ∘
a bulging fontanel;
- ∘
- •
the child presents non-specific signs that can lead to misdiagnosis:
- ∘
behavioural changes described by carers: crying, moaning, irritability, changes in sleep or feeding patterns, less smiling,
- ∘
vomiting,
- ∘
respiratory pauses,
- ∘
pallor,
- ∘
suspected pain.
- ∘
In all cases, the clinical examination must be thorough and performed after undressing the child; in particular it should include palpation of the fontanel, measurement of the head circumference (which should be checked against the growth chart) and examination of the whole body (including the scalp) for bruises.
Given the lack of specificity of several of these signs, a combination of signs may provide much more information ( Table 1 ). Thus, vomiting (which is a very frequent and banal symptom) is a warning sign if combined with a bulging fontanel, axial hypotonia, vigilance disorders and a shift towards the top of the head circumference curve.
| Signs observed | Frequency (%) |
|---|---|
| Axial hypotonia and an epilepsy attack | 53 |
| An epilepsy attack and bulging fontanel | 46 |
| Vomiting and bulging fontanel | 38 |
| Vomiting and axial hypotonia | 34 |
| A shift towards the top of the head circumference curve and bulging fontanel | 31 |
| Vomiting, an epilepsy attack and bulging fontanel | 25 |
| Vomiting and vigilance disorders | 24 |
| Vomiting, axial hypotonia and bulging fontanel | 23 |
| Vomiting, vigilance disorders and bulging fontanel | 19 |
The child’s medical history (family health notebook) should also be screened for the above-mentioned signs, since they may testify to previous HI.
Certain items of information in the infant’s medical history can suggest the occurrence of an AHI:
- •
a delay in seeking medical assistance and/or a lack of responsiveness by the family/carers;
- •
an absence of explanations for the observed clinical signs:
- ∘
in the series reported by Mireau , the family/carers did not report any trauma at all in 71.6% of the cases, despite repeated questioning,
- ∘
according to Hettler and Greenes , the fact that a history of trauma is not immediately reported is very discriminant for AHI, compared with non-inflicted (accidental) HI [in 69.3% and 3% of cases, respectively ( P < 0.001), with a high specificity (0.97) and a high positive predictive value (0.92)];
- ∘
- •
more suggestive, implausible explanations: for example, bruising supposedly related to a fall in an infant who cannot yet walk unaided;
- •
an explanation that changes over time or differs from one person to another;
- •
spontaneous reporting of a mild HI;
- •
a child who reportedly cries a lot or a prior consultation for crying;
- •
a history of trauma of any sort;
- •
a history of unexplained sibling death.
If the physician suspects a diagnosis of SBS, he/she must tell the parents about his/her concern for the child’s status and inform them that emergency hospitalization is indicated.
1.3.2.2
Is there a lucid interval between the shaking and the onset of symptoms?
A variety of studies have established that there is no lucid interval in most cases:
- •
Willman et al. performed a retrospective study of 95 children having suffered a fatal HI and concluded that there was no lucid interval (except for the cases with EDH);
- •
Starling et al. established that in cases where shaking (with or without impact) had been admitted, the symptoms appeared immediately after the trauma 52 times out of 57. In five cases, it was difficult to date the symptom onset but it must have been within 24 hours of the shaking;
- •
according to Biron and Shelton’s study of 52 cases of shaking investigated by the police and considered to be “serious”, the symptoms were immediate in cases with a full description.
It appears thus that in the great majority of cases of SBS (or perhaps even in all cases), shaking immediately leads to symptoms. Of course, it must be borne in mind that the consultation may take place some time after shaking has occurred.
1.3.2.3
Risk factors for abusive head injury
It is important to remember that a risk factor is a variable with a statistically significant association with a phenomenon, disease or syndrome but is not the cause.
1.3.2.3.1
Risk factors related to the child
The gender ratio: there is male predominance, with a boy/girl ratio of between 1.3 and 2.6.
Prematurity: there is a higher proportion of premature infants among SBS victims (11 to 21%, with 11% in the series reported by Mireau ) than among the general population (7 to 8%).
Multiple pregnancies are more frequent in SBS (in 5% of cases reported by Mireau ) than in the general population (1.5% of all births).
Crying cannot be considered as a risk factor per se but may trigger abuse of the infant , given that parents’ tolerance of crying in a child is very variable. A consultation for crying in a young baby should not only search for the cause but also evaluate the parents’ feelings and reactions.
1.3.2.3.2
Risk factors related to the shaker
In cases where the perpetrator has been identified (regardless of whether he/she has admitted the act), the latter is usually (70%) male (more often the child’s father than the mother’s partner).
Unrelated adults also constitute a significant category of potential shakers: in the series of 151 AHI cases examined by Starling’s group , the mother’s partner was implicated in 20.5% of cases and a female carer/babysitter was implicated in 17.3% of cases.
1.3.2.3.3
Risk factors related to the parents
In terms of the socio-economic context, the results are very contradictory. All backgrounds are concerned by SBS but the suggested vulnerability factors remain to be documented (a first child, a new pregnancy, a return to work, poor knowledge of a child’s needs or normal behaviour, social and family isolation, a history of domestic violence, past or current psychiatric disorders, drug or alcohol abuse, etc.). In 2005, Mireau noted that the parents had very poor knowledge of a child’s needs or normal behaviour. Low parental age is frequently emphasized by researchers and has been reported as a potential risk factor .
A prospective study examined the socio-economic context of 25 cases of non-accidental HI observed over almost 10 years (January 1998 to September 2006) in a region of Scotland: 76% of the cases came from the most deprived areas in terms of education, learning and social capacities, with 72% in areas with the highest crime rates, 68% in areas with poor healthcare facilities, 60% in low-income areas, 52% in areas with poor housing and 48% in areas with high unemployment.
These results are in sharp contrast to those of earlier studies: of the two studies published in 2000 on the same cohort of children, one noted that most parents had a stable job (81% of the mothers were in work) and the other found that the majority of the parents had been in secondary or higher education.
Ruling out a diagnosis of AHI because of an apparently favourable sociofamilial context may lead to so-called “missed” diagnoses .
However, in general, a healthcare professional should pay attention to a difficult sociofamilial context for the child’s carers.
The relationship between SBS and ethnic factors has been studied. Fortin reviewed the literature on this topic and concluded that ethnic origin is no more significantly associated with SBS than it is with accidental HI. In fact, the data suggested rather that the “ethnic origin” parameter constituted a risk factor for other social markers that increased in the risk of AHI in the child.
In summary , the currently available data (although fragmented and sometimes contradictory) suggest that children who are male, first born, aged under 6 months, born prematurely after a complicated or multiple pregnancy, living with parents with a history of psychoactive substance abuse (alcohol, drugs) or family violence and/or with poor knowledge of strategies for managing the relationship with their infant are at a greater risk of being SBS victims. Of course, this violent act can occur in the absence of any socio-economic and cultural risk factors. Even though it is right to consider that SBS victims are more likely to belong to one or more of the above-mentioned risk groups, it is wrong to believe that the majority of children presenting these characteristics are victims of this type of abuse.
1.3.3
What types of lesions occur and which clinical and paraclinical assessments are necessary and sufficient to detect them?
1.3.3.1
The lesions
1.3.3.1.1
The meninges (with subdural or subarachnoid haemorrhage), the brain, the eyes and the spinal cord are likely to be damaged in SBS
Other lesions may also be observed: fractures of the limbs, ribs or skull; bruising of the scalp, hematoma of the neck muscles and posterior spinal lesions.
Although the most detailed data have been provided by autopsy series, the latter obviously correspond to the most serious forms of SBS because they have led to the child’s death.
On the basis of 93 neuropathological examinations of SBS victims lacking visible cranial trauma, Billette described:
- •
81 cases of subdural hematoma (SDH), 65 cases of subarachnoid haemorrhage, 14 cases of intraparenchymatous haemorrhage, 69 cases of brain oedema and 41 cases of cerebral herniation;
- •
56 cases of intraocular haemorrhage;
- •
21 spinal cord lesions.
The state of the spine was not mentioned. The lesions observed here were not specific for the mechanism of death.
Another study found cervical epidural haemorrhages and focal axonal lesions of the brain stem and the roots of the spinal nerves in 11 of 37 AHI cases and in none of 14 control cases (i.e. deaths from other causes).
Different types of damage to the brain parenchyma can be observed:
- •
anoxic lesions of the cortex, grey nuclei and thalamus: these lesions translate into (rarely haemorrhagic) hypodensities associated with a loss of contrast between white matter and grey matter ;
- •
brain oedema, translating into a decrease in the volume of liquid-filled spaces;
- •
contusions, in particular in the frontal and temporal regions and at the white matter–grey matter junction.
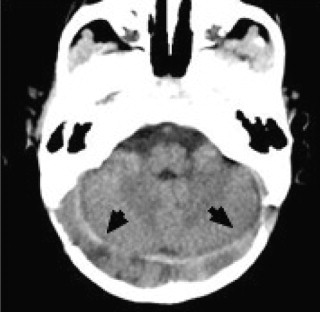
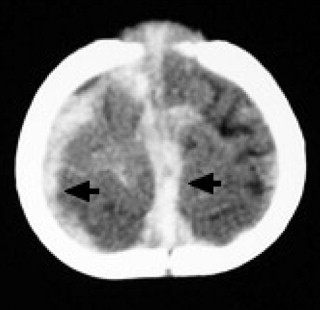
Intracranial extra-axial, blood collections (SDH, potentially combined with subarachnoid haemorrhage) present some particular features in SBS ( Figs. 1–3 ). They are generally multifocal, bilateral and faint (with no mass effect). They cover the convexity of the brain hemispheres and accumulate in the longitudinal fissure in an inclined position and along the insertion of the tentorium cerebelli. The detection of a haemorrhage in the falx cerebri is very suggestive of SBS , as are subdural collections in the posterior fossa. It is nevertheless noteworthy that SDH is not observed in all shaken babies: it was only seen in 72–93% of the cases in the articles reviewed by Christophe .

EDH results more from accidental HI than SBS, where it is extremely rare.
1.3.3.1.2
Eye lesions
RHs are NOT always present in SBS: according to Defoort-Dhellemmes , they are seen in about 80% of cases (ranging from 50 to 100%, depending on the series). They are described in terms of:
- •
whether they are bilateral or not: most are bilateral, which contrasts with the generally unilateral RH that can be observed in accidental HI . Nevertheless, RH are unilateral in 10 to 17% of cases of SBS;
- •
their appearance, size (small, large, more or less than two optic discs) and shape (flame-shaped, blots, punctiform, dome-shaped), which depend on their location in the eye;
- •
their location at the posterior pole of the eye (peripapillar, macular, along the vascular arcades) or at the periphery of the fundus (near to the periphery or extending out across the very edge to the ora serrata);
- •
their location relative to the retinal layers ( Table 2 ):
- ∘
dome-shaped, preretinal haemorrhages situated just under the internal limiting membrane, whether small (classic, pearl-shaped RH) or large (haemorrhagic retinoschisis),
- ∘
superficial haemorrhages (that disappear very rapidly, sometimes in less than 24 hours) or deep intraretinal haemorrhages,
- ∘
subretinal haemorrhages.
- ∘
| Preretinal haemorrhages | Dome-shaped, small (< 1 optic disc diameter) |
| Dome-shaped, large (> 1 optic disc diameter) | |
| Haemorrhagic retinoschisis | |
| Intraretinal haemorrhages | Superficial intraretinal |
| Deep intraretinal | |
| Subretinal haemorrhages | |
Defoort-Dhellemmes distinguishes between three types of RH, depending on their number and their extent ( Table 3 ):
- •
type 1: intraretinal haemorrhages, flame-shaped, blots or punctiform, situated at the posterior pole of the eye;
- •
type 2: preretinal dome-shaped haemorrhages that are small (no larger than the diameter of the optic disc) and pearl-shaped, situated at the posterior pole, around the optic disk and along the vascular arcades or mid-way out towards the periphery. These haemorrhages may occur alone or in combination with type 1 RH;
- •
type 3: profuse, multiple haemorrhages of all types (intra-, pre- or subretinal), coating the whole retina or flecked out to its periphery, combined with unilateral or bilateral premacular haemorrhagic plaques (which are sometimes immediately suggestive of haemorrhagic retinoschisis). Type 3 haemorrhages are extremely suggestive of SBS. They can be considered as almost pathognomonic, especially when combined with SDH, massive brain oedema or bone lesions that are very suggestive of abuse. However, they can be observed extremely rarely in violent, accidental HI (road accidents).
| Type 1 | Intraretinal haemorrhage (flame-shaped, blots or punctiform, situated at the posterior pole of the eye |
| Type 2 | Small, dome-shaped, preretinal haemorrhage, situated at the posterior pole of the eye, around the optic disk and along the vascular arcades or mid-way out towards the periphery. They may occur in isolation or in combination with Type 1 RH |
| Type 3 | Profuse, multiple haemorrhages of all types (intra-, pre- or subretinal) coating the whole retina or flecked out to its periphery, combined with unilateral or bilateral premacular haemorrhagic plaques |
Other lesions can be seen in the fundus: vitreous matter and choroidal haemorrhage and papillary oedema due to intracranial hypertension.
Intra-orbital haemorrhage (scleral haemorrhage and haemorrhage of the optic nerve sheath, muscles and orbital fat) can be detected on autopsy .
1.3.3.1.3
Lesions of the neck muscles, spine or spinal cord
Neck damage was noted in 4% of the children studied by King et al. . Billette reported that several observations of spinal cord SDH have been described in the literature. Christophe pointed out that violent shaking can provoke: (i) widespread axonal lesions near the brain stem and the upper spinal cord and (ii) epidural haematoma near the neck/head junction.
1.3.3.1.4
Skin lesions
In the absence of medical causes, bruising is very suggestive of abuse in an infant that cannot yet walk unaided . In the latter article, only 0.6% of the children under 6 months and 1.7% of the children under 9 months of age had one or several bruises. It is particularly important to look for bruising on the scalp: in a study on HI in infants, Greenes and Schutzman found that 93% of the infants presenting bruising of the scalp also had intracranial lesions.
1.3.3.1.5
Bone lesions
Bone lesions are particularly suggestive of abuse:
- •
rib fractures (in the absence of prior, aggressive, respiratory physiotherapy) are posterior, at the costovertebral junction. There are generally multiple fractures on contiguous, symmetric ribs;
- •
metaphyseal fractures;
- •
periosteal spurs;
- •
some skull fractures: multiple fractures and depressed occipital fractures.
1.3.3.2
Clinical and paraclinical assessments
1.3.3.2.1
Clinical assessments
Check and update the height, weight and head circumference curves.
Thorough clinical screening for trauma, which must be photographed if found.
A neurological examination is, of course, essential; one should note the head circumference (in comparison with earlier figures), the state of the fontanel, axial tone and possible motor impairments.
1.3.3.2.2
Additional assessments
When faced with neurological clinical signs or a combination of the signs described above, the following additional examinations are required:
- •
a computed tomography (CT) brain scan is the first-line examination in an emergency . It is a sensitive method for detecting haemorrhagic lesions: SDH, subarachnoid haemorrhage and (more rarely) haemorrhages of the brain parenchyma. The brain scan can also define the extent of any oedema. If symptoms persist (and even when the first scan is normal) a second scan can be performed 12 to 24 hours later;
- •
an ophthalmological examination: it must be performed after dilatation, by an experienced ophthalmologist, within 48 to 72 hours at the latest (due to the rapid resorption of some types of RH). Photos must be taken whenever possible;
- •
the value of MRI:
- ∘
when performed in the acute phase as soon as permitted by the child’s state, MRI is of significant diagnostic value for revealing lesions that are not visible on CT (i.e. small SDH, oedema and hypoxic lesions). Performance of an MRI scan depends on the child’s clinical state (stability). This is the examination of choice for having a complete overview of axial and extra-axial lesions, whether haemorrhagic or not . MRI enables the brain stem, spinal cord and neck region to be assessed, in addition to the brain itself.
Kemp et al. reviewed the literature on children with severe spinal cord damage (24 children described by 15 studies) and recommended that head and neck MRI should be performed in any infant in whom HI is suspected, especially if there is unexplained deformation of the spine, focal neurological signs or skeletal lesions.
Useful conventional sequences include the T1- and T2-weighted spin-echo sequences and the T2* echo gradient sequence. All are sensitive to the paramagnetic effect of the haemoglobin degradation products and enable determination of the approximate age of intraparenchymatous haemorrhage.
The fluid-attenuated inversion recovery (FLAIR) sequence is very good for detecting subarachnoid haemorrhage and small SDH .
So-called “advanced” techniques (such as magnetic susceptibility imaging, spectroscopy and diffusion imaging) have further increased the sensitivity and the diagnostic and prognostic value of MRI:
- –
magnetic susceptibility imaging can visualize very small areas of bleeding, whether recent or old ,
- –
spectroscopy can provide information on anatomical and functional damage to neurons and axons ,
- –
diffusion imaging can estimate changes in the volume and configuration of extracellular spaces and/or intracellular viscosity ,
- –
studies on SBS have demonstrated that early anomalies in diffusion imaging are compatible with cytotoxic-type oedema – probably as part of an associated ischaemic, hypoxic encephalopathy ;
- –
- ∘
it is less urgent to perform MRI as part of the lesion screening process but it must be performed before discharge from hospital. The brain stem, spine and spinal cord must be studied and not just the brain. Furthermore, the MRI can reveal hypoxic lesions and lesions of different ages;
- ∘
- •
other necessary examinations:
- ∘
a complete blood count + platelet count, PT, APTT, coagulation factors,
- ∘
X-rays of the whole skeleton, performed according to the American Academy of Pediatrics guidelines . A skeletal survey is mandatory in all cases of suspected physical abuse in children younger than 2 years (not a “whole body” X-ray): radiographies of the axial skeleton (anteroposterior and lateral views of the thorax, and possibly an oblique view to see the ribs, the upper dorsal and lumbar spine; anteroposterior and lateral views of the pelvis, in order to see the medial lumbar spine; a lateral view of the lumbosacral spine, anteroposterior and lateral views of the cervical spine, anteroposterior and lateral views of the skull [and other views, if necessary]) and all limb segments. One should thus screen for recent or older fractures – particularly in the locations suggestive of SBS cited earlier.
There are then three possibilities: the bone lesions are (i) very suggestive of abuse or (ii) not typical or (iii) absent. In the last two cases and if abuse is strongly suspected, scintigraphic examination can reveal lesions that are not visible on X-rays (e.g. rib fractures that do not yet show callus formation, very small diaphyseal fractures and early periosteal thickening). Another option (if the child can be placed in a safe environment) is to repeat the skeletal X-rays 10 or 15 days later and see whether there are any changes .
- ∘
If the child is dead on admission to the hospital, the family/carers must be questioned as to any abnormal signs in the hours or days before death. In February 2007, the French National Authority for Health (HAS) recommended performing the following examinations (in addition to an analysis of the circumstances in which the child was found and the medical history) in all cases of unexpected infant death: a thorough clinical examination, a fundoscopy and an X-ray examinations by a paediatric radiologist (X-rays of the skull, spine, pelvis, all four limbs and the thorax) and CT or MRI imaging of the brain and, if possible, the whole body. Autopsy is essential but requires the parents’ consent (unless otherwise decided by the district prosecutor for forensic and legal reasons) and so must always be suggested. It must include a fundoscopy and a neuropathological examination of the brain, eyes and spinal cord. Several authors have described autopsy techniques in the young child . Ehrlich et al. insist on the need to evidence rupture of the corticodural veins. Several techniques for this have been suggested .
Some time after shaking, certain neurological or neuropsychological symptoms and some neuroradiological images can suggest shaking a posteriori. It is then necessary to look for a drop in the head circumference curve (at this stage, microcephaly is observed) and perform MRI.
1.3.4
What are the differential diagnoses for shaking and which clinical and paraclinical assessments are necessary and sufficient for an aetiological diagnosis?
1.3.4.1
The main differential diagnosis is accidental HI. Rarer, disease-related diagnoses must be ruled out
1.3.4.1.1
Disorders of haemostasis
Congenital coagulation disorders (factor V, X or XIII deficiencies and haemophilia A) can lead to intraparenchymatous or extra-axial haemorrhage .
Severe thrombopenia can lead to intracranial haemorrhage (mainly intraparenchymatous haemorrhage).
1.3.4.1.2
Arteriovenous malformations
These are extremely rare below the age of 1 year and trigger subarachnoid haemorrhage (often associated with an intracerebral or intraventricular haemorrhage) rather than subdural haemorrhage.
1.3.4.1.3
Metabolic diseases
Depending on the context, one must screen for:
- •
type 1 glutaric aciduria: 1 in 30,000 births. This condition often manifests itself by acute neurological distress in the first months of life, with a pseudoencephalitic clinical picture in children with macrocephaly and pre-existing hypotonia. Imaging can reveal suggestive anomalies: a broad lateral sulcus and lesions in the central grey nuclei. During disease progression, SDH is frequent and RHs are reported in 20 to 30% of cases . Faced with this characteristic clinical and radiological picture, a diagnosis of this metabolic disease is confirmed by the chromatographic assay of urinary organic acids ;
- •
Menkes disease: this affects boys only (as a recessive, X-linked disease) and is also rare (1 per 250,000–300,000 births). It is a metabolic disease of copper absorption and induces multiple bone lesions, SDH , hypotonia, early convulsions and severe mental retardation in children surviving beyond the neonatal period. The twisted appearance of the hair is suggestive. Serum copper and ceruloplasmin assays make a biochemical diagnosis very easy.
1.3.4.1.4
Osteogenesis imperfecta
Two articles have stated that SDH is possible in this syndrome but did not indicate its frequency and a causal relationship has not been established. The clinical picture is quite different; the constitutive bone fragility results in diaphyseal fractures and not metaphyseal damage.
1.3.4.2
Are retinal haemorrhages required for diagnosis of SBS?
RHs are observed in about 80% of cases of AHI, on average (with values ranging from 50 to 100%, depending on the series).
In fact, the frequency of RH is difficult to estimate because:
- •
as reported in the literature, the frequency increases when the fundoscopy is performed by a senior ophthalmologist on admission to the emergency room, after dilatation or when photos (taken on admission by specialists in paediatric resuscitation) show these haemorrhages;
- •
many ophthalmologic studies consider their presence to be necessary for the diagnosis of SBS – thus introducing circularity bias because the RH is both the subject of the study and an obligatory diagnostic criterion.
One can nevertheless conclude that RH (absent in about 20% of the cases reported by Defoort-Dhellemmes ) are not essential for a diagnosis of SBS. In accidental HI due to road accidents, RHs are much rarer (ranging from 0 to 17%, with a frequency of 8.9% for all the literature cases collated by Kivlin et al. ). However, their frequency has certainly been underestimated, since fundoscopy is not performed systematically in child victims of road accidents or may be performed too late. The most frequent RH in accidental HI corresponds to type 1 and 2 in Defoort-Dhellemmes’ classification and disappear rapidly – sometimes in less than 2 days .
1.3.4.3
Clinical criteria for a diagnosis of shaking
This question can be addressed from two standpoints:
- •
according to the clinical situation;
- •
according to the lesions found upon examination.
1.3.4.3.1
Different clinical situations can suggest a diagnosis of SBS
When an infant is brought in dead and does not correspond to terminal progression of a known pathology , a diagnosis of AHI must always be considered as a potential cause of unexpected death. The interview with the family must be performed with respect but must also be detailed, in order to establish the circumstances surrounding the death.
Some signs must be given special attention:
- •
implausible explanations;
- •
statements that change over time (although the parents’ emotional state can be an explanation);
- •
suspicion of previous abuse and other poorly explained deaths in the family.
For all cases of unexpected infant death, it is advisable to obtain the parents’ consent for an autopsy that will potentially enable collection of data on shaking (bearing in mind that any indication of SBS should be reported to the district prosecutor, who will be able to order an autopsy as part of a forensic procedure).
When faced with inaugural, acute, neurological distress , the clinician should perform a brain CT scan as soon as possible and, if intracranial haemorrhage is evidenced, look for the simultaneous presence of other signs of shaking:
- •
RH;
- •
signs of abuse (skin and/or bone lesions);
- •
explanations given by the family that are implausible or change over time.
If all these signs are found together, the diagnosis of SBS is highly probable, or even certain.
When faced with signs that strongly suggest neurological damage , such as those described above (changes in behaviour, poor food intake, poor contact, less smiling, decrease in the child’s capabilities; change in tone [axial hypotonia] or certain non-specific signs (vomiting, respiratory disorders [pauses, apnoea], pallor or an infant who appears to be in pain), it is essential to consider shaking:
- •
palpation of the fontanel, measurement of the head circumference and examination of the growth curve (acts that must always be performed when examining an infant) can evidence a bulging fontanel and enlargement of the skull with a sharp upwards shift on the head circumference curve;
- •
look for:
- ∘
a combination of the above-mentioned signs ( Table 1 ), found in a significant percentage of cases of shaking,
- ∘
other signs of abuse via clinical examination and analysis of the medical history;
- ∘
- •
note during the interview:
- ∘
the existence of any delay in seeking medical care,
- ∘
the fact that the explanations given by the family/carers are implausible, barely plausible or change over time or from one person to another;
- ∘
- •
look for RH;
- •
perform a brain CT scan immediately (MRI being performed later, when permitted by the child’s state).
Some of these elements may be absent and it is impossible (given our current state of knowledge) to assess the relative importance of each of those elements present. However, certain data have more specific value:
- •
in clinical terms: in addition to the interview data, the existence of apnoea, bruising (on the scalp or elsewhere);
- •
the CT results: subdural or subarachnoid haemorrhages are more frequent (refer to the description above) than intraparenchymatous bleeding and EDH is extremely rare in cases of SBS;
- •
the fundoscopy: the existence of RH of all types (even on one side only; Table 3 ), especially when profuse or flecked across the retina to the outer periphery, combined with one or several large, dome-shaped or plaque-shaped haemorrhages (sometimes with the characteristic aspect of haemorrhagic retinoschisis) or a perimacular retinal fold (Defoort-Dhellemmes type 3, which is almost completely pathognomonic for SBS).
One of these signs alone will not enable the physician to affirm a diagnosis of SBS. The combination of two or more of these signs is strongly suggestive, as long as differential diagnoses have been ruled out. The description of an act of shaking (sometimes by the perpetrator but more often by an eye witness) is, of course, a key element.
In any case, any suspicion of shaking must prompt the physician to tell the parents about his/her concern and the absolute need to hospitalize the child.
1.3.4.3.2
At the end of the clinical and radiological assessments (whatever the initial symptoms), the probability of a diagnosis of SBS will vary according to the lesions observed
In a child under 1 year of age and after having ruled out differential diagnoses:
- •
a diagnosis of shaking is highly probable (or even certain) in cases with:
- ∘
multifocal extra-axial haemorrhages (SDH, subarachnoid haemorrhage) ( Figs. 1–3 ),
- ∘
AND RH that is profuse or flecked across the retina out to its periphery (Defoort-Dhellemmes type 3) ( Table 3 ),
- ∘
AND a clinical history that is absent, incoherent, changes over time or is incompatible with the observed lesions or the child’s age.
The coexistence of these three diagnostic elements (as described here) prompts a diagnosis of AHI (probably by shaking).
Other elements can be present and reinforce the diagnosis of shaking:
- –
hypoxic brain lesions,
- –
cervical lesions (spinal canal haematoma, spinal cord lesions and lesions of the occipitovertebral or cervicodorsal junctions),
- –
description of violent shaking by an eye witness;
- –
- ∘
- •
a diagnosis of shaking is probable in cases with:
- ∘
EITHER multifocal extra-axial haemorrhages ( Figs. 1–3 ), in the presence or absence of RH of any type ( Table 3 ),
- ∘
OR localized extra-axial haemorrhage with type 2 or 3 RH,
- ∘
AND a clinical history that is absent, incoherent, changes over time or is incompatible with the observed lesions or the child’s age;
- ∘
- •
in cases of localized SDH and RH limited to the posterior pole (type 1 RH), with a clinical history that is absent, incoherent, changes over time or is incompatible with the lesions observed or the child’s age, there was no consensus within the Hearing Commission as to whether diagnosis of shaking must be considered as probable or possible;
- •
a diagnosis of shaking is possible in cases with:
- ∘
localized SDH,
- ∘
AND a clinical history that is absent, incoherent, changes over time or is incompatible with the observed lesions or the child’s age;
- ∘
- •
a diagnosis of shaking can be ruled out in cases with:
- ∘
localized SDH ( Fig. 4 ), with a linear fracture and adjacent bruising in some cases,
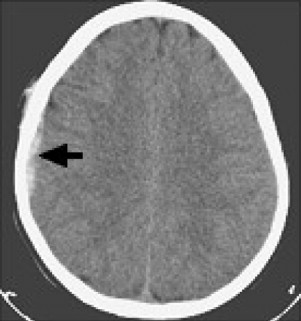
Fig. 4
Localized right frontoparietal SDH and adjacent bruising of the scalp (indicated by an arrow) in a case of accidental head injury (HI).
- ∘
AND an unchanging clinical history compatible with the observed lesions and the child’s age and which features a description of a violent, accidental HI.
- ∘
In all cases, the observation of any of the following is strongly suggestive of a diagnosis of abuse and should prompt the implementation of appropriate measures:
- •
abuse-specific bone lesions and bruising (particularly on the scalp) in a child too young to walk unaided;
- •
a history of abuse, or of unexpected poorly explained sibling death(s);
- •
a delay in seeking medical assistance.
1.4
The causal mechanism of lesions
1.4.1
In the presence of subdural haematoma (in the presence or absence of subarachnoid haemorrhage) and retinal haemorrhage (alone or combined), which causal mechanisms or circumstances may be invoked?
Since the lesions observed in SBS are not highly specific (even though some are highly suggestive), it is important to determine which lesions can be observed during activities frequently invoked by the adults when a child is brought to hospital after denied shaking. The most frequent explanations are falls and attempts to resuscitate the infant after loss of consciousness. Indeed, some people consider that shaking alone is not sufficient to create lesions and that an accompanying impact is essential. This is why the following question is dealt with here, with a view to facilitating the diagnosis of SBS: which mechanisms or circumstances may be involved in the occurrence of SDH (in the presence or absence of subarachnoid haemorrhage) and RH (alone or in combination)?
The following mechanisms and circumstances are discussed below:
- •
shaking in the absence of an impact;
- •
mild HI by fall from a low height;
- •
playing;
- •
childbirth;
- •
hypoxia or anoxia;
- •
resuscitation manoeuvres.
1.4.1.1
Shaking in the absence of an impact
1.4.1.1.1
Subdural haematoma
Biomechanical evidence.– In their first study in 1987, Duhaime et al. estimated that shaking in the absence of an impact could not cause brain lesions or SDH. However, the reference values used in the study had been obtained in primates and the transposition to infants had not been validated.
Some more recent biomechanical studies have indicated that shaking in the absence of an impact is sufficient to rupture the corticodural veins. Roth et al. , by using a finite element model of the infant head to show that even though the pressure and shearing values are significantly higher in cases of impact, the relative extension of the corticodural veins is similar in the presence and absence of impact (180%) and exceeds the degree of stretching need to rupture the said veins in children under 3 months of age (150%) .
Clinical evidence.– Several clinical studies have confirmed that SDH may be caused by shaking in the absence of an impact . Moreover, SDH are more frequent in confirmed cases of AHI by shaking than in accidental HI in children of the same age .
Autopsy data.– Autopsy data confirm also the existence of SDH in the absence of any signs of external impact .
In conclusion.– There are sufficiently clinical, radiological, autopsy and biomechanical arguments to affirm that SDH can occur with shaking in the absence of any impact.
1.4.1.1.2
Retinal haemorrhage
Shaking in the absence of an impact can cause RH. In fact, RHs seem more strongly linked to the mechanism of shaking than to the occurrence of an impact.
Biomechanical elements.– Modelling of the infant eye has shown that during shaking, significant stress is applied to the posterior pole as a result of the strong traction exerted by the optic nerve on the retina. This explains the predominance of lesions to the posterior part of the retina .
Clinical elements.– RHs are found in cases of SBS both with and without cranial impacts and may be even more frequent during shaking alone (in the absence of an evidenced impact) .
Further evidence in favour of a link between the shearing mechanism and RH is the fact that in cases of AHI (compared with accidental HI), RH are:
- •
more frequent: 80%, on average (ranging from 50 to 100%, depending on the study) in cases of shaking vs. 8.9% on average for all the cases in the literature on road accidents collated by Kivlin et al. ;
- •
bilateral in the great majority of cases (83 to 90%) ;
- •
often more abundant ;
- •
more abundant in cases of certain SBS than in cases of probable SBS ( P < 0.0001) .
Type 3 RH extending out to the periphery are extremely rare after accidental HI:
- •
they are extremely rare in road accidents ;
- •
they have been reported only five times in other circumstances that were not simple falls (a television set or a 63 kg person falling on the child’s head; a child falling off a platform in a play area ), some of which are controversial because there were no independent eye witnesses, no autopsy data and no fundoscopy data from an ophthalmologist .
According to Betz et al. , massive RH covering more than 20 to 30% of the whole retina’s surface area cannot be explained by a simple, accidental HI and a banal fall in particular. According to Defoort-Dhellemmes , type 3 RH are considered as almost pathognomonic for shaking .
In conclusion.– Type 3 RH (but also types 1 and 2 RH) can occur during shaking in the absence of an impact and seem even more related to the mechanism of shaking than to the existence of an impact.
Type 3 RH are extremely rare in other circumstances and are thus almost pathognomonic for shaking.
1.4.1.2
Mild head injury: falls from a low height
In the absence of a formal definition of “mild” injury, examples of trauma considered to be mild (falls from a low height, in particular) and for which some evidence exists in the scientific literature have been extrapolated.
1.4.1.2.1
Falls are the main explanation given by adults
It is particularly important to study the mechanism of falls because the latter explanation is that most frequently alleged by adults to justify the lesions observed in an infant .
It is probably often accepted in error in the absence of other plausible explanations, as very strongly suggested by several studies:
- •
in 1991, Chadwick et al. reviewed the medical records of 317 consecutive admissions to a children’s trauma centre in San Diego between 1984 and 1988, for which a history of a fall was reported by the parents as being the cause of HI. The researchers analysed the data on the history as reported and did not evaluate their probability or credibility with respect to the diagnosis and the outcome. For the 283 children for whom the height of the fall was known, they found 7% of deaths for falls reportedly from a height of less than 1 metre (7 out of 100), compared with a rate mortality of 0% for falls from a height of between 1 and 3 m (0 out of 65) and of 0.8% for falls from a height of between 3 and 12 m (1 out of 118). The age of the child was not always specified but of the seven deaths for alleged falls from a height of less than 1 metre, two children had fallen from their own height (and thus were under the age of four because a 4-year-old is 1 metre tall, on average), two had fallen from a bed or a table (which suggests a young age) and two children (aged 6 weeks and 13 months) had fallen from someone’s arms. Lastly, the remaining case (an 11-month-old child) had fallen down the stairs;
- •
in a prospective study of 398 falls by children admitted to Oakland Children’s Hospital over a 2-year period, Williams compared two populations of under-3s for whom the alleged causal mechanism was either a fall reported by family members or carers (53 cases) or by a neutral eye witness or several eye witnesses (106 cases). The researchers observed a death rate of 3.8% and a serious HI rate of 34% for cases with related eye witnesses and no deaths (other than a child who fell 21 m) and no serious HIs for cases with neutral or several eye witnesses;
- •
in an editorial , Chadwick insisted on the fact that reliably witnessed cases in mechanistic studies are those occurring in hospital or an authorized care setting under certain conditions. He considered that cases for which the eye witnesses are carers or other children should not be included in databases concerning alleged mechanisms.
1.4.1.2.2
Mortality due to falls from a low height
In the child under 5 years of age, the immediate or differed mortality rate after a fall from a low height (< 1.5 m) is very low:
- •
on the basis of a review of three databases in the United States, five book chapters, the work of two learned societies, seven literature reviews and 177 articles published in peer-reviewed journals, Chadwick et al. estimated the mortality rate at less than 0.48 per million under-5s per year (some cases were included in this study despite doubtful circumstances of occurrence). The estimation of the incidence under the age of 1 year was not specified;
- •
in five studies, none of the 708 children who fell in a hospital setting (at least 94 of whom were under the age of one) died .
Denton and Mileusnic published the case of a 9-month-old child (looked after by its grandmother) who died 72 hours after a backwards fall from a 76-cm-high bed where it was sitting. The child (which did not have any clinical symptoms until the evening before death) was found dead in the morning. The autopsy evidenced mild parenchymatous brain lesions and slight SDH above a linear parietal fracture, without disjunction of the edges in spite of massive brain oedema (1035 g for an expected weight of 750 g). There were no RHs. However, this case (not considered by Chadwick et al. as resulting from a fall from a low height) cannot be taken into account since (i) the eye witness was not neutral and (ii) the absence of disjunction of the sutures (despite a large oedema) argues in favour of a very recent HI – which casts doubt on the alleged mechanism of a fall from a low height.
The article by Plunkett on 75,000 playground accident reports over a period of 11.5 years showed that death is possible but extremely rare after a fall from a low height. Eighteen children (0.024%) aged from 12 months to 13 years had died “following a fall from playground equipment from a height of between 0.6 to 3 m” (the height was judged in terms of the part of the body nearest to the ground at the time of the fall, rather than the distance above ground of the child’s centre of gravity). However, the following points must be noted for the eight deaths of children aged three or under (cases 1 to 8):
- •
none of the children was under 1 year of age and the four youngest cases (cases 1 to 4) were 12 to 20 months old;
- •
the eye witnesses were either family members in five of the eight cases (cases 1 to 4 and 6). This was particularly the case for the four youngest children and one other child (case 8);
- •
an autopsy was not performed in three cases (cases 1, 2 and 7). In a fourth case (case 4), the autopsy was “limited”;
- •
only one of the four youngest children received a full autopsy (case 3);
- •
being swung or rocked was associated with the fall in three of the eight cases (cases 1, 3 and 6), including two of the four youngest children;
- •
the lucid interval between the fall and the first symptoms was always less than 15 minutes and was even zero in three cases (cases 1, 3 and 6);
- •
brain oedema was indicated as the cause of death – even for cases lacking an autopsy.
In the eight youngest children in this series, only case 5 (a 23-month-old child having fallen over a barrier around a platform situated 0.7 m above the ground) appears to be an incontestable HI due to a fall from a low height (a filmed case, with an autopsy). There was a 10-minute lucid interval before coma. The lesions observed before death were:
- •
bilateral RH evidenced 24 hours after admission but with no other details (the fundoscopy was not performed by an ophthalmologist) and not described later at autopsy either;
- •
a large right SDH with disappearance of the lateral ventricle and mild subfalcine herniation on the initial CT scan. Soft tissues were not studied. The SDH had been evacuated.
At autopsy, the following were found:
- •
a right frontal impact;
- •
a small residual SDH;
- •
a right parietal parenchymatous contusion;
- •
brain oedema with cerebellar herniation.
The low risk of death by falling from a low height is emphasized by the fact that even falls from a great height have a very low mortality rate:
- •
two studies found no deaths for falls from heights of less than three storeys:
- ∘
Smith et al. : a study on falls from three storeys or less by 70 children aged from 10 months to 15 years (50% of whom were under 3 years of age),
- ∘
Barlow et al. : 61 children under 16 years of age;
- ∘
- •
in the series by Chadwick et al. , only one of the 118 children admitted after a fall from more than 3 m died (it was 11 months old). None of the 65 children having fallen from 1 to 3 m died.
1.4.1.2.3
Which clinical signs result from falls from a low height?
A few studies provide reliable data falls from a low height (corresponding to a mild HI) that have occurred in well-established circumstances (as observed by objective or several eye witnesses):
- •
five studies concerning falls of hospitalized children found the same results: no deaths and one case with vigilance disorders (a neonate having fallen 1 m off a delivery table) among 708 children in total, including 493 children under the age of seven. On the basis of the details given by the articles, one can establish that at least 94 of the children were under the age of one ;
- •
a prospective study of 106 children under 3 years of age with neutral eye witnesses did not find any serious clinical manifestations (bruising, abrasions, cuts or neurological disorders) and found only three skull fractures without loss of consciousness (a fall against a hard edge) for falls from a height of less than 1.5 m;
- •
other data came from questionnaires put to parents on possible previous falls and consequences. Kravitz et al. questioned the mothers of children under 1 year of age ( n = 536) and established that over half of these children had fallen from a low height at some moment in their life, with very few serious injuries and no fatalities . Fifteen children had been hospitalized. The reported symptoms were lethargy in 14 cases, a loss of consciousness in two cases, vomiting in eight cases and convulsions in two cases. The total number of consultations has not been indicated;
- •
of 3357 falls (including 97% concerning the head) in 2554 children monitored longitudinally from birth to the age of 6 months, an injury was reported in 437 cases (as bruising in 244 cases and as a fracture or mild HI [commotion] in less than 1% of cases [21 times]) .
On the basis of these studies, it is clear that a fall from a height of 1.5 m hardly ever leads to death (fewer than 0.48 per million under-5s per year ) and rarely produces clinical signs.
1.4.1.2.4
Can subdural haematomas be observed after falls from a low height?
Available data.– A few articles are available:
- •
on the basis of two studies of infant death [first study: 63 accidental deaths, including 10 by accidental HI and six by falls, excluding deaths due to drowning, fires, burns and road accidents, with 25 (39%) children under 1 year of age, 18 (28%) between 1 and 2 years of age and five (8%) between 2 and 3 years of age; second study: 21 accidental deaths, including two due to HI and with nine children (43%) under 1 year of age] performed in a city with two million inhabitants over a 24-year period (1975 to 1985 and 1986 to 1999) and other studies in the literature, Case concluded that in cases of falls from a height of less than 1.8 m (6 feet), fractures of the skull were observed in 1 to 3% of cases. The factures are generally linear and are not accompanied by intracranial haemorrhage or neurological impairments. Fewer than 1% of these fractures caused EDH (1–3 per 10,000) and even fewer caused a contact subdural haemorrhage. When these haemorrhages are sufficiently voluminous to create a mass effect, death can occur by intracranial hypertension. In all these cases, the EDH and SDH were focal and were situated at or adjacent to the fracture;
- •
based on his experience and a literature review, Dias found that:
- ∘
falls from a height of less than 1.5 m (5 feet) can cause intracranial damage, albeit very rarely (usually skull fractures, EDH and subarachnoid haemorrhage but also localised SDH),
- ∘
diffuse SDH and brain hypodensities “are extraordinarily rare if they exist at all” (Dias did not find any case reports),
- ∘
the lesions are often silent or poorly symptomatic and do not leave sequelae,
- ∘
falls from a low height are even less likely to be lethal. Sixty-seven to 75% of the deaths were due to lesions with a mass effect (EDH, SDH);
- ∘
- •
Matschke et al. found just one case of SDH due to accidental HI (a road accident) in a study of 715 consecutive autopsies of children under 1 year of age [with deaths due to malformation (almost 300), perinatal complications (175 cases), infections (under 100 cases) and metabolic damage (30 cases)]. The SDH was localized.
Biomechanical aspects.– Bertocci et al. have studied linear accelerations of the head for falls from the height of a bed onto different types of surfaces. Even though further research is still necessary to determine the lesional limits of the child (since the values obtained [55 to 418 m/s 2 ] are very much lower than the lesional threshold in the adult [900 m/s 2 ]), the work suggests that (for the falls studied) serious brain lesions (such as acute SDH or intracerebral haemorrhage) cannot occur, since the linear acceleration is too low.
Conclusions concerning SDHs.– SDH after falls from a low height are extremely rare and are localised. They are mostly adjacent to the fracture line. Given the extreme rarity of this situation, the observation of SDH after an alleged fall from a low height should prompt the healthcare professional to first consider AHI as the cause.
1.4.1.2.5
Retinal haemorrhage after a fall from a low height
Regardless of the height of the fall, RHs are rarely described in falls with one or more neutral, reliable eye witnesses.
After a fall from a low height, RHs (when observed) are never widespread in terms of either surface area or depth, as described in cases of AHI. The RHs are then more likely to be associated with an EDH and are moderate: small intraretinal or preretinal haemorrhages, situated on the posterior pole of the eye . They are usually unilateral but can be bilateral and often asymmetric (in the series reported by Defoort-Dhellemmes ).
1.4.1.2.6
Subdural haematoma and retinal haemorrhages after a fall from a low height
Christian et al. have reported three cases of traumatic SDH occurring at home, including two cases with RHs that were limited to the posterior pole (with pre-, intra- or subretinal haemorrhage) in one eye only. However, none of these cases corresponded to a fall from a low height:
- •
a fall down 13 steps by a 13-month-old child, with local signs of impact (skin contusions on the forehead, nose abrasion) and RH on the same side as the SDH;
- •
a fall through banisters onto a concrete floor by a 7-month-old child, with a skull fracture and right-side brain parenchymatous contusion but no RH;
- •
a fall suffered by a 9-month-old infant after being swung: it was stated that the father lost his grip while swinging the child in his arms. The rear of the child’s head had then hit the ground. This case cannot be considered as an example of a fall from a low height because:
- ∘
the eye witness (a family friend) was not neutral,
- ∘
the combination of swinging and a loss of grip during swinging cannot be likened to a simple fall from a low height,
- ∘
the height was very low (30 cm),
- ∘
there was no lucid interval,
- ∘
in contrast to the significant internal lesions (parieto-occipital SDH and RH), there were no external lesions, bruising or soft tissue damage observed in the other two cases to suggest an impact.
- ∘
Vinchon et al. gathered 3 years of prospective data on 150 under-2s having suffered an HI. Seventy-three cases were considered to be accidental. There were 12 road accidents. The trauma occurred at home in 55 cases and was been reported as a fall in 53 of these: 13 falls from a seat, 10 down the stairs, nine from the arms of an adult, nine from a table, eight falls when standing or from a great height and two from a bed. The eye witness (when there was one) was a family member or friend in all cases. In some cases, the traumatic nature of the incident has been deduced from the observed lesions. RHs were observed in five of the 73 children but Vinchon et al. did not state which children were concerned, how old they were and what the associated intracranial lesions were. On the basis of this article, it is impossible to identify any case of a child with both SDH and RH after a fall from a low height (especially in the absence of any neutral eye witnesses).
For the four cases of children aged between 12 to 20 months of age who died after playground accidents described by Plunkett , only one (case 4) had undergone fundoscopy and presented SDH and bilateral RH (RH in several layers). The fundoscopy had not been performed by an ophthalmologist. The eye witness was not neutral.
In summary, there are no literature cases of children under the age of one presenting both SDH and RH after a fall from a low height.
1.4.1.3
Can shaking be performed by another child?
There is only one biomechanical study on this subject . Morison asked some children aged from 3 to 15 years of age to shake masses corresponding to infants weighing 3 to 10 kg. The children under four were unable to shake 3 kg weights, those under six were unable to shake 5 kg weights, those under nine were unable to shake 7 kg weights (which corresponds to the weight of a 6-month-old child) and those under 13 were unable to shake 10 kg weights (which corresponds to the weight of a 1-year-old child). The acceleration of the shaking (when the latter was possible) was well below that generated by an adult: for example, for a 7 kg weight (corresponding to the weight of a 6-month-old child), the acceleration was estimated to be 2125 cm/s 2 , whereas shaking by an adult produces almost twice as much (3954 cm/s 2 ).
1.4.1.4
Activities considered to be play by the family or carers
Very few studies have addressed this question.
1.4.1.4.1
Biomechanical aspects
Adults sometimes mention a mechanism that involves shaking the infant in “baby bouncer” seat by an older child.
Jones et al. studied a manikin corresponding to a 5-week-old child and submitted it to rocking in a “baby bouncer” seat. The acceleration values ranged from 6 to 16 G (compared with the 50 G peak acceleration considered to be lesional, 750 G resulting from an impact against a wall and 177 G corresponding to violent shaking). Moreover, when the duration of action is taken into account, the resulting index ranged from 2 to 52 (in comparison with a value of 1000 for a 50% chance of severe neurological damage in an adult). Even though if further studies are necessary to determine the lesional limits in the child, the values obtained (2 to 52) are well below the lesional threshold in the adult (1000) and suggest that it is very likely that serious brain lesions cannot occur through shaking in a “baby bouncer” seat.
1.4.1.4.2
Clinical aspects
There are no literature reports or expert feedback on any cases of HI with RH or SDH having occurred during play.
1.4.1.5
Childbirth
Childbirth is sometimes suggested as being responsible for SDH or RH. Hence, the lesions that can be observed after childbirth and their change over time in an asymptomatic child are specified below.
1.4.1.5.1
Subdural haematoma
Biomechanical elements.– The subdural lesions occurring during childbirth correspond to “static” compression phenomena, rather than impacts.
Clinical aspects.– The type of delivery influences the frequency of occurrence of intracranial haemorrhage, which occurs above all in cases of abnormal labour. Towner et al. studied 583,340 consecutive live, first births of children weighing 2500 to 4000 g (excluding multiple pregnancies) registered in a Californian database between 1992 and 1994, and examined the relationship between morbidity and the type of delivery. The rate of intracranial haemorrhages is higher after vacuum-assisted delivery, force forceps delivery and caesarean section performed after induction of labour than for non-instrumented delivery or caesarean section performed before induction of labour. This suggests that the risk is above all related to an abnormal course of labour.
We reviewed prospective studies on asymptomatic children . None of these children had undergone fundoscopy.
Asymptomatic SDH can be seen soon after childbirth (within 72 h), with a variable frequency of 9 to 46% depending on the investigational technique (ultrasound vs. MRI), the MRI field strength and the use of coronal slice to differentiate between supratentorial and subtentorial locations, the date of the examination and the type of delivery.
SDH is found more frequently when investigated soon after birth, with a more powerful MRI system, after vaginal delivery (14 to 33%), for vacuum-assisted delivery (40 to 77%) or forceps delivery (30 to 33%), for higher birth weights , lesions in the genital area , premature deliveries (24% in the study by Sezen ) and for first children (20% in the study by Sezen ).
These SDHs are situated on the subtentorial level, the supratentorial level or both. Whitby et al. and Looney et al. described a preponderance of subtentorial sites – in contrast to Rooks et al. .
Supratentorial SDH can be occipital but also parietal or temporal. In the series reported by Rooks et al. , all 46 cases of supratentorial SDH were situated in the posterior half of the skull: 30 out of 46 (65%) were interhemispheric and posterior, 29 out of 46 (63%) were occipital and 22 out of 46 (22%) were close to the tentorium cerebelli. Twenty children (43%) had also SDH of the posterior fossa. None of the cases of asymptomatic, supratentorial SDH in the series was frontal, as also reported by Whitby et al. . In the series reported by Rooks et al., 74% of the cases (34 out of 46) had SDH in two or three areas. The SDH was always homogeneous in all the MRI sequences . In the study by Looney et al. (using a 3 Tesla MRI machine), the 12 cases of multiple SDH were homogeneous and the lesions had the same age. The haemorrhage was often mild and appeared in the form of a thin film. None of the 46 cases described by Rooks et al. had an extradural subarachnoid or intraparenchymatous haemorrhage.
In summary, in the context of childbirth, SDH can be evidenced by brain imaging in asymptomatic neonates. The SDH is generally situated generally in a supratentorial site in the posterior half of the skull (not the anterior half) or in the posterior fossa – sites which are found in SBS. These SDHs are often multifocal. They are homogeneous and have the same age (when this information is given).
In the referenced studies, the follow-up data (when complete) showed that these asymptomatic SDHs did not progress to chronic SDH and resolved spontaneously within 1 month , except for one case in Rooks et al. which initially had (i) bilateral occipital SDH and (ii) SDH of the posterior fossa and then developed (at 26 days of age) a new left-side, frontal SDH. An examination at 5 months confirmed the disappearance of the SDH but enlargement of the pericerebral spaces.
1.4.1.5.2
Retinal haemorrhage
On the basis of several prospective studies, it seems that about one in three term neonates have RHs. They are found after all types of childbirth but occur more frequently after forceps or (even more so) vacuum-assisted deliveries. These haemorrhages are almost always superficial and deep intraretinal and uni- or bilateral (52%, i.e. 26 out of 50 of the cases reported by Emerson). They are often numerous (> 10) and extend out to the periphery in a third of cases. In 15 to 25% of cases, the RH has a white centre. They disappear very rapidly – often in less than 3 days . The RHs are very rarely still found at 1 month of age (two out of 202 cases, both of which involved vacuum-assisted delivery) and are never found after 2 months .
In summary, in a context of childbirth (particularly after forceps and vacuum-assisted deliveries) in asymptomatic neonates, RH of various types exist in a third of cases. These are mainly Defoort-Dhellemmes type 1 or 2 and disappear in less than a month (and mostly within a few days).
RH and even haemorrhages of the vitreous matter can also occur as a complication of prematurity-associated retinopathy in 1 to 2% of premature infants and can last for longer.
1.4.1.6
Hypoxia and anoxia
1.4.1.6.1
Subdural haematoma
Radiological aspects.– Three retrospective studies on the radiological signs of serious hypoxia have shown the absence of SDH in children (including some with prolonged cardiac arrest ).
Autopsy data.– Byard et al. did not evidence any macroscopic SDH in a series of 82 autopsies with histological proof of hypoxic-ischaemic encephalopathy in children under the age of three, other than in a context of SBS. They did not differentiate between foetuses and neonates.
Matschke et al. (who did not differentiate between foetuses and neonates either) found only 50 macroscopically observable cases of SDH in 715 consecutive autopsies performed in children under 1 year of age, most of whom had suffered from hypoxia before death [malformation (40.4%), the outcome of a perinatal complication (24.3%), infection (12.2%), metabolic disease (4.5%), sudden infant death (3.4%), inflicted trauma (2.4%) and other non-natural causes (2.1%)]. A cause was found for all the cases of SDH when a full dataset was available, i.e. in 48 cases out of 50: 14 cases of SBS, one case of accidental injury, 13 haemostasis disorders, 13 perinatal deaths, four deaths due to metabolic causes, three due to infectious disease and cases of two very localised SDH after sudden death. The most frequent cause was inflicted trauma (14 cases) and the latter mechanism was also mentioned for the two cases with incomplete data.
Thus, SDH in a hypoxic context is extremely rare. This is also what clinical studies show .
Upon histological examination, Geddes et al. found 36 intradural haemorrhages (IDH) in 50 foetuses and children but only one (unilateral) SDH was found macroscopically (in a child born after 25 weeks of pregnancy, who died of an infection after 1 week of life). In the 30 children born alive, only 13 had a histologically manifest IDH. Twelve of the 13 deaths occurred very early in perinatal period (during the first week for 11 of them) or the neonatal period (the first month of life for the 12th case) and only one of the children with clear IDH corresponded to the average age for SBS. Childbirth had been excluded as a possible cause of bleeding in 72% of the cases (36 out of 50: in 11 of the 17 in utero deaths but also in 13 of the 18 children who had lived more than 5 days [median: 23 days]), whereas haemorrhages due to childbirth can last up to 1 month. The difference in the frequency of occurrence of IDH (pooling “+” cases and “++” cases) according to whether there was hypoxia and anoxia or not was not significant ( P = 0.15) but it was stated that this lack of significance was due to the small number of cases. Despite this lack of significance, a “unified hypothesis” was presented. It supposed that subdural bleeding seen in some cases of HI in the child can result from passage of blood from the intracranial veins to the subdural space, due to a combination of severe hypoxia, brain oedema and an elevation in the central venous pressure. According to Geddes et al., subdural bleeding may thus not be due to rupture of the corticodural veins but may testify to immaturity – with no need for an impact or considerable force.
Cohen and Scheimberg evidenced clear IDH and signs of hypoxia of various degrees of severity in 25 foetuses and 30 children who died within the 19 first days of life, including 25 in the first week. SDH was found in two thirds of cases (16 foetuses and 20 neonates). The IDH was predominantly in the posterior part of the falx cerebri and the tentorium cerebelli.
In summary, hypoxia:
- •
is likely, in a particular population constituting of foetuses and children who died in the first month of life (mostly in the first week), to cause, contribute to or be associated with histologically detectable IDH and, at most, very mild posterior supratentorial and subtentorial subdural effusion (a thin film). Intradural suffusions may be missed on imaging or even on autopsy when the sample is inadequate;
- •
does not produce any macroscopic SDH in children over the age of 1 month.
1.4.1.6.2
Retinal haemorrhages
Acute hypoxia (such as that produced during suffocation, which frequently produces petechiae at the surface of the lungs, the heart or other internal organs) does not cause any RH.
1.4.1.7
Resuscitation manoeuvres
At the time of diagnosis of SDH, cardiorespiratory resuscitation manoeuvres are sometimes alleged to have caused bleeding.
1.4.1.7.1
Subdural haematoma
There are no known literature reports of an association between SDH and cardiorespiratory resuscitation.
The lesions observed following resuscitation are above all related to whatever circumstances had justified the use of resuscitation manoeuvres. The most frequently encountered lesions after resuscitation are anoxic-ischaemic lesions with brain oedema, diffuse brain ischemia that predominates in the less well vascularised regions, depending on the age of the child, and ischaemic lesions of the central grey nuclei. In the series, no SDH was reported .
In the retrospective study by Bush et al. of 211 children (mean age: 19 months) having required cardiorespiratory resuscitation (a study inclusion criterion) lasting 45 minutes on average (range: 3 to 180 minutes) for sudden infant death (56%), drowning (8%), congenital cardiopathy (7%) and pneumonia (4%), brain lesions were not reported.
The discovery of SDH after a cardiorespiratory resuscitation does not at all prove that resuscitation manoeuvres were responsible for this haematoma.
1.4.1.7.2
Retinal haemorrhage
There are few available studies concerning pre-hospital or hospital-based resuscitation by healthcare professionals. RH are extremely rare in young babies with neither HI nor haemorrhagic disease and who have received cardiorespiratory resuscitation (even when prolonged). In such cases, the RH are few in number, punctiform or flame-shaped, localized (sometimes with a white centre) and situated in the posterior pole in one or both eyes .
1.4.1.8
Other circumstances
Various circumstances can be addressed as part of this topic .
1.4.1.8.1
Retinal haemorrhage after convulsions
None of 32 children admitted after convulsions had any RH .
Only one child (aged 8 months) out of 153 (aged from 2 months to 2 years) examined after an epileptic attack had RH. The RH was unilateral and flame-like around the optic disc .
None of 32 children (mean age: 30 months) hospitalized after an epileptic attack had any RH, despite the need for resuscitation in a few cases .
1.4.1.8.2
Retinal haemorrhage after coughing
No RH was observed in a series of 100 consecutive children with a persistent cough .
1.4.1.8.3
Retinal haemorrhage after vomiting
No RH was observed in a series of 100 children with vomiting due to pyloric stenosis .
1.4.2
To what extent can the date of shaking be determined?
This dating has significant legal and forensic consequences: was there just a single episode of shaking? Was the abuse recurrent? Dating the injury is also essential for establishing the course of events, which can clear certain people with access to the child.
Dating is based on interview data, a set of clinical and radiological data (from repeated examinations, if need be) and, in some cases, pathological evidence.
1.4.2.1
Dating based on a set of clinical symptoms
Several publications having analysed comprehensive accounts of shaking state that the symptoms occur immediately after the trauma.
In a prospective study of 76 dead children, Gilliland found that there was no lucid interval whenever the information was given by a person who was not the perpetrator of the trauma.
Starling et al. studied 81 cases of admitted AHI. In 57 cases, the exact time of the trauma was known. None of the children for whom the data on the early sequelae were complete (52 cases, 91%) had been described as having normal behaviour after the act. When the data were incomplete (a child that was not looked after following the shaking), a lucid interval of up to 24 hours was described.
In a retrospective study, Biron and Shelton also found the immediate appearance of symptoms in the cases that included a description of the clinical courses of events.
Rubin et al. have reported that if pulmonary oedema occurred after AHI, it appeared within an hour.
1.4.2.2
Dating based on additional tests
1.4.2.2.1
Retinal lesions
It is difficult to date RH .
RH located at the posterior pole disappears within a few days, whereas massive haemorrhages (of all types, i.e. intra-, pre- or subretinal) that are profuse, coating the whole retina or flecked out to the periphery and associated with a unilateral or bilateral premacular haemorrhagic plaque, sometimes immediately suggesting haemorrhagic retinoschisis) take several weeks or months to disappear.
RH with a white centre (usually considered to be old) can be seen on the first day post-trauma.
Since intraretinal RH disappears within a few days, only the association with scarring, the sequelae of preretinal or subretinal haemorrhages (circular white scar on the retinal folds, macular retraction syndrome, zones of pigmentation and retinal atrophy – particularly in macular areas or right out at the edge of the retina – and fibroglial scarring) can be considered as reflecting the coexistence of older and recent lesions.
1.4.2.2.2
Subdural haematoma and subarachnoid haemorrhage
Time windows for dating.– On imaging, the change over time of intraparenchymatous haemorrhages is known:
- •
on a CT scan and for up to 2 days, the haemorrhage is hyperdense (compared with the adjacent parenchyma) and then (from 2 days to 1 month) becomes isodense and then (beyond 1 month) hypodense;
- •
on MRI, the characteristics of the intraparenchymatous haemorrhage are determined by the paramagnetic effects of the haemoglobin degradation products, the strength of the magnetic field and the type of sequence. However, this change over time is not applicable to SDH and subarachnoid haemorrhages in the infant, where it depends on the haemoglobin degradation products and physiological process such as blood clot formation and retraction, the change over time in the red blood cell concentration, the suffusion of serous liquid through the damaged dura mater and the extravasation of CSF and/or blood from the subarachnoid spaces through a torn arachnoid membrane .
The time window for dating acute SDH is wide for both CT and MRI: for CT, the hyperdensity can persist up to 11 days after the trauma; using MRI, the T1 hyperintensity can extend beyond day 13 .
According to a CT and MRI study of HIs of known date in adults, the time window for hyperintensity on T1, FLAIR and even diffusion sequences was wide: the FLAIR hypersignal is visible for up to 3 weeks and the T1 hypersignal becomes visible after 24 hours and persists for up to 4 months.
In conclusion, it is difficult to achieve precise dating by imaging .
Furthermore, the images are not always easy to interpret:
- •
in the acute stage of cases of compressive, diffuse brain oedema, SDH in a case of SBS can be absent or missed in the first imaging dataset . It may also not be detected if it is of low abundance and only located at the vertex;
- •
hyperdensity of the longitudinal fissure can reflect congestion or acute, intradural bleeding but also subarachnoid haemorrhage, a normal falx or relative hypodensity of the oedematous brain parenchyma .
Lastly, it should be noted that:
- •
heterogeneous SDH (suggesting repeated trauma and a diagnosis of SBS according to some authors) has also been reported in accidental HI ;
- •
the heterogeneous character of SDH can reflect rebleeding from the capillaries in a neoformed membrane ;
- •
some children can be subjected to several episodes of shaking, with the possible superposition of lesions of different ages (i.e. acute and older lesions). The presence of several SDHs with different density then becomes highly informative.
In summary, it is difficult to date lesions precisely with imaging.
It would be advisable to launch multicentre studies with contrasted-enhanced CT and MRI in all cases of accidental or non-accidental HI, in order to determine the potential for evidencing venous rupture and determining narrower time windows for dating.
1.4.2.3
Dating based on pathology laboratory data
Pathology-based dating is relatively accurate but cannot be performed thoroughly until the autopsy.
1.4.2.3.1
Examination of SDH
Macroscopic examination.– Dating is based on the appearance of an adherence between the SDH and the dura mater. For the first 3 days, the blood is liquid. Adherence starts on the fourth day. A neomembrane forms around the bleeding and becomes visible at between 7 to 10 days and is well developed from week 2 to week 4. From week 6 onwards, the contents of the blood clot take on a classic “engine oil” aspect. Encapsulation is complete at around week 8.
Histology.– The dura mater and the blood clot must be studied as a whole. One must study the junction zone between the healthy dura mater and the zone of the dura mater to which the clot begins to adhere. The dating involves the appearance of the clot, the dura mater and the brain’s meningeal surface. Schematically, the change over time is as follows :
- •
in the first 2 days, polynuclear neutrophils invade the clot and then progressively increase in number;
- •
on days 2–3, macrophages arrive and the nuclei swell;
- •
at around days 4–5, red blood cell lysis begins;
- •
from day 2 onwards, the neomembrane starts to form via the attachment of a layer of fibroblasts to the dural surface. Roughly, one layer of fibroblasts forms each day. Hence, one can distinguish between the following times: from 2 to 5 days, with the presence of two to five layers of fibroblasts at the dural surface;
- •
by week 1, the angiofibroblastic invasion of the clot begins; the dural membrane has 12 to 14 layers of fibroblasts at this point;
- •
by week 2, giant neovessels appear. The neomembrane is then about a third or half as thick as the dura mater;
- •
in parallel, Perls staining is always used for all samples, in order to identify iron in blood and siderotic macrophages which appear on days 2–3 in the subdural compartment following blood contact. This corresponds to metabolism of the heme group from haemoglobin after its release into the tissues by bleeding.
1.4.2.3.2
Examination of brain contusions
The presence of possible brain contusions and their change over time (albeit not very precise) can aid the dating process.
Histology.– In the child, three time phases can be distinguished:
- •
in the acute phase (during which there is little bleeding), one observe pycnosis of the nuclei of astrocytes and nearby neurons and the appearance of a few polynuclear cells;
- •
at 36 hours and up to week 3, the second phase starts with a cell reaction that intensifies progressively: it includes vacuolization of the capillaries and the oligodendrocytes, an inflammatory cell reaction, the activation and swelling of glial cells and activation of the microglia;
- •
after week 3, the third phase (gliosis) occurs.
Immunohistochemistry.– Oehmichen et al. have described the immunohistochemical change over time in the macrophages appearing in contusion areas as a function of the time since the trauma. This may enable dating on the basis of this marker.
1.4.2.3.3
Examination of the thymus
Another essential element in early-stage dating is the presence or absence of an acute thymic involution. This thymic reaction (mediated by corticoids synthesized and released by the adrenals) is the body’s reaction to stress. Four stages of acute thymic involution have been described, depending on the histological appearance. These stages are significantly correlated with the time since the onset of stress :
- •
in the first 12 hours, the appearance of the thymus does not change;
- •
Grade I acute involution corresponds to stress lasting for 12 to 24 hours: the thymic cortex takes on a faint “starry sky” appearance, due to the arrival of macrophages that come to phagocytose apoptotic lymphocytes in the cortex;
- •
Grade II corresponds to stress lasting for 24 to 48 hours and is characterized by a very marked “starry sky” aspect, associated with necrosis of Hassall’s corpuscles;
- •
Grade III corresponds to stress lasting for 48 to 72 hours: the differentiation between the cortical and spinal cord regions is no longer visible due to lymphocyte depopulation (their re-release into the circulation and intracortical apoptosis);
- •
Grade IV, for stress lasting for 3 days or more: there is complete lymphoid depopulation of the cortical zones; hence, the medulla appears to occupy the whole thymic surface and Hassall’s corpuscles are large and very close together.
This gradation of the thymus’s appearance is very reliable and very useful.
1.4.2.3.4
Analysis of bruising
This analysis can be performed in different ways : inspection with the naked eye or on photographs, histological analysis, biochemical assays (rarely used in routine practice) and objective evaluation of the colour by colorimetry and spectrometry.
Dating is random, due to high inter- and intra-individual variability. One can consider than a violet colour means that the bruising is less than 24 hours old and that the yellow colour does not appear before 18 hours at least .
By pooling and cross-checking all the clinical, imaging and pathology lab data, one can narrow the estimated window during which the trauma occurred to a day or even half a day.
1.4.3
Are some infants predisposed to the occurrence of subdural haematoma?
1.4.3.1
Expansion of the subarachnoid space
The observation of a widening of the pericerebral spaces together with SDH has given rise to two hypotheses.
1.4.3.1.1
First hypothesis: expansion of the subarachnoid spaces is a factor favouring the occurrence of SDH
The first hypothesis is that this widening is part of an expansion of the subarachnoid spaces (ESAS), a clinical entity which may predispose to the occurrence of SDH.
Characteristics of ESAS.– ESAS – a transient disorder of CSF resorption – has sometimes been called “benign external hydrocephalus of the infant”. ESAS is a clinical entity that is accepted by the paediatric and neurosurgical communities and is characterised by widening of the arachnoid spaces in an infant (in boys more than girls) in the absence of developmental abnormalities or clinical neurological signs.
The main clinical sign is macrocrania, with an increase in head circumference and a large, bulging fontanel. Some studies have reported a high frequency of children with ESAS but no macrocrania, corresponding almost completely to a physiological particularity . However, these studies were retrospective, the brain CT scan was performed in hospitalized children who were all symptomatic (retarded development, epilepsy or tone disorders ) and, lastly, clinical, radiological and ophthalmological signs of abuse were not always screened for.
In this entity, head circumference is often (but not always) high at birth and steadily increases to more than 2 standard deviations (SD) between 3 and 6 months. It generally stabilizes between the age of 1 and 2 years and then moves smoothly back to around +2 SD afterwards . The subarachnoid spaces normalize after 2 years .
There may be a family history of the condition.
The diagnosis of ESAS is based on the detection (in brain imaging) of liquid-filled expansion of the pericerebral spaces and the cerebral fissures (testifying to subarachnoid involvement) that predominates in frontal regions (mostly on both sides of the body) and the longitudinal fissure (more than 3 mm at the convexity, more than 4 mm in the corticocranial area near the foramina and more than 6 mm for the interhemisphere gap). The effusion is isodense with the CSF, the arachnoid cannot be distinguished and the parenchyma is normal. The expansion then decreases but moderate skull-brain detachment may persist .
Analysis of the literature concerning the hypothesis whereby ESAS favours the occurrence of SDH.– Clinical aspects:
- •
this hypothesis is rarely and poorly documented in the literature ;
- •
the main obstacles to progressing our knowledge of this precise aspect of the pathogenesis of SDH in the infant are as follows: sources of methodological bias, old studies that ignore the potential role of abuse and (above all) the difficulty in proving the prior existence of ESAS and the absence of trauma;
- •
the case reports with coexisting SDH and ESAS have only very rarely been explored thoroughly in terms of a potential AHI: fundoscopy and radiological bone examinations were rarely performed, an investigation was not always performed and the head circumference curve had not always been plotted. Whether the eyewitness was a family member/carer or not was not always stated;
- •
eight studies (either series or case reports) have reported follow-up data for children presenting ESAS , including just one prospective study . In all, 215 patients were followed up for an average of 40.3 months (cumulative follow-up: 524 patient years). Only two studies reported a total of four patients, including one in which the performance of fundoscopy and an investigation was not stated and three patients who definitely did not undergone fundoscopy or an investigation.
Biomechanical aspects:
- •
a biomechanical model suggests that ripping of the corticodural veins is promoted by ESAS . In contrast, a recent finite element analysis of the head of a 6-month-old infant by Raul et al. showed that ESAS has a shock-absorbing effect by reducing the relative displacement of the brain relative to the skull .
In summary, there is nothing in the literature to support the hypothesis whereby ESAS favours SDH in the infant.
1.4.3.1.2
Second hypothesis: expansion of the pericerebral space is the consequence of a previously undiagnosed head injury
The second hypothesis is that the widening of the pericerebral space is, in fact, a consequence of a previously undiagnosed HI.
Ewing-Cobbs et al. prospectively compared the initial imaging results for two groups of HI victims aged between 1 month to 6 years (30 children with AHI and 29 with accidental HI). The two groups were similar in terms of data on the perinatal period (apart from the birth weight) and the neonatal period. In the 30 children with AHI, there were nine cases of brain atrophy (bilateral, cortical and supratentorial), four cases of subdural hygroma (unilateral and affecting the convexity and the longitudinal fissure) and seven cases of ventricular dilatation. None of these anomalies were found in the 29 children with AHI. The nine children with atrophy all had some other associated brain anomalies: four had ventricular dilatation, four others had ventricular dilatation and hygroma and the ninth had subdural hygroma but normal-sized ventricles. Several haemorrhages were present in 68% of the AHI group vs. 32% in the accidental HI group. The mean number of extra-axial haemorrhages was 2.1 in the AHI group and 1.3 in the accidental HI group.
In a prospective study of children under the age of three with SDH, Feldman et al. found chronic SDH or acute SDH on chronic mixed SDH in 17 (44%) of 29 children with AHI, in eight (67%) children with trauma of unknown origin and in none of the 15 (0%) children with an accidental HI.
These studies suggest that the widening of the pericerebral spaces observed during the initial phase corresponds to the sequelae of an undiagnosed HI, rather than ESAS.
Follow-up studies on a cohort of infants with ESAS and shaken infants (evaluating the change over time in the brain imaging data) would be very useful.
1.4.3.2
Can SDH occur during a CSF circulation disorder?
Arachnoid cysts can causes complication with SDH after surgery in the infant. SDH can also occur after excessive drainage of CSF (after lumbar or peritoneal external derivation) or severe dehydration. All these cases reflect a very particular context.
1.4.3.3
Osteogenesis imperfecta
Osteogenesis imperfecta constitutes a differential diagnosis for diaphyseal and non-metaphyseal fractures. In fact, constitutive bone fragility is not responsible for metaphyseal lesions .
A relationship between osteogenesis imperfecta and SDH has not been established, even though two articles report the occurrence of SDH in children with the condition. SDH is not part of the usual set of symptoms in osteogenesis imperfecta.
1.4.3.4
New bleeding after SDH
The capillaries of a neoformed membrane can bleed anew, regardless of whether the infant has been shaken or not .
1.4.3.5
Conclusion
According to a literature review, there are no arguments to suggest that ESAS and osteogenesis imperfecta are factors that promote SDH. The diagnostic approach in these children (e.g. those with diseases that predispose to the occurrence of SDH or handicap) should be the same as in any other child.
In contrast, when shaking has already produced an SDH, new bleeding is possible in the absence of repeat shaking.
1.5
How does the most likely diagnosis affect the actions to be taken?
Shaking may have very serious consequences for the health of a young child (usually an infant). There is a risk of immediate death or handicap (the extent and impact of which are hard to predict in the early phase of diagnosis). There may be behavioural, intellectual, physical and sensory sequelae.
This type of trauma must prompt healthcare professionals to consider that the child is a victim of abuse and a victim of crime, in as much as shaking always constitutes an offence.
This document addresses the questions posed during the public hearing, by starting from the medical diagnosis established in a hospital setting:
- •
the diagnosis of SBS is highly probable (even certain) or probable;
- •
the diagnosis of SBS is possible;
- •
the diagnosis of SBS is ruled out. This latter point is not discussed here.
In this third section of the report, we provide a set of practical guidelines that continue on from those formulated in the two previous sections.
1.5.1
First hypothesis: a diagnosis of SBS is highly probable (even certain) or probable
In such a case, the medical care team and all other professionals involved (regardless of their field of expertise) must act to protect the child if they consider that it is in danger and so that its rights as a victim of abuse are safeguarded. In contrast, these professionals do not have to determine the identity of the perpetrator of the shaking (even if they can have an opinion on the matter) or the opportunity to start legal proceedings – these matters are the sole responsibility of the district prosecutor.
If the child dies, the death certificate must mention that there is a forensic and legal problem.
1.5.1.1
Should shaking be reported? If so, for what reasons?
The term “report” refers to any communication with the district prosecutor concerning the situation of a child in danger or likely to be so.
A report to the district prosecutor (with a copy sent to the Chairperson of the County Council) is essential. This will trigger a civil procedure (placing the child in care without delay) and a criminal inquiry (because shaking is an offence). These two procedures are distinct and have different objectives but can (and should) be performed in parallel – except in the situations of shaking by a third party in which there is no need to provide the child with legal protection since the latter is provided by the parents when they have authority over the child.
1.5.1.2
Discuss the case before reporting it
Although (i) the care team is faced with legal and ethical obligations to protect the child against possible future violence and (ii) shaking is a criminal offence, reporting the act often raises many questions.
In a first step, it is essential for the care team (or at least two professionals) to meet and review the symptoms and the reported facts, pool and compare the information gathered, make a diagnosis, examine other acts of abuse as appropriate, clarify each person’s opinion and discuss whether a report should be made. This meeting must take place as soon as possible. A written meeting report must be drafted.
Furthermore, a multidisciplinary medical, psychological and social evaluation of the situation is essential in order to analyse the child’s situation, identify risk factors and consider the child’s future and potential protection measures. Consulting with colleagues is never a waste of time. The healthcare professional should not confuse speed and haste.
When a social service assistant is part of the hospital team, he/she must necessarily participate in the decision-making process. In the event of a divergence of opinion with the care team, he/she is obliged to make a report (in view of the applicable legislation mentioned below) if it appears that the child is likely to be in danger.
1.5.1.3
What happens once a report has been submitted?
The hospital team’s report enables to protect the child at a time it is important to shield the latter from possible recurrence of abuse, regardless of who the perpetrator is.
1.5.1.3.1
Civil proceedings
Following the report, the district prosecutor can deliver an ordonnance de placement provisoire (OPP, temporary care order) if he/she feels that it is necessary to protect the child without delay (even during a hospital stay, in view of the risk of early recovery of the child by its parents, while enabling continuation of medical care).
The report also enables the protection of other children (whether siblings or not) likely to be in danger by virtue of the risk of recurrence, whoever the perpetrator is.
A protective OPP does not influence any subsequent legal proceedings and is strongly recommended to give the child immediate protection. This decision has no right of appeal and is valid for 8 days. It may involve referring the case to a juvenile court judge.
The district prosecutor who pronounces an OPP has “ must petition the appropriate judge within one week, who will maintain, modify or revoke the order ” (article 375-5 of the French Civil Code). Hence, the juvenile court judge can decide to prolong or not protective measures for the child or to modify it if needed. He/she can pronounce a care order (which is likely to be appealed by the holders of parental responsibility) that can last several months and may be renewed. The judge can also implement educational assistance measures.
When the judge is petitioned by the district prosecutor having pronounced the emergency, temporary care order, “he/she summons the parties and pronounces within two weeks of being petitioned. Otherwise, the child is handed back on request to its father, mother or guardian or to person or service to which it had been confided” (Civil Proceedings Code, article 1184, paragraph 3).
“The decision on pursual or not of the case must be taken within six months of the decision to issue temporary measures. Otherwise, the child is handed back on request to its father, mother or guardian or to person or service to which it had been confided.
If the inquiry has not finished within the term set out in the previous paragraph, the judge may, after seeking advice from the district prosecutor, extend this term for a period not exceeding six months” (Civil Proceedings Code, article 1185).
1.5.1.3.2
Criminal proceedings
Referring the matter to the district prosecutor in parallel enables the evidence to be examined in terms of a criminal offence and triggers an immediate criminal inquiry, in order to identify and potentially prosecute the perpetrator(s), decide on whether or not the enquiry should be pursued to establish the facts or identify the perpetrator(s) and assess whether the explanations given by the family/carers are plausible or change over time. The criminal inquiry may also exonerate other people involved. During the criminal inquiry, one must not lose sight of the need to protect the child.
Submission of the case to a judge enables the child’s future rights to be preserved (notably its right to compensation for the injury, even if the latter was caused by one of its parents). It is essential to maintain the possibility of compensation that will help pay for future care (private-practice occupational therapy and psychomotor therapy not covered by the social security system, individual help at school, etc.), limit the sequelae and enable the provision of appropriate support during childhood and then during adulthood in the event of handicap (a third-party carer, in particular).
In the event of death and medical and forensic opposition to burial, the police office leading the criminal inquiry and/or the district prosecutor must be informed. The latter opens an inquiry or proceedings to establish the cause of death (article 74 of the Code of Criminal Procedure) and can order a forensic autopsy.
The case must be submitted to the district prosecutor as soon as possible, so that the inquiry can start rapidly.
1.5.1.4
Who can report a case of abuse?
Any person becoming aware of child abuse, any person working in a public- or private-sector establishment aware that child is in danger or likely to become so, any public authority or any public servant becoming aware of a crime or offence in the exercise of his/her official duties must inform the competent authority without delay.
It is important to bear in mind the following legislation:
- •
Article 226-13 of the Penal Code: “ The disclosure of secret information by a person entrusted with such a secret, either because of his position or profession, or because of a temporary function or mission, is punished by one year’s imprisonment and a fine of €15,000 .”
- •
Article 226-14 of the Penal Code: “ The Article 226-13 is not applicable to the cases where the law imposes or authorises the disclosure of the secret. In addition it is not applicable :
(1) to the person informing a judicial, medical or administrative authority of cruelty or deprivation of which he has knowledge and which has been inflicted on a minor under fifteen years of age, or a person unable to protect himself because of his age, psychic or physical state;
(2) to the to the physician who, with the agreement of the victim, brings to the knowledge of the public prosecutor acts of cruelty that he has observed in the exercise of his profession that cause him to believe that sexual violence of any nature has been committed. When the victim is a child or a person unable to protect him/herself because of his/her age or physical or mental handicap, the said victim’s agreement is not necessary.
When performed under the conditions set out in the present article, reporting to the competent authorities cannot be the object of any disciplinary sanctions. ”
This article relieves the physician of the duty of physician-patient confidentiality and authorizes him/her to report the suspected abuse to the district prosecutor.
- •
Article 223-6 of the Penal Code: “ Anyone who, being able without risk to himself or to third parties to prevent by immediate action a felony or a misdemeanour against the bodily integrity of a person, wilfully abstains from doing so, is punished by five years’ imprisonment and a fine of €75,000. The same penalties apply to anyone who wilfully fails to render to a person in danger any assistance which, without risk to himself or to third parties, he could render him either by his own action, or by initiating rescue operations .”
- •
Article 434-1 of the Penal Code: “ Any person who, having knowledge of a felony the consequences of which it is still possible to prevent or limit, or the perpetrators of which are liable to commit new felonies that could be prevented, omits to inform the administrative or judicial authorities is punished by three years’ imprisonment and a fine of €45,000. Except where felonies committed against minors under fifteen years of age are concerned, the following are exempted from the provisions above :
1) the relatives in a direct line and their spouses, and the brothers and sisters and their spouses, of the perpetrator or accomplice to the felony;
2) the spouse of the offender or accomplice to the felony, or the person who openly cohabits with him.
Also exempted from the provisions of the first paragraph are persons bound by an obligation of secrecy pursuant to the conditions laid down under article 226-13 .”
- •
Article 434-3 of the Penal Code: “ Any person who, having knowledge of maltreatment, deprivations, or sexual assaults inflicted upon a minor under fifteen years of age or upon a person incapable of self-protection by reason of age, sickness, disability, psychic or physical deficiency or state of pregnancy, omits to report this to the administrative or judicial authorities is punished by three years’ imprisonment and a fine of €45,000. Except where the law otherwise provides, persons bound by an obligation of secrecy pursuant to the conditions set out under article 226-13 are exempted from the above provisions .”
- •
Article L. 226-4 of the Family and Social Action Code: “ Any person working in any of the organisations mentioned in the fourth paragraph of article L. 226-3 5
5 Public services, as well as public and private establishments that may be aware of children in danger or likely to become so.
and who, in view of the seriousness of the situation, reports on a child in danger to the district prosecutor must send a copy of this report to the Chairman of the County Council .”
- •
Article 40 of the Code of Criminal Procedure: “ Every constituted authority, every public officer or civil servant who, in the performance of his duties, has gained knowledge of the existence of a felony or of a misdemeanour is obliged to notify forthwith the district prosecutor of the offence and to transmit to this prosecutor any relevant information, official reports or documents .”
- •
Article 44 of the Code of Medical Ethics: “ When a physician considers that one of his patients is a victim of abuse or privations, he/she must implement the most appropriate resources for protecting the patient while showing circumspection. For a child aged 15 or under, he/she must (except under particular circumstances considered in all conscience) alert the judicial, medical or administrative authorities .”
1.5.1.5
To whom should shaking be reported?
Shaking is a serious act which justifies referral of the matter to the district prosecutor in order to protect the child. A report is also justified by the fact that shaking is a criminal offence.
Only the district prosecutor has the resources needed to protect the child rapidly and start a criminal inquiry to establish the facts of the case and look for the perpetrator.
The term “report” is used for any communication with the district prosecutor concerning the situation of a child who in danger or is likely to become so.
Article L. 226-4 of the Family and Social Action Code, modified by the Child Protection Act 2007-293 dated March 5, 2007, states that “ Any person working in any of the organisations mentioned in the fourth paragraph of article L. 226-3 and who, in view of the seriousness of the situation, reports on a child in danger to the district prosecutor must send a copy of this report to the Chairman of the County Council. When the prosecutor has been advised of the situation by another person, he/she shall send Chairman of the County Council the information that is required to enable the latter to fulfil the duty of protection confided in him/her and will inform the reporting person on the action taken as a result of the said report, in accordance with the terms set out in articles 40-1 and 40-2 of the Code of Criminal Procedure.”
It is thus important to send a copy of the report to the Chairperson of the County Council, in order to protect the child.
Only the district prosecutor can decide on measures to be taken following the report, the immediate protection of the child by issuing an OPP, the initiation of a criminal inquiry, the nature of the supposed criminal offence and proceedings before a court; he/she can also name an ad hoc legal guardian .
The district prosecutor can also refer the matter to the Cellule de recueil, de traitement et d’évaluation des informations préoccupantes (CRIP, the County Child Abuse Prevention Office) in order to obtain additional information on the family situation and thus evaluate the need to initiate administrative protection or any form of assistance for the parent(s), in compliance with the protocol established by the Chairperson of the County Council and the district prosecutor.
1.5.1.6
What information should the report contain?
The report per se is not defined in law. There are no legal or regulatory texts specifying the content of the report and the procedures for transmission to the district prosecutor.
However, a certain number of rules must be followed, in order to provide an objective opinion:
- •
the person who reports the shaking must never accuse or refer by name to the perpetrator of what may be a criminal offence;
- •
it is important to make a clear distinction between the observed facts on one hand and reported accounts on the other. Always specify the source of the information (e.g. statements made by the patents’ or the social worker), in order to avoid any ambiguity for the recipient of the report. One should use the conditional tense, an indirect style or put reported statements between quotes.
The report’s content is outlined below 6
6 This proposal appears to be better suited to these situations than the model medical certificate published in 2004 by the French Ministries of Justice, Healthcare and the Family.
.Essential information:
- •
the recipient’s name and address;
- •
the report writer(s) name(s), job title(s) and professional address(es);
- •
the parents’ names, address(es) and telephone number(s);
- •
a chronological description of the facts concerning the child;
- •
initial medical observations, with the results of the main additional examinations and hypotheses on the cause of the lesions. If an initial medical certificate is attached, it should be kept separate from the main report;
- •
information on the severity of situation justifying direct filing with the district prosecutor’s office;
- •
details on the immediate follow-up envisaged by the physician or medical staff;
- •
date and signature(s).
Add the following to the initial report whenever possible:
- •
administrative information concerning the family: composition, ages, professions, etc.;
- •
childcare procedures: parents, child-minder, crèche , other people;
- •
explanations for the observed lesions provided by the carers and the degree of compatibility between these explanations and the medical observations;
- •
people already involved in the matter, citing the names, job titles and addresses of other professionals potentially contacted or involved (County Childcare Office, crèche , day nursery, etc.).
It is recommended that each hospital establishment defines the procedure to be followed by its staff in the event of a report of suspected abuse to the district prosecutor. The following advice can be given:
- •
establish a document signed by both the hospital physician attending to the child and the social worker (potentially completed by the psychologist or psychiatrist who had spoken with the family);
- •
when immediate child protection seems necessary, it is recommended to contact the district prosecutor’s office by telephone and then confirm the report in writing, as follows:
- ∘
send the report by fax and by registered post with signed-for delivery, keeping a copy in the hospital file,
- ∘
send a copy to the Chairperson of the County Council, in accordance with article L. 26-4 of the Family and Social Action Code.
- ∘
The protocol established between the County Council, the prosecutor, the hospitals and other professionals likely to become aware of cases of shaking (in compliance with the 2007 Child Protection Act) should include clear, valid instructions for the county as a whole.
The report should include a request by the authors to be kept informed of any subsequent action taken by the district prosecutor.
1.5.1.7
When should a report be filed?
It is advisable to report the main details as rapidly as possible, in order to protect the child and not jeopardize the criminal inquiry. The sooner after the event the report is filed, the sooner an effective criminal inquiry can start.
Delaying the submission of a report is risky for two reasons: it delays protecting the child and complicates any subsequent enquiry.
However, this does not remove the imperative need to consult with colleagues before completing the report, except in extremely urgent circumstances (e.g. the child will be in danger if discharged to home immediately).
When faced with an urgent need to protect the child, it is advisable to make an initial report and then send additional information after meeting with colleagues and performing a multidisciplinary evaluation.
1.5.1.8
What impact will failure to report shaking have on the child?
The child can only receive legal protection if the district prosecutor has taken up the case. If no report is made, there will not be a criminal inquiry to establish the facts more precisely and potentially identify the perpetrators. The child cannot hope to receive compensation.
If the immediate protection of the child appears necessary and if the parents do not agree, it is essential to contact the district prosecutor because he/she alone can impose protection (NB:administrative protection decided by the Chairperson of the County Council can only be implemented if the holders of parental responsibility agree).
The child’s rights as a victim may not be taken into consideration and defended because if there is a conflict of interest, an ad hoc legal guardian can only be named by the judicial authorities 7
7 The report enables the designation of an ad hoc guardian by the prosecutor (Act 2010-121 dated February 8, 2010 – article 5; article 706-50 of the Code of Criminal Procedure), by the investigating judge (article 706-50 of the Code of Criminal Procedure and article 388-2 of the Civil Code), the juvenile court judge or the jurisdiction in which the perpetrator of the shaking is being judged (Act 2007-308 dated March 5, 2007; article 388-2 of the Civil Code).
.In the absence of a report, the child will not be able to receive any compensation for the injury suffered. Only legal action provides access to compensation procedures. It must be borne in mind that shaking an infant may to provoke severe pathologies that may lead to life-long handicaps (notably mental retardation and blindness) that will require significant care provision.
1.5.1.9
What risks are incurred by professionals who do not report cases of shaking?
1.5.1.9.1
Risks incurred by the physician
Article 44 of the French Code of Medical Ethics obliges the physician (except under particular circumstances that he/she shall consider in all conscience) to alert the judicial, medical or administrative authorities in the event of abuse or privation in a child aged 15 or under. For cases of severe abuse, a report to the State Prosecutor is recommended by the French Medical Council. If the physician does not alert any of these authorities, he/she may be sanctioned under article 223-6 of the Penal Code.
The fact that this obligation is accompanied by a conscience clause does not make it any less imperative. Hence, if the physician does not alert the authorities, he/she must explain the exceptional circumstances that prompted this decision. Consideration of these exceptional circumstances in all conscience does not exempt the physician from explaining the absence of a report but does protect him/her against being sanctioned. However, in the latter case, repeated refusal to report a suspected case (which would appear to be the result of a predetermined policy) would prevent the physician from invoking the conscience clause because the supposedly exceptional circumstances would then have become general.
If a physician does invoke the conscience clause, he/she must nevertheless ensure that effective protective measures are implemented in order to avoid recurrence of the shaking or other abuse.
If further abuse occurs, the physician may be accused of inaction, on the basis of article 223-6 of the Penal Code 8
8 “Anyone who, being able without risk to himself or to third parties to prevent by immediate action a felony or a misdemeanour against the bodily integrity of a person, wilfully abstains from doing so, is punished by five years’ imprisonment and a fine of € 75,000. The same penalties apply to anyone who wilfully fails to render to a person in danger any assistance which, without risk to himself or to third parties, he could render him either by his own action, or by initiating rescue operations.”
concerning failure to assist a person in danger. Failure to assist makes no exceptions: healthcare professionals and non-professionals alike are concerned. This article does not refer to the absence of a report but does refer to inaction of the professional or anyone aware of the danger. The article therefore sanctions failure to act to protect the child effectively rather than failure to speak out.In the event of death following highly probable (or even certain) shaking, a physician who attests that the infant died of natural causes and that the death does not pose any legal or forensic problems commits the offence of falsification, which is punishable by 3 years imprisonment, a fine of €45,000 and being struck off (article 441-1 of the Penal Code).
The physician also exposes him/herself to disciplinary sanctions for violation of the following dispositions: article 3 of the French Code of Medical Ethics as codified by article R. 4127-3 of the Code of Public Health (“ The physician must, under all circumstances, comply with the principles of morality, probity and devotion that are essential for practicing medicine. ”) and article 28 of the French Code of Medical Ethics (codified by article R. 4127-28 of the Code of Public Health (“ The issuance of a biased report or a certificate out of kindness is prohibited. ”).
As soon as a diagnosis of shaking appears to be the cause or a possible cause of the infant’s death, the physician who delivered the death certificate must mention that there are forensic and legal problems.
1.5.1.9.2
Risks incurred by other professionals
Articles 434-1 and 434-3 of the Penal Code on the obligation to report crimes and abuse include an exception for the people subject to the professional duty of confidentiality and specify that the latter may not be convicted on this basis. Nevertheless, these people may choose not to report the abuse but always have a legal obligation to assist a person in danger (articles 223-5 to 223-7 of the Penal Code).
1.5.1.10
What risks are incurred by professionals who report shaking?
The report cannot lead to prejudicial legal consequences for persons subject to a professional duty of confidentiality, except when the report could be considered as a knowingly false accusation.
The last paragraph of the article 226-14 of the Penal Code states that “the report made to the competent authorities under the conditions set out in present article cannot lead to any disciplinary sanctions”.
On the penal level, a report that turns out to be groundless will only be considered as a knowingly false accusation 9
9 Penal Code, article 226-10: “A denunciation made by any means and directed against a determined person, of a fact that is liable to cause judicial, administrative or disciplinary sanctions and that the maker knows to be totally or partially false, where it is sent either to a judicial officer or to a judicial or administrative police officer, or to an authority with power to follow it up or to refer it to the competent authority, or to hierarchical superiors or to the employer of the person concerned, is punished by five years’ imprisonment and a fine of € 45,000. The falsity of the act denounced is conclusively established by a final decision of acquittal, or decision to drop the prosecution, which declares that the alleged facts are not established or that they are not attributable to the person denounced. In any other case, the court seized with the prosecution of the denouncer weighs the accuracy of the denouncer’s accusations.”
if it can be proved that the author of the said report acted in bad faith, i.e. with the intention to harm the accused person. Again, use of the conditional tense and an indirect style and putting reported statements between quotes are recommended.1.5.1.11
What information should be given to the parents? What are their rights?
The necessary dialogue with the parents and the obligation to provide them with information must not, however, hinder or interfere with the criminal inquiry.
If the decision to make a report is taken, the hospital staff must reconcile (i) the need for dialogue with the parents and the need to provide them with information and (ii) the effectiveness of the criminal inquiry. Information exchange with the parents must form part of efforts to make a medical diagnosis, treat and protect the child and evaluate the situation. Reports made in the absence of true dialogue with the parents are likely to undermine trust.
Dialogue with the parents is necessary and enables the physician to gather their explanations about the injuries presented by the child. The physician should first inform the parents that in light of the severity of their child’s condition, the district prosecutor’s office will be contacted. He/she should also specify that the district prosecutor will decide on any further actions to be taken. This approach, which means taking time and making an effort to listen, is best led by a senior physician in the presence of another staff member.
It is essential to try to make the parents understand that the goal is not to denounce them but to attract attention to a dangerous situation and protect their child.
The parents must be informed of the report (except when contrary to the child’s interests), the possibility that a temporary care order may be issued by the district prosecutor and the possibility of filing a complaint against person or persons unknown if they deny the shaking and attribute it to someone else.
The report and the information therein form part of the legal file and not the medical records. The objection whereby the parents may gain access to their child’s medical records and thus become aware of the report is therefore not valid, inasmuch as this document is not part of the medical records as defined in the Code of Public Health. In fact, the Commission on Access to Administrative Documents ( Commission d’accès aux documents administratifs , CADA) considered in an opinion issued on July 27 2006 that the report is a legal document rather than an administrative document and that the parents have to contact the judicial authorities if they wish to gain access to it.
In terms of the judicial procedure, the government decree dated March 15, 2002, acknowledged the parents’ right to directly access the records on judicial protection of their child but only in the time period between the summons and the hearing at which a decision is taken. The judge can, however, decide to exclude certain documents from this consultation 10
10 Article 1187 of the Civil Proceedings Code: “The minor’s, his father’s, mother’s, tutor’s attorney or that of the person or the institution in whose care the child is placed may consult the file at the Clerk’s office from the date on which the opening of the proceeding has been notified till the eve of the testimony of court hearing […] By a reasoned ruling, the judge may, when an attorney is not present, exclude the whole or part of the documents from the consultation by one or the other parent, the tutor, the person or the representative of the institution who has the child’s custody or the minor if this consultation would cause grave physical or moral damage to the minor, a party or a third party.”
.1.5.1.12
What information should be given to other hospital staff and professionals outside the hospital?
The information circulated within the care team must be limited to the strict minimum required by each professional to establish a diagnosis, provide care or make a multidisciplinary evaluation of the situation or to protect the child.
Information sharing was cited for the first time in the Patients’ Right Act dated March 4, 2002. It concerns healthcare professionals. Article L. 1110-4 of the Code of Public Health states that “ two or more healthcare professionals can […], in the absence of opposition by the duly advised person, exchange information concerning the same treated patient ”. This information exchange between healthcare professionals is, however, licit when required for care purposes, “ in order to ensure the continuity of care or determine the best type of care possible ”.
The sharing can take on a more collegial dimension and concern all the members in the care team: “When the person is treated by a care team in a healthcare establishment, his/her personal information is considered to have been confided by the patient to the whole team.” Here, information is shared not only between healthcare professionals but also between members of the care team, which may enable to social workers to be included, in particular. It may be useful to remind staff of this principle, notably during review meetings with medical students and trainee nurses. The duty of confidentiality applies not only to the hospital staff but also to any other people involved with the healthcare establishment (members of a patient association and volunteers, for example).
The report and the information contained therein form part of a legal file and not the medical records. However, this information must be given to healthcare professionals if it is necessary for ongoing care.
Regarding non-hospital-based medical and social staff, it is important to only send information that is strictly required as part of their care duties, for protection or when evaluating the situation or deciding on whether the child should be taken into care or monitored. The Child Protection Act 2007-293 dated March 5 extends the possibility of information sharing to people who implement child protection measures. The latter “ are authorized to share confidential information” under certain conditions. Only strictly necessary information can be sent to these professionals or shared between people subject to a duty of confidentiality 11
11 Article L. 226-2-2 of the Family and Social Action Code: “As an exception to article 226-13 of the Penal Code, people subject to a professional duty of confidentiality and who implement child protection measures or […] assist the latter are authorized to share confidential information with each other in order to evaluate an individual situation and determine and implement the protective and supportive measures from which the children and their families may benefit. Information sharing relative to an individual situation is strictly limited to that required for the fulfilment of their child protection duties. The father, mother or other persons holding parental authority, the legal guardian and the child (depending of his/her age and maturity) must be informed first in an appropriate way, unless this is not in the child’s interest.”
.Subject to this condition, information sharing is not limited to staff within the same hospital or belonging to the same profession but can take place between all professionals involved with the child 12
12 Article 226-2-2 of the Family and Social Action Code.
(between a hospital department and a nursery or a clinic or between a physician and a social worker, etc.).The conditions on sharing information between professionals thus fall into three groups:
- •
the shared information must be kept confidential (including physician-patient confidentiality) and must be strictly limited to whatever is necessary to achieve the duty of care (diagnosis, medical treatment, evaluation and/or protection);
- •
the parents (or even the child him/herself, depending on age and maturity) must be informed that information concerning their child is being exchanged, except when this is not in the child’s interest or risks compromising the criminal inquiry;
- •
the people participating in the information sharing must comply with a professional duty of confidentiality.
1.5.1.13
What information will the reporting person receive concerning the outcome of his/her report?
In return, the district prosecutor’s office must inform the professional who signed the report of any subsequent action taken (while complying with the need for confidentiality within the inquiry). Article L. 226-4 of the Family and Social Action Code (introduced by the 2007 Child Protection Act) states that “ the district prosecutor shall inform the person who made the report of the actions taken as a result, in accordance with the terms set out in articles 40-1 and 40-2 of the Code of Criminal Procedure” .
The district prosecutor’s office must tell the person who filed the report about any immediately taken actions: an ongoing criminal inquiry, referral of the case to a juvenile court judge, etc. This feedback set out in the legislation must be properly implemented.
Immediate, partial feedback is quite easy to provide by setting up simple procedures. It is recommended that a form is established and sent back and forth between the district prosecutor’s office and the person who filed the report. In order to set up this procedure, the form should be part of the standard report mentioned above.
1.5.1.14
What measures may be taken by the district prosecutor following a report of suspected abuse?
A report sent to the district prosecutor’s office can trigger a child protection procedure and/or a criminal inquiry. Two parallel, complementary procedures may thus be launched. In parallel, an ad hoc legal guardian can be appointed.
The ad hoc legal guardian is a representative of the child who has a limited mandate and who is appointed (for a given case) to defend the child’s interests. His/her appointment enables a child lacking a legal capacity to be a plaintiff and to receive assistance in court.
The ad hoc legal guardian can be drawn from a regional list (article 706-50 of the Code of Criminal Procedure and article 388-2 of the Civil Code) and appointed by:
- •
the district prosecutor;
- •
the magistrate investigating abuse of a child by the one or more holders of parental authority; the ad hoc legal guardian then exercises the plaintiff’s rights (if required) on behalf of the child;
- •
by the juvenile court judge;
- •
by the jurisdiction judging the criminal offence;
- •
by the judge supervising guardianship “when the legal representative’s interests conflict with those the child”.
The ad hoc legal guardian thus has a legal duty and a role as a contact person and a helper. He/she is independent with respect to the judge and the parents but must keep the judge informed about the main steps in the proceedings and the performance of his/her duties.
The ad hoc legal guardian can refer the matter to the Commission d’indemnisation des victimes d’infraction pénale (CIVI, a crime victim compensation commission) 13
13 The CIVI’s powers and duties are defined in articles 706-3 to 706-15 of the Code of Criminal Procedure.
, without waiting for the conclusion of the legal proceedings. This commission is present in each county court and can be petitioned by “ any person having suffered injury as a result of confirmed criminal acts whether voluntary or not in nature” with a view to obtaining compensation. The commission does not have to wait for the conclusion of the legal proceedings before awarding compensation.1.5.1.14.1
The criminal inquiry
The goal of the criminal inquiry is to determine the exact circumstances leading to injury of the child and the causes and motives for the shaking, to evaluate the risk of recurrence, to establish whether a crime has been committed 14
14 There are two kinds of penal charges: offences are assaults causing a temporary work incapacity for less than a week or more than a week or involuntary acts of violence causing a temporary work incapacity of more than three months or less than three months; crimes are murder with intent and manslaughter.
and, if so, to identify the perpetrators. In France, it is led by the police force or the gendarmerie (usually a specialist child protection unit under the supervision of the district prosecutor’s office).The possible perpetrators must be confronted with the contradiction between their version of the facts and the medical diagnosis. This confrontation is essential but complex. The date or probable date of the injury is an important piece of information for the criminal inquiry. It prompts the investigation of all persons likely to have been in the presence of the child during the suggested period (police custody, a hearing before the judge, seizure of documents, comments, etc.). The police custody is decided by police officer in the criminal investigation department.
The members of the hospital team and professionals in contact with the family may be interviewed – notably in the event of contradiction with the parents’ explanations or the absence of an explanation. They must state their knowledge of the situation and transmit any documents required for the purposes of the inquiry . Hospital staff and social workers cannot claim an overriding professional duty of confidentiality when information is requested by a crime squad officer duly mandated and supervised by a legal authority.
If the physician receives a summons as part of a preliminary inquiry, he/she may communicate the facts known to him/her but is not obliged to do so – he/she can plead a professional duty of confidentiality.
The criminal investigation department performs all the procedural acts, under the supervision of the district prosecutor’s office (to which regular reports will be made). In this respect, an autopsy or an expert medical opinion may be ordered and the members of the hospital service may be called for interview.
Importantly, experts who become involved after the start of the judicial inquiry should be competent in the field concerned: paediatrics, ophthalmology or even biomechanics. In the absence of appointed medical experts, information on the context, compatibility of accounts and the drafting of medical reports are necessary for the investigating officers.
During the inquiry or investigation, the medical records may be requisitioned. This requisition is the only way for criminal investigation department officers to obtain the medical information held by the physicians and healthcare establishment. This procedure must comply with procedures that maintain physician-patient confidentiality. The requisition must be performed in the presence of the establishment’s Director and the Head of Service concerned.
The medical records are generally handed over voluntarily by the hospital service to a criminal investigation department officer bearing letters rogatory (i.e. without the need for seizure) (appeal judgement 95-811.40 dated 20/09/1995 and Circular 97-13 dated 24/11/1997).
It is advisable to photocopy requested documents prior to their transmission, in order to (i) comply with the healthcare establishment’s obligation to store its medical data and (ii) counter the risk of not having the requisitioned items returned.
The presence of a Medical Council representative is recommended during the requisition of medical records (Circular 97-13 dated 24/11/1997 ).
An inventory of requisitioned items should always be made before the latter are placed under seal. However, if drawing up an inventory at the time is problematic, it is possible to have the items placed under seal temporarily (article 56 of the Code of Criminal Procedure).
It is advisable to request the return of requisitioned items. This request must be sent to the investigating judge if it is made during the legal proceedings (article 99, paragraph 1 of the Code of Criminal Procedure) or to the ruling jurisdiction if the case is closed (Article 373 and article 484, paragraph 2 of the Code of Criminal Procedure).
1.5.1.14.2
The outcomes of the criminal inquiry
The procedure may 15
15 Article 40-1 of the Code of Criminal Procedure: “Where he considers that facts brought to his attention in accordance with the provisions of article 40 constitute an offence committed by a person whose identity and domicile are known, and for which there is no legal provision blocking the implementation of a public prosecution, the district prosecutor with territorial jurisdiction decides if it is appropriate: (1) to initiate a prosecution; (2) implement alternative proceedings to a prosecution, in accordance with the provisions of articles 41-1 or 41-2; (3) or to close the case without taking any further action, where the particular circumstances linked to the commission of the offence justify this.”
:- •
be abandoned forthwith if the offense cannot be proven due to lack of evidence or lack of an identifiable perpetrator;
- •
prompt the opening of a judicial investigation (obligatory for offences classified as crimes) so that an examining judge can pursue the inquiry. The later may request assistance from medical experts. At the end of the investigation, the case may be:
- ∘
dismissed if the offence is not sufficiently characterized,
- ∘
judged before a Magistrates Court (if the act is considered to be an offence with relatively minor consequences),
- ∘
judged before Court of Assizes (for offences with serious consequences);
- ∘
- •
lead to judgement of the person or persons accused:
- ∘
by a Magistrates Court, as a result of a direct summons, convocation by a criminal investigation department, through a statement or by an immediate appearance in court in the few cases where the facts are simple, can be dealt with by the magistrate and can be ascribed with certainty to the accused,
- ∘
by Court of Assizes if the act is considered to be a crime; the accused person may appear in court prior to arrest or after a period of provisional custody.
- ∘
1.5.1.14.3
Initiation of a child protection procedure
Initiation of a child protection procedure is intended to provide the child with judicial protection. The district prosecutor can (regardless of whether an OPP is ordered or not) refer the case to a juvenile court judge. The latter generally orders investigation and a 6-month care review procedure ( investigation et orientation éducative 16
16 The social inquiry and the IOE are due to be renamed as a “mesure judiciare d’investigation educative” (MJIE).
) to better describe the personalities of the people involved and the family situation: a social inquiry and a psychological or psychiatric assessment. The judge may then decide (if he/she considers that the conditions of article 375 of the Civil Code 1717 Art. 375 of the Civil Code: “Where the health, security or morality of a not emancipated minor are imperilled, or where the conditions of his education are seriously endangered, measures of educational assistance may be judicially ordered.”
are met) to apply protective measures at the child’s home domicile ( action éducative en milieu ouvert, AEMO) or placement of the child with a foster family or in institutional care. He/she can decide to place the child with the child protection service as the social inquiry proceeds or to place the child as soon as he/she is petitioned.In theory, these measures are independent of the outcome of any legal proceedings seeking to establish whether the child’s family or carers are guilty or not. If the presumption of innocence leads to the dismissal of legal proceedings (in the event of doubt as to the intention to cause harm or the identity of the perpetrator of a violent act), this does not means that the child may no longer require protection.
1.5.1.14.4
What are the potential criminal charges and sentences for perpetrators of shaking?
There is no specific criminal charge of “shaking” per se but the act always constitutes a violation of the law. The usual criminal charges relate to involuntary or voluntary assault with aggravating circumstances. It is important to differentiate between the intent to shake and consideration of the consequences of this act.
The severity of sentences handed down by the courts illustrates very clearly the clear disapproval of all violent acts inflicted on a child under the age of 15 by an ascendant (the legal, natural, or adoptive parents or the grand-parents, if the child has been entrusted to them) or a person with responsibility for the child (a child-minder, the latters’ spouse or partner, a partner of one of the parents or any other person charged with looking after the child).
In fact, the sentences are even heavier for perpetrators who have a duty to look after the child’s health and safety. The maximum prison sentence for perpetrators of shaking as set out below, depending on whether the act is classified as an offense or a crime (fines are voluntarily not referred to):
- •
for a crime to be tried before a Court of Assizes:
- ∘
manslaughter of a child aged 15 or under: a 20-year prison sentence, or 30 years if the perpetrator is an ascendant or a person with authority over the child,
- ∘
assault leading to mutilation or permanent infirmity in a child aged 15 or under: a 15-year prison sentence, or 20 years if the perpetrator is an ascendant or a person with authority over the child;
- ∘
- •
for an offence to be tried before a Magistrates Court:
- ∘
assault leading to ITT for more than 1 week in a child aged 15 or under: a 5-prison sentence, or 10 years if the perpetrator is an ascendant or a person with authority over the child,
- ∘
assault leading to a ITT for a week or less in a child aged 15 or under: a 3-year prison sentence, or 5 years if the perpetrator is an ascendant or a person with authority over the child.
- ∘
There is also a charge relating to repeated violence to a child aged 15 or under; depending on the outcome, this charge may be qualified as a crime or an offence:
- •
the act is qualified as a crime if the repeated violence led to death of the child (with a 30-year prison sentence) or mutilation or permanent infirmity (with a 20-year prison sentence);
- •
the act is qualified as an offence if the repeated violence led to ITT of more than a week (with a 10-year prison sentence) or less than a week (with a 5-year prison sentence).
In addition to the main perpetrator, other people in the child’s environment may also be prosecuted for other charges, notably:
- •
not having prevented a crime or offence against the child, failure to assist a person in danger: a 5-year prison sentence;
- •
lack of care and/or endangerment of a child’s state of health by an ascendant or a person with authority over a child aged 15 or under (for example, this is the case for a passive mother who is aware of her child’s precarious status and fails to act, thus worsening the situation): a 7-year prison sentence.
It has been suggested that shaking an infant can be qualified as involuntary damage to a person’s well-being caused by clumsiness, imprudence, inattention, negligence or a failure to ensure safety or prudence imposed by the law (this type of qualification mainly applies to traffic offenses, labour law offences and injuries caused by animals). These charges are unlikely to be used in the context of SBS because the act itself is always qualified as voluntary violence (with intent; as stated by the Court of Cassation’s judgement dated January 7, 1998, which criticized the Court of Appeal for not having sufficiently established that the accused [an ascendant charged with manslaughter of a child aged 15 or under] was aware that his actions could damage the child’s physical integrity of its child but added the facts pertaining to the accusation were indeed considered as a crime under the law and that the proceedings were legitimate). There do not appear to be any cases of jurisprudence that qualify shaking an infant as an involuntary act.
If the act is qualified as an offense or crime by a judge, an ad hoc legal guardian 18
18 Article 706-50 of the Code of Criminal Procedure: “The district prosecutor or the investigating judge seized for intentional offences committed against a minor appoint an ad hoc administrator where the protection of the interests of the minor is not completely ensured by his legal representatives or by one of them. The ad hoc administrator ensures the protection of the interests of the minor and exercises if necessary in the latter’s name the rights open to a civil party. In the event of a civil party petition, the judge has an advocate appointed officially for the minor if none has been already chosen. The previous provisions are applicable before the trial court.”
can be appointed by the judicial authority to defend and protect the child’s interest if the latter conflicts with that of its legal representatives. The ad hoc legal guardian exercises parental authority over the child relating to the ongoing proceedings instead of the legal representatives. A lawyer appointed to defend the child can act as a plaintiff and thus gain access to the legal file (the inquiry and the proceedings). He/she can ensure that medical specialists in SBS are appointed.Additional sentences may be handed down. In cases where shaking is admitted, the most adequate additional sentence is a temporary or permanent professional ban on the person charged with looking after the child (5 years at most, in this instance).
It is important to note that qualifying the act of shaking is of huge importance. The whole process of protection is enabled or stopped according to whether the act is qualified or not. The same is therefore true for the compensation.
1.5.1.14.5
Under which conditions can the victim receive compensation?
Compensation is possible once the act of shaking is established. It is therefore important that it be established, even if the perpetrator is never identified. Reporting the shaking to the legal authorities is essential for enabling the possible award of long-term compensation to the victim of shaking.
Since shaking may cause severe, invalidating injuries, the question of compensation for the victim arises. The compensation process is rendered more complex by two factors: the victim’s young age (which prevents the child from acting in a legal capacity) and the fact that the perpetrator of the injury is often the child’s legal representative, charged with safeguarding his/her interests. Furthermore, the perpetrator’s economic situation may not correspond at all to the amount of compensation awarded as damages to the victim. Lastly, the inquiry does not always enable identification of the perpetrator with certainty.
The law has solved the first problem by instituting the ad hoc legal guardian, enabling to resolve the contradiction generated by the fact that the parent is the legal representative of the abused child. Hence, it is important for the latter to be appointed.
The second series of difficulties (resulting from the perpetrator’s meagre financial resources or, more generally, when then perpetrator cannot be identified) has been taken into account by legislative introduction of the CIVI. As in the field of road accidents or terrorist attacks, the law replaces the traditional mechanism of individual responsibility (where the perpetrator of the injury is the only person liable to pay damages) by shared responsibility, where the state takes charge of compensating the victims of certain types of damage or injury (although the state can pursue the perpetrator, if ever the latter becomes known).
The powers and attributions of the CIVI are defined in articles 706-3 to 706-15 of the Code of Criminal Procedure. This commission exists within all county courts and is composed of two professional magistrates and one lay assessor. It can be petitioned by “ any person having suffered injury as a result of confirmed criminal acts, whether voluntary or not in nature ” and which have led to death, permanent incapacity or temporary incapacity of more than a month or which constitute a crime of rape, sexual assault, sexual injury without violence or slave trading. This definition covers all the charges likely to be brought in cases of SBS. The compensation system also concerns situations where the perpetrator has not been identified with certainty, although the shaking has been confirmed. The only case in which a child will not be compensated by the CIVI is when the inquiry has quashed the diagnosis of shaking and excluded any criminal behaviour leading to injury.
The matter can be referred to the CIVI immediately, without waiting for the outcome of the judicial proceedings. A request for compensation must be presented within 3 years of the date of the offence or in the year following the final verdict issued in a public or civil prosecution before the criminal courts, in compliance with article 706-5 of the Code of Criminal Procedure. The plaintiff may, however, be freed from this debarment if he/she was unable to exercise his/her rights within the prescribed time interval, if the injury worsens or “ for any other legitimate reason ”. The fact that the victim is a child suspends the time restriction; the victim can pursue the matter before the CIVI up until his/her 21st birthday.
Any compensation awarded by the CIVI is paid out of the national Victims of Terrorism and other Offenses Fund. Given that the cases for compensation are quite burdensome for the Fund, the CIVI tends to appoint a medical expert to re-evaluate the sequelae.
Proceedings before the CIVI do not prevent the victim from acting as a plaintiff in court against the perpetrator of the acts, although the commission is not obliged to wait for the end of legal proceedings before compensating the victim. The CIVI may be petitioned immediately, without waiting for the end of legal proceedings, by the ad hoc legal guardian or even by a parent. If the court awards more compensation that has been granted by the CIVI, the victim can petition the latter for additional compensation.
After the trial (before the Magistrates Court or the Court of Assizes), the matter can be referred to the CIVI with a view to obtaining full compensation on the basis of the expert medical opinion. Petitioning the CIVI before the trial is always possible but it is advisable to be in possession of the latest legal and medical evidence.
1.5.2
Second hypothesis: a diagnosis of “possible” SBS
If the diagnosis is one of “possible” SBS, the hospital team must consider the child’s situation: does home discharge pose a potential danger to the child? Does the child need protection?
1.5.2.1
Must “concern” be disclosed?
If the medical diagnosis is one of “possible” SBS, the medical team’s multidisciplinary evaluation may prompt it to consider that the infant may be in danger (as defined in article 375 of the Civil Code 19
19 “If the health, safety or morality of a non-emancipated minor are in danger or if its education or physical, affective, intellectual and social development are seriously compromised”.
) and that protective measures may be required.Article L. 226-3 of the Family and Social Action Code (as modified by the 2007 Child Protection Act) states that “The Chairperson of the County Council is responsible for gathering, processing and evaluating (at any time and regardless of the source) disclosures of concern for children in danger or who may become so. The representative of the State and the legal authorities shall provide the said Chairperson with their assistance. A process for determining the procedures for collaboration between the State, the legal authorities, cooperating institutions and not-for-profit associations must be established.”
In this respect, the hospital staff must report their concern 20
20 The 2007 Child Protection Act clearly distinguishes between a report to the district prosecutor on one hand and “concern” reported to the County Child Abuse Prevention Office on the other. According to the law, “concern” relates to any situation in which one or more professionals are concerned that the child is in danger or may become so (as defined in article 375 of the Civil Code).
to the County Child Abuse Prevention Office (referred to as a CRIP, Cellule de recueil, de traitement et d’évaluation des informations préoccupantes, in most counties), in compliance with article L. 226-3 of the Family and Social Action Code.The protocol established between the County Council, the prosecutor, the hospitals and other professionals likely to become aware of cases of shaking (in compliance with the 2007 Child Protection Act) should include clear, valid instructions for the county as a whole.
It is recommended that each CRIP should include a physician for exchanging and processing medical information.
1.5.2.2
Why should “concern” be disclosed?
When the diagnosis of shaking is only “possible”, notifying the CRIP of concern enables the need for child protection and parental support to be considered without necessarily triggering legal proceedings.
The CRIP may use or complete the evaluation performed by the hospital team or, in the absence of an existing evaluation, decide to perform one.
The treatment of the concern must be performed in a delay as short as possible and no longer than 1 month, whether the evaluation is performed by the CRIP itself or field-based experts.
However, a report to the district prosecutor can be made by the CRIP immediately or following the evaluation, if it turns out that the act is likely to be a crime or if protection of the child appears to be necessary and cannot be given by the latter’s parents. The district prosecutor can also be petitioned if it is impossible to evaluate the situation.
1.5.2.3
What information should be given to the parents following a disclosure of concern?
The parents must be informed when a disclosure of concern involves their child, except when this is counter to the child’s interest.
Article L. 226-2-1 of the Family and Social Action Code states that “except when against the child’s interests, the father, mother and other persons holding parental authority or the guardian are informed prior to this transmission through appropriate channels”.
It is best to explain to the parents that the goal of disclosure of concern is to evaluate whether there is a need to protect their child but also to help them because are in a difficult situation with their child.
When administrative protection is suggested, the county office must inform the parents of the reasons why protection has been considered, by emphasizing the child’s interests. It is recommended to initiate a continuous dialogue according to the spirit of the 2007 Child Protection Act.
1.5.2.4
Administrative protection
If the parents give their approval and when necessary, administrative protection can be given. The Chairperson of the County Council can, with the parents’ approval, implement administrative protection in various forms 21
21 Article 223-1 of the Family and Social Action Code: “The county services and the holders of the parental authority shall together draw up a document called a ‘Plan for the Child’ that specifies the measures to be taken with respect to the child, the parents and their environment, the parents’ role, the objectives and the timelines for implementation. It shall state the institution and the person charged with ensuring that the measures are coherent and that they proceed correctly. This document is countersigned by the Chairperson of the County Council, the child’s legal representative and representatives of each organisation charged with implementing the measures. The child is informed of the plan and, in application of article L. 223-3-1, the plan is sent to the judge. On the basis of the information in his/her possession, the Chairperson of the County Council shall ensure that the child protection measures for the child and its family have been and continue to be implemented.”
, while bearing in mind their parental rights and helping them to exercise the said rights.If the parents refuse the principle of protection or the protective measures, the Chairperson of the County Council may refer the matter to the district prosecutor. He/she may also petition the latter if the implemented administrative protection is not sufficient to adequately protect the child 22
22 Art. L. 226-4 of the Family and Social Action Code. “The Chairperson of the County Council shall immediately inform the district prosecutor when a child in danger as defined in article 375 of the Civil Code and: (1) that it has already been subject to one or several measures mentioned in articles L. 222-3 and L. 222-4-2 and the first part of the article L. 222-5 and that the said measures have not resolved the situation; (2) that even though the child is not subject to the measures mentioned in (1), the said measures cannot be implemented due to the family’s refusal or inability to accept involvement by the child protection services.” “He/she shall also immediately inform the district prosecutor when a child is presumed to be in danger (as defined in 375 of the Civil Code) but when it is impossible to evaluate this situation.”
.1.5.2.5
Parental support
If child protection does not appear to be necessary but, after evaluation, the family situation nevertheless suggests the need for temporary assistance, certain parental support measures can be envisaged with the parents (whether individual or group-based, at home or outside the home).
All deployable resources must be sought within in or near to the family environment, in order to help the parents in their duties. In general, personal problems and life problems experienced by people looking after children should act as a warning sign for any professionals who know about them.
It is important to offer and implement appropriate assistance. Referral to child protection staff (notably through home visits) must be considered. “Parent and child drop-in points” at which the relationship between the parents and the child can be built or strengthened are recommended solutions.
1.5.3
Practical guidelines
In all cases, “all decisions must be guided by the child’s interest and consideration for its fundamental, physical, intellectual, social and affective needs and the defence of its rights”, in compliance with the first article of France’s 2007 Child Protection Act (codified as article L. 112-4 of the Family and Social Action Code).
1.5.3.1
Guidelines for hospital staff
1.5.3.1.1
Team coordination
For a diagnosis of “probable” SBS, the medical team (at least two healthcare professionals) must meet and review the symptoms and the reported facts, pool and compare the gathered information, make a diagnosis, consider (as appropriate) any other associated mistreatment, clarify each person’s positions and discuss whether a report should be filed. This meeting must take place without delay must be summarized in writing.
In addition, a multidisciplinary medical, psychological and social evaluation of the situation is essential, in order to analyse the child’s situation, identify risk factors, consider the child’s outcome and consider child protection measures. Consulting with colleagues is never a waste of time. The healthcare professional should not confuse speed with haste.
1.5.3.1.2
Reporting
Each hospital service should define the disclosure procedures to be followed by its staff in cases of shaking, as follows:
- •
establish an initial, emergency report that includes the essential information (see the textbox above: Section 1.5.1.6 ), and then add further information after a multidisciplinary evaluation;
- •
the report should be signed by the attending hospital physician and social services staff. In some cases, it may be completed by the psychologist or psychiatrist who has interviewed the family. It is essential to provide investigators with information on the context and the latter’s compatibility with the medical facts;
- •
the report should be sent by fax and by registered post with signed-for delivery, while keeping a copy for the hospital records;
- •
if the report is sent directly to the district prosecutor’s office, a copy must be sent to the Chairperson of the County Council.
An ordonnance of placement provisoire (OPP) ordered à titre conservatoire by the district prosecutor will not influence subsequent legal proceedings and is recommended – if only to provide the child with immediate protection.
Disclosure should be made as quickly as possible, in order to provide the child with immediate protection and not jeopardize the inquiry: the sooner after the event the report is filed, the sooner an effective criminal inquiry can start.
In this respect, the County’s procedure (established in compliance with the 2007 Child Protection Act and involving the council itself, the district prosecutor’s office, hospitals and other parties likely to be aware of children in danger in general and shaking victims in particular) should contain advice that is clear and is applicable to the county as a whole.
As soon as a diagnosis of SBS is stated as the cause of (or one of the causes of) an infant’s death, the physician who delivers the death certificate must mention the fact that this death raises legal issues.
1.5.3.1.3
Dialogue with the parents and the family
In the diagnostic phase, dialogue with the parents is essential – notably in order to note their explanations concerning the child’s injuries. Issues such as forming an opinion on the circumstances of and justifications for shaking, identifying the perpetrator and deciding whether the latter should be prosecuted are not diagnostic objectives and are the sole responsibility of the district prosecutor.
The physician should inform the parents that in light of the severity of their child’s condition, the district prosecutor’s office will be contacted. He/she should also specify that the district prosecutor will decide on any further actions to be taken. This approach, which means taking time and making an effort to listen, is best led by a senior physician in the presence of another staff member. It is essential to try to make the parents understand that the goal is not simply to denounce them but to draw attention to a dangerous situation and protect their child.
The parents must be informed of the report (except when counter to the child’s interest), the possibility that an OPP may be issued by the district prosecutor and the possibility of filing a complaint against person or persons unknown if they deny the shaking and attribute it to someone else.
However, this necessary dialogue and the obligation to provide the parents with information must not hinder or jeopardize the criminal inquiry.
1.5.3.1.4
Exchanging information with the district prosecutor’s office
We recommend the use of a form for exchanging information between the district prosecutor’s office and the reporting person. To initiate this practice, the form should feature in the reporting procedure.
1.5.3.1.5
Requisition of medical records
It is advisable to photocopy requisitioned documents prior to their transmission, in order to (i) comply with the healthcare establishment’s obligation to store its medical data and (ii) counter the risk of not having the seized items returned.
It is advisable to request the return of requisitioned items. This request must be sent to the investigating judge if the latter is involved in the legal proceedings (article 99, paragraph 1 of the Code of Criminal Procedure) or to the ruling jurisdiction if the prosecution is over (Article 373 and article 484, paragraph 2 of the Code of Criminal Procedure).
1.5.3.1.6
Disclosure of concern
To disclose concern to the County Child Abuse Prevention Office (CRIP), the physician should follow the county’s procedure, in compliance with article L. 226-3 of the Family and Social Action Code 23
23 “… procedures to this end must be established by the Chairperson of the County Council, the State’s representative in the county and the legal authorities with a view to centralizing disclosures of concern within a specialist unit for gathering, processing and evaluating this information within the County Child Abuse Prevention Office”.
.1.5.3.2
Guidelines for non-hospital-based medical staff
A medical condition that is as serious as SBS requires hospitalisation. Private practitioners and staff in child protection units should refer the child towards a paediatric care unit if they are in any doubt as to potential SBS.
The physician who refers the child must first contact the hospital staff. He/she must check that the infant is admitted by the parents. If not, the physician remains fully responsible for the child’s safety).
Private practitioners and child protection units must be trained to diagnose SBS and refer cases to appropriate bodies.
Joint continuing professional education sessions on SBS must be organized for all physicians practising outside hospital.
1.5.3.3
Guidelines for staff in county services
A disclosure of concern concerning SBS must be processed as rapidly as possible (within one month at most) by the CRIP itself or by field-based professionals (in the district or from voluntary organizations).
Each CRIP should appoint a physician responsible for promoting the exchange and processing of medical information.
It is recommended of maintain continuous dialogue with the parents, in the spirit of and subject to the provision of the 2007 Child Protection Act. The objective is to not only protect the child but also to help parents in difficulty with their infant.
County staff must inform the parents and obtain their consent for any administrative care procedures, in compliance with the parents’ rights and by encouraging the exercise of the said rights.
1.5.3.4
General guidelines
1.5.3.4.1
For professionals dealing with infants
Initial training, continuous professional education and staff support must be implemented in order to maintain high levels of awareness.
In general, any professional likely to become aware of shaking in some way must receive at least basic training on this issue: social services staff, child care managers, magistrates, police officers, etc.
When justified by the context, it is advisable to identify all the resources that can potentially be leveraged in the family environment to help parents better fulfil their role. In general, personal problems experienced by people looking after children should act as a warning sign for social services staff and healthcare professionals.
1.5.3.4.2
For parents and families
It is advisable to organise frequent, appropriate awareness-raising and information campaigns (targeted at people in contact with infants, above all) on the dangers of shaking and the precautions that should be taken.
In maternity wards and in the days following discharge to home, parents should always be made aware of the danger of shaking.
“Parent and child drop-in points” at which the relationship between the parents and the child can be built or strengthened are recommended solutions.
It is important to offer appropriate support to parents and implement support measures when requested. Referral to child care professionals (notably with home visits) must be envisaged. The same is true for various forms of home help (provided by the social services).
1.5.3.4.3
In the child’s interest
We recommend that France borrows elements of Canadian law in which an ad hoc legal guardian can be appointed whenever necessary in the child’s interest and in defence of the child’s rights.
2
Version française
Ce texte est composé de trois parties. La première consacrée au diagnostic de secouement (signes d’appel, facteurs de risque, investigations à mener, lésions possibles) se conclut par la proposition de critères diagnostiques fondés sur l’histoire clinique et les lésions.
La deuxième partie étudie la possibilité pour des mécanismes souvent allégués telle la chute ou les manœuvres de réanimation d’induire des lésions comparables à celles du SBS. Elle étudie également l’éventualité de facteurs favorisant la survenue de lésions.
La troisième partie, enfin, est consacrée aux conséquences (dans le contexte réglementaire et législatif français) du diagnostic de secouement.
2.1
Abréviations
CIVI
commission d’indemnisation des victimes d’infraction pénale
CRIP
cellule de recueil, de traitement et d’évaluation des informations préoccupantes
EESA
expansion des espaces sous-arachnoïdiens
HR
hémorragie rétinienne
HAS
Haute Autorité de santé
HED
hématome extradural
HSD
hématome sous-dural
IRM
imagerie par résonance magnétique
ITT
incapacité totale de travail
OPP
ordonnance de placement provisoire
SBS
syndrome du bébé secoué
TC
traumatisme crânien
TCI
traumatisme crânien infligé
2.2
Participants
Cette audition publique a été organisée par la Société française de médecine physique et de réadaptation (Sofmer), avec les partricipations suivantes :
- •
Collège national des généralistes enseignants
- •
Inserm
- •
InVS
- •
Société française d’anesthésie-réanimation
- •
Société française de médecine d’urgence
- •
Société française de médecine légale
- •
Société française de neurochirurgie pédiatrique
- •
Société française de neuropédiatrie
- •
Société française de pédiatrie
- •
Union nationale des associations de familles de traumatisés crâniens et cérébro-lésés (UNAFTC)
2.2.1
Financement
- •
Caisse primaire d’assurance maladie des professions libérales de province
- •
Direction générale de la santé
- •
France traumatisme crânien
- •
Société française de médecine physique et de réadaptation
- •
Société francophone d’étude et de recherche sur les handicaps de l’enfance
- •
Caisse primaire d’assurance maladie des professions libérales d’Île-de-France
2.2.2
Comité d’organisation
- •
Dr Anne Laurent-Vannier, médecin de médecine physique et de réadaptation, Saint-Maurice – présidente du comité d’organisation
- •
Dr Juliette Bloch, médecin épidémiologiste, InVS, Saint-Maurice
- •
M. Thierry Boulouque, commissaire divisionnaire, chef de la brigade de protection des mineurs, Paris
- •
Dr Jeanne Caudron-Lora, urgentiste, Créteil
- •
Pr Brigitte Chabrol, pédiatre, Marseille
- •
M. Frédéric de Bels, HAS, Saint-Denis La Plaine
- •
Dr Patrice Dosquet, HAS, Saint-Denis La Plaine
- •
Mme Françoise Forêt, professeur honoraire, Union nationale des associations de familles de traumatisés crâniens et cérébro-lésés (UNAFTC), Paris
- •
Dr José Guarnieri, neurochirurgien, Valenciennes
- •
Pr Vincent Gautheron, médecin de médecine physique et de réadaptation, Saint-Étienne
- •
Dr Cyril Gitiaux, pédiatre, Paris
- •
Mme Anne-Sophie Jarnevic, magistrat, Chartres
- •
Mme Thérèse Michel, assistante sociale, Tours
- •
Pr Gilles Orliaguet, anesthésiste-réanimateur, Paris
- •
Dr Claude Rougeron, médecin généraliste, Anet
- •
Pr Michel Roussey, pédiatre, Rennes
- •
M. Yvon Tallec, magistrat, Paris
- •
Pr Gilles Tournel, médecin légiste, Lille
- •
Dr Anne Tursz, directeur de recherche, Inserm, Villejuif
2.2.3
Commission d’audition
- •
Dr Mireille Nathanson, pédiatre, Bondy – coprésidente de la commission d’audition
- •
Mme Fabienne Quiriau, directrice de la Convention nationale des associations de protection de l’enfant (CNAPE), Paris – coprésidente de la commission d’audition
- •
Mme Aurélie Assié, assistante sociale, Aide sociale à l’enfance de Paris, service d’accueil familial, Ecommoy
- •
Dr Joseph Burstyn, ophtalmologiste, Paris
- •
Dr Christine Cans, pédiatre, Grenoble
- •
Dr Catherine Arnaud, pédiatre, Toulouse
- •
Mme Violaine Chabardes, gendarme, Lyon
- •
Mme Hélène Collignon, journaliste, Paris
- •
Dr Marie Desurmont, médecin légiste, Lille
- •
Mme Isabelle Gagnaire, infirmière puéricultrice, Saint-Étienne
- •
Pr Nadine Girard, radiologue, Marseille
- •
Pr Étienne Javouhey, réanimateur, Lyon
- •
Dr Anne Laurent-Vannier, médecin de médecine physique et de réadaptation, Saint-Maurice
- •
M. Philippe Lemaire, magistrat, Paris
- •
Dr Caroline Mignot, pédiatre, Paris
- •
Dr Sylviane Peudenier, neuropédiatre, Brest
- •
Dr Bruno Racle, pédiatre, Versonnex
- •
Dr Pascale Rolland-Santana, médecin généraliste, Paris
- •
Dr Thomas Roujeau, neurochirurgien, Paris
- •
Dr Nathalie Vabres, pédiatre, Nantes
- •
Mme Roselyne Venot, fonctionnaire de police, Versailles
2.2.4
Chargés de la synthèse bibliographique
- •
Dr Élisabeth Briand-Huchet, pédiatre, Clamart
- •
M. Jon Cook, anthropologue, Villejuif
2.2.5
Experts
- •
Pr Thierry Billette de Villemeur, pédiatre, Paris
- •
Pr Jean Chazal, neurochirurgien, Clermont-Ferrand
- •
Pr Catherine Christophe, radiologue, Bruxelles
- •
Dr Sabine Defoort-Dhellemmes, ophtalmologiste, Lille
- •
Dr Gilles Fortin, pédiatre, Montréal
- •
Dr Caroline Rambaud, médecin légiste, Garches
- •
Pr Jean-Sébastien Raul, neurochirurgien, Strasbourg
- •
Dr Caroline Rey-Salmon, pédiatre, Paris
- •
M. François Sottet, magistrat, Paris
- •
Mme Élisabeth Vieux, magistrat honoraire, Paris
- •
Pr Mathieu Vinchon, neurochirurgien, Lille
- •
Pr Rémy Willinger, professeur de mécanique, Strasbourg
Iconographie mise à disposition par la Société francophone d’imagerie pédiatrique et prénatale (SFIPP).
2.3
Rapport d’orientation. Quelle est la démarche diagnostique du secouement ?
2.3.1
Définition du syndrome du bébé secoué
Le SBS est un sous-ensemble des traumatismes crâniens (TC) infligés (TCI), ou TC non accidentels ( abusive head trauma ) , dans lequel c’est le secouement (seul ou associé à un impact) qui provoque le TCI. Le SBS survient le plus souvent chez un nourrisson de moins d’un an : dans les trois études réunissant le nombre le plus important de cas (King et al. au Canada en 2003 , Mireau en France en 2005 , Programme canadien de surveillance pédiatrique (PCSP) en 2008 ), l’âge médian est 4,6 et cinq mois respectivement chez King et al. et PCSP , l’âge moyen est de 5,4 mois chez Mireau (dans cette série, les nourrissons les plus jeunes ont un mois).
Les articles de la littérature concernent la plupart du temps les TCI et non uniquement le SBS, de ce fait les réponses apportées aux questions se rapportent souvent aux TCI.
L’incidence du SBS varie entre 15 et 30/100 000 enfants de moins d’un an . Si l’on rapporte ces résultats au chiffre des naissances en France, on peut estimer que 120 à 240 nourrissons pourraient être concernés chaque année par cette maltraitance. Mais il n’existe pas de données épidémiologiques françaises ; Mireau avance le nombre de 180 à 200 cas par an .
Les chiffres publiés sous-estiment certainement la réalité. En effet :
- •
ils font surtout état des cas les plus sévères, qui eux-mêmes ne sont probablement pas tous répertoriés ;
- •
l’absence d’autopsie systématique des nourrissons décédés d’une mort inattendue empêche de faire certains diagnostics ;
- •
il est souvent difficile de différencier TCI et TC accidentels.
La méconnaissance du diagnostic fait courir un risque de récidive de la maltraitance ; des publications font état de ce risque ; une étude rétrospective récente portant sur 112 enfants identifie une répétition du secouement (de deux à 30 fois, dix fois en moyenne) dans 55 % des cas.
2.3.2
Quels sont les éléments (signes cliniques, contexte, facteurs de risque, etc.) pouvant ou devant faire évoquer le diagnostic de syndrome du bébé secoué, ou risquant d’égarer le diagnostic ?
2.3.2.1
Signes et symptômes initiaux
Il existe une grande hétérogénéité clinique :
- •
dans les cas les plus graves, l’enfant a été trouvé mort. La conduite à tenir en ce cas est précisée plus loin ;
- •
l’enfant présente des signes évoquant d’emblée une atteinte neurologique grave, imposant une prise en charge immédiate :
- ∘
convulsions,
- ∘
malaise grave décrit par les parents (« j’ai cru qu’il allait mourir », « il s’est arrêté de respirer ») ou constaté par le médecin (trouble grave de la conscience, pauses respiratoires, bradycardie),
- ∘
troubles de la vigilance allant jusqu’au coma,
- ∘
apnées sévères : très spécifiques des TCI par rapport aux TC accidentels (dans l’étude de Maguire et al. leur valeur prédictive positive est de 93 %),
- ∘
plafonnement du regard,
- ∘
signes orientant vers une hypertension intracrânienne aiguë, voire précédant un engagement : troubles de la posture (décortication ou décérébration, accès d’hypertonie), bradycardie, hypertension artérielle, troubles du rythme respiratoire ;
- ∘
- •
l’enfant présente des signes qui doivent orienter vers une atteinte neurologique :
- ∘
modifications du tonus (hypotonie axiale),
- ∘
moins bon contact (enfant répondant mal aux stimuli, ne souriant plus),
- ∘
diminution des compétences de l’enfant,
- ∘
macrocrânie avec cassure vers le haut de la courbe (importance du carnet de santé),
- ∘
bombement de la fontanelle ;
- ∘
- •
l’enfant présente des signes non spécifiques pouvant égarer le diagnostic :
- ∘
modifications du comportement décrites par les accompagnants : pleurs, geignement, irritabilité, modifications du sommeil, mauvaises prises alimentaires, moins de sourires,
- ∘
vomissements,
- ∘
pauses respiratoires,
- ∘
pâleur,
- ∘
bébé qui semble douloureux.
- ∘
De toute façon, l’examen doit être minutieux et complet, sur un nourrisson dénudé, comprenant en particulier la palpation de la fontanelle et la mesure du périmètre crânien, à reporter sur la courbe, la recherche d’ecchymoses sur tout le corps, y compris sur le cuir chevelu.
Étant donné la non-spécificité de plusieurs de ces signes, leur association prend tout son intérêt ( Tableau 1 ). Ainsi les vomissements, qui sont un symptôme très fréquent et banal, doivent alerter s’ils sont associés à une fontanelle bombée, une hypotonie axiale, des troubles de la vigilance ou une cassure vers le haut de la courbe de périmètre crânien.
| Signes observés | Fréquence (%) |
|---|---|
| Hypotonie axiale et crise comitiale | 53 |
| Crise comitiale et tension de la fontanelle | 46 |
| Vomissements et tension de la fontanelle | 38 |
| Vomissements et hypotonie axiale | 34 |
| Cassure de la courbe de périmètre crânien et tension de la fontanelle | 31 |
| Vomissements, crise comitiale et tension de la fontanelle | 25 |
| Vomissements et troubles de la vigilance | 24 |
| Vomissements, hypotonie axiale et tension de la fontanelle | 23 |
| Vomissements, trouble de la vigilance et tension de la fontanelle | 19 |
Les signes qu’on vient de décrire sont également à rechercher dans les antécédents de l’enfant (carnet de santé) car ils peuvent témoigner d’un éventuel TC antérieur.
Certaines données de l’anamnèse peuvent évoquer un TCI :
- •
retard de recours aux soins, manque de réactivité de l’entourage ;
- •
absence d’explications des signes cliniques observés :
- ∘
dans la série de Mireau , l’entourage ne décrit aucun traumatisme quel qu’il soit dans 71,6 % des cas, malgré des interrogatoires répétés,
- ∘
pour Hettler et Greenes , le fait qu’aucune histoire traumatique ne soit d’emblée évoquée est très discriminant des TCI par rapport aux TC non infligés (69,3 % des cas versus 3 % [ p < 0,001]), avec une haute spécificité [0,97] et une valeur prédictive positive élevée [0,92] ;
- ∘
- •
plus évocatrices, des explications non plausibles : par exemple, ecchymoses chez un bébé qui ne se déplace pas ;
- •
histoire changeante selon le moment ou l’interlocuteur ;
- •
histoire rapportée spontanément d’un TC minime ;
- •
enfant qui est décrit comme pleurant beaucoup, ou qui a déjà consulté pour pleurs ;
- •
antécédent de traumatisme, quel qu’il soit ;
- •
antécédent de mort non ou mal expliquée dans la fratrie.
Suspecter le diagnostic de secouement doit conduire le médecin à faire part aux parents de son inquiétude sur l’état de l’enfant et à poser l’indication d’une hospitalisation en urgence.
2.3.2.2
Peut-il y avoir un intervalle libre entre le secouement et le début des signes ?
Différentes études établissent que la plupart du temps il n’y a pas d’intervalle libre :
- •
Willman et al. , dans une étude rétrospective portant sur 95 enfants ayant eu un TCI ayant entraîné la mort, concluent que, en dehors des cas où il existe un HED, il n’y a pas d’intervalle libre ;
- •
Starling et al. établissent que dans les cas où le secouement (avec ou sans impact) avait été reconnu, les symptômes étaient apparus immédiatement après le traumatisme 52 fois sur 57 ; dans cinq cas, il était difficile de dater le début des symptômes, mais le délai était inférieur à 24 heures ;
- •
pour Biron et Shelton également, sur 52 cas de secouement investigués par la police et considérés comme « sérieux », lorsque la description du cas était complète, les symptômes étaient immédiats.
Il semble donc que dans la grande majorité des cas, sinon dans tous les cas de SBS, le secouement entraîne immédiatement des symptômes. Cela est à différencier du délai qui peut exister entre le secouement et la consultation.
2.3.2.3
Facteurs de risque de traumatisme crânien infligé
Il est important de rappeler qu’un facteur de risque est une variable statistiquement associée à un phénomène, une pathologie ou un syndrome, sans pour autant en être la cause.
2.3.2.3.1
Facteurs de risque liés à l’enfant
Sex-ratio : prédominance des garçons (sex-ratio G/F entre 1,3 et 2,6).
Prématurité : taux de prématurité plus élevé que dans la population générale : 11 à 21 % (11 % dans la série de Mireau ) versus 7 à 8 % dans la population générale.
Grossesses multiples : elles seraient plus fréquentes (gémellité dans 5 % des cas de Mireau ) que dans la population générale (1,5 % de grossesses multiples).
Les pleurs ne peuvent être considérés comme un facteur de risque à proprement parler, mais ils peuvent être un élément déclenchant de comportement maltraitant envers les nourrissons , sachant que la tolérance des parents aux pleurs de l’enfant est très variable : une consultation pour pleurs d’un nourrisson ne devrait pas avoir pour seul but de trouver la cause des pleurs, mais également d’évaluer le ressenti et les réactions des parents à ces pleurs.
2.3.2.3.2
Facteurs de risque liés à l’auteur des faits
Dans les séries où l’auteur des faits a été identifié, qu’il y ait eu ou non aveu de sa part, cet auteur est dans la majorité des cas (70 %) un homme, le père plus souvent que le compagnon de la mère.
Les adultes non apparentés constituent également une catégorie significative d’auteurs potentiels de maltraitance : dans la série de 151 cas de TCI examinés par l’équipe de Starling , les boyfriends de la mère sont en cause dans 20,5 % des cas, les baby-sitters de sexe féminin dans 17,3 % des cas.
2.3.2.3.3
Facteurs de risque liés aux parents
En ce qui concerne le contexte socio-économique, les études sont très contradictoires, tous les milieux peuvent être concernés ; les facteurs de vulnérabilité évoqués restent à documenter (premier enfant, nouvelle grossesse, reprise du travail, méconnaissance des besoins et des comportements normaux de l’enfant, isolement social et familial, histoire de violences familiales, troubles psychiatriques passés ou présents, abus de drogue illicite et d’alcool, etc.). Mireau en 2005 note que les parents ont une importante méconnaissance des besoins et comportements normaux de l’enfant. Le jeune âge des parents est fréquemment souligné par les auteurs et signalé comme un facteur de risque potentiel .
Une étude prospective réalisée de janvier 1998 à septembre 2006 détaille le contexte socio-économique de 25 cas de TC non accidentels observés en dix ans dans une région écossaise : 76 % des cas provenaient des quartiers les plus défavorisés du point de vue de l’éducation, de l’instruction et des habiletés sociales, 72 % de ceux où la criminalité était la plus élevée, 68 % de ceux où la santé était la moins bonne, 60 % de ceux où le revenu était le plus bas, 52 % de ceux où la qualité des habitations était la plus mauvaise, 48 % de ceux où le chômage était le plus important.
Ces résultats sont battus en brèche par des études antérieures : deux études de 2000 portant sur la même cohorte d’enfants notent, l’une que la majorité des parents a une situation professionnelle stable (81 % des mères sont sur le marché du travail), l’autre qu’une grande partie des parents a un niveau d’études secondaire ou supérieur.
Écarter le diagnostic de TCI en raison d’un contexte sociofamilial apparemment favorable peut en tout cas être à l’origine de diagnostics « manqués » .
Cependant, d’une façon générale, les difficultés liées au contexte de vie des personnes s’occupant de l’enfant doivent attirer l’attention du professionnel qui en a connaissance.
La relation du SBS avec un facteur ethnique a été étudiée. Fortin fait la synthèse des articles et conclut que l’origine ethnique ne constitue pas un facteur significativement plus associé au SBS qu’au TC accidentel. Les données suggèrent plutôt que la variable « origine ethnique » constitue un facteur de risque lié à d’autres marqueurs sociaux qui augmentent chez l’enfant le risque de blessures.
En résumé , les données disponibles à ce jour, bien que parcellaires et parfois contradictoires, suggèrent que les enfants de sexe masculin, premiers-nés, âgés de moins de six mois, nés prématurément d’une grossesse compliquée ou multiple, vivant avec des parents ayant une histoire présente ou passée d’abus de substances psychoactives (alcool, drogues) ou de violence familiale et/ou ayant une méconnaissance des stratégies de gestion de la relation avec leur nourrisson, sont plus à risque d’être victimes du SBS. Cet acte de violence peut bien sûr survenir sans qu’il y ait de tels facteurs de risque socio-économiques et culturels. De plus, s’il peut être juste de penser que l’enfant victime de SBS appartient plus souvent au groupe à risque ci-dessus, il est faux de croire que la majorité des enfants présentant ces caractéristiques sont victimes de cette forme de maltraitance.
2.3.3
Quelles sont les lésions et quel est le bilan clinique et paraclinique nécessaire et suffisant à leur mise en évidence ?
2.3.3.1
Les lésions
2.3.3.1.1
Sont susceptibles d’être lésés dans le SBS les méninges (hémorragies sous-durales ou sous-arachnoïdiennes), l’encéphale, l’œil et la moelle épinière
D’autres lésions peuvent être associées : fractures des membres, des côtes, du crâne, ecchymoses du scalp, hématomes des muscles du cou, lésions rachidiennes postérieures.
Les données les plus précises sont apportées par les séries neuro-anatomopathologiques, mais elles concernent évidemment les formes les plus graves puisque responsables du décès de l’enfant.
Billette , à partir de 93 examens neuropathologiques d’enfants victimes de secouement sans impact crânien visible, décrit :
- •
81 hématomes sous-duraux (HSD), 65 hémorragies sous-arachnoïdiennes, 14 hémorragies intraparenchymateuses, 69 cas d’œdème cérébral, 41 engagements cérébraux ;
- •
56 hémorragies intraoculaires ;
- •
21 lésions de la moelle épinière ;
- •
l’état du rachis n’est pas mentionné ;
- •
les lésions observées ne sont pas spécifiques du mécanisme du décès.
Une autre étude trouve des hémorragies épidurales cervicales et des lésions axonales focales du tronc cérébral et des racines des nerfs spinaux dans 11 cas parmi 37 de TCI et aucun chez 14 cas-témoins, morts d’autres causes.
Différents types de lésions du parenchyme cérébral peuvent être vus :
- •
lésions anoxiques du cortex, des noyaux gris, des thalamus : ces lésions se traduisent par des hypodensités, rarement hémorragiques, associées à une perte de contraste entre les substances blanche et grise ;
- •
œdème cérébral se traduisant par une diminution des espaces liquidiens ;
- •
contusions en particulier dans les régions frontales et temporales, et à la jonction substance blanche–substance grise.
Les collections hématiques extra-axiales (HSD, éventuellement associés à des hémorragies sous-arachnoïdiennes) présentent des caractères particuliers dans le SBS ( Fig. 1–3 ). Elles sont habituellement plurifocales, bilatérales et fines, sans effet de masse. Elles recouvrent la convexité des hémisphères cérébraux, s’accumulent dans la scissure interhémisphérique en position déclive et longent l’insertion de la tente du cervelet. La reconnaissance d’une hémorragie de la faux du cerveau est très évocatrice du diagnostic de SBS , de même que les collections sous-durales de la fosse postérieure (cf. figures ci-dessous). Il faut cependant remarquer que l’HSD n’est pas observé chez tous les bébés secoués : il n’existe que dans 72 à 93 % des cas dans les articles revus par Christophe .











