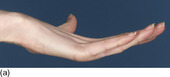
A normal-looking woman complains that she repeatedly sprains her ankles. Examination reveals that she has marked pes planus and valgus hindfeet (Fig. 42.1). She has extremely flexible fingers, wrists, knees and spine (Fig. 42.2).
1 Diagnose this condition.
2 What heritable disorders of connective tissue should be excluded in your diagnosis?
3 How would you grade the severity of this young woman’s condition?
4 What systemic sequelae are associated with this condition?
5 How should this condition be managed?
6 Specifically with regard to her feet, how should the problem of recurrent sprains be managed?
Benign joint hypermobility syndrome
2 Marfan’s syndrome, Ehlers–Danlos syndrome and osteogenesis imperfecta are genetic diseases that include hypermobility as a feature. The skin hyperelasticity, hernias, lens anomalies and abnormal body proportions that typify these conditions are not present in patients with BJHS.
3 This patient scores 9/9 on the Beighton Scale (Table 42.1).
4 Mitral valve prolapse is more prevalent in patients with BJHS, as are uterine prolapse in women, varicose veins, bruising and generally poor wound healing.
5 Education on joint protection is important in BJHS. Strengthening and proprioceptive exercises are recommended to improve joint muscle function.
6 The tendency to recurrent ankle sprains may be lessened by use of antipronatory in-shoe orthoses. Additional supportive strapping or splinting may be helpful (Fig. 42.3).
| Item | Points |
|---|---|
| Passive dorsiflexion of little fingers beyond 90° | 1 point each hand |
| Passive apposition of thumbs to flexor aspects of the forearms | 1 point each hand |
| Hyperextension of knees beyond 10° | 1 point each knee |
| Hyperextension of elbows beyond 10° | 1 point each elbow |
| Forward flexion of the trunk, with knees straight, so the palms of hands rest easily on the floor | 1 point |
Key points
• Marfan’s, Ehlers–Danlos and osteogenesis imperfecta are genetic diseases that include hypermobility as a feature.
• The Beighton Scale is used to grade the severity of this condition.
• Patients with BJHS may have additional health problems.
• Feet are often involved with BJHS and are treated with orthoses and supports.
Further reading
Adib, N; Davies, K; Grahame, R; Woo, P; Murray, KJ, Rheumatology joint hypermobility syndrome in childhood. A not so benign multisystem disorder, Rheumatology 44 (6) (2005) 744–750.
Beighton, P; Grahame, R; Bird, H, Assessment of hypermobility, In: Hypermobility of joints (1983) Springer-Verlag, Berlin, pp. 9–25.
Grahame, R, Time to take hypermobility seriously (in adults and children), Rheumatology 40 (2001) 485–491.
Grahame, R; Bird, H, British consultant rheumatologist’s perceptions about hypermobility syndrome: a national survey, Rheumatology 40 (2001) 559–562.
Russek, LN, Hypermobility syndrome, Physical Therapy 79 (1999) 591–599.
Case 43
A young woman, in her early 20s, has persistent discomfort in the balls of both feet. Pain and stiffness are worse first thing in the morning. Her symptoms began insidiously, without a history of trauma. On examination, there is obvious swelling of the forefoot and the patient has become aware that her toes appear ‘separated’ (Fig. 43.1). Plantar skin lesions are shown in Figure 43.2.
1 This girl has an unusual presentation of metatarsalgia. Of what condition should you be suspicious and how frequently are feet affected with this condition?
2 What name is given to separation of the toes as seen in Figure 43.1?
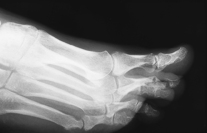
3 Describe the diagnostic radiographic features in Figure 43.3. Is this a common site for this feature?
4 Name the further investigations which are now required.
5 What therapeutic measures should be considered?
 |
| Fig. 43.1 |
 |
| Fig. 43.2 |
 |
| Fig. 43.3 |
Diagnosis of rheumatoid arthritis
2 Joint effusions can lead to spreading of toes, giving rise to the ‘daylight sign’. Inflamed and full bursae are likely to be present over the metatarsal heads on the plantar side.
3 Radiographs of the feet show diagnostic erosions of the fifth metatarsal head. The metatarsal heads are the most common sites of erosive change, with an order of involvement from metatarsal 5, then 3, 2, 4 and 1. The metatarsal head erodes before the base of the proximal phalanx. The distal IP joints are rarely affected.
4 Investigations should include measurement of erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), tests for rheumatoid factor and radiographs. Radiographs may be unremarkable in early disease (see also Table 43.1).
5 Disease-modifying antirheumatic drugs should be considered to retard the erosive process. Specific foot therapy is aimed at ensuring the patient’s footwear is adequately wide at the toe box. Cushioning insoles will also help.
| Laboratory test | Abbreviation | Positive indication for RA | Normal values |
|---|---|---|---|
| Anaemia | (Normochromic or hypochromic, normocytic) | ||
| Thrombocytosis | |||
| • Serum iron concentration | Low | Male: <65 µg/dl | |
| Female: <50 µg/dl | |||
| • Low total iron binding capacity | Low | 250–460 µg/dL | |
| • Serum globulin | Raised | ||
| • Serum alkaline phosphatase | Raised | ||
| Acute phase response | |||
| • Erythrocyte sedimentation rate | ESR | Raised | Male: 1–13 mm/h |
| Female: 1–20 mm/h | |||
| • C-reactive protein concentration | CRP | Raised | <6 mg/l |
| Rheumatoid factor | RF | Present | Titres >1:80 |
| Antinuclear antibodies | ANA | Present | Titres >1:80 |
Key points
• Presentation of pain and swelling in the forefoot without a history of trauma should raise the suspicion of rheumatoid disease, particularly if accompanied by joint pain elsewhere.
• Feet are involved earlier and more frequently than the hands in rheumatoid arthritis.
• MTP joint erosions are diagnostic and indicate the need for second-line drug management.
Further reading
Akil, M; Amos, RS, ABC of rheumatology: rheumatoid arthritis: clinical features, British Medical Journal 310 (1995) 587–590.
Corbett, M; Young, A, The Middlesex Hospital prospective study of early rheumatoid disease, British Rheumatology 27 (suppl II) (1988) 171–172.
Renton, P, Radiology of the foot, In: Disorders of the foot 3rd edn (1991) Blackwell Scientific Publications, London, pp. 272–279.
Case 44
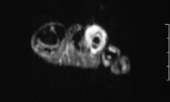
Examination of her left foot reveals a boggy, soft tissue mass on the dorsum of the left third toe (Fig. 44.1). The signs are not typical for a ganglion (see Fig. 10.1) and so an MR scan is requested (Fig. 44.2).
1 What are your differential diagnoses at this stage?
2 What features are revealed on MR imaging (see Fig. 44.2)?
3 How is the condition treated and what is the prognosis for this patient?
 |
| Fig. 44.1 |
 Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|