Myopathies
Emory University School of Medicine, Atlanta, GA, USA
Introduction
Myopathies occur in both adults and children, and may be due to numerous underlying etiologies. Many of the myopathies have similar features, but appropriate classification is critical for proper management. This chapter will focus primarily on the idiopathic inflammatory myopathies and overlap syndromes, and will briefly discuss toxic myopathies.
Common Causes of Myopathy
- Idiopathic inflammatory myopathies (autoimmune-mediated [AIM]): polymyositis (PM), dermatomyositis (DM), inclusion body myositis (IBM), immune-mediated necrotizing myopathy (IMNM)
- Overlap syndromes: connective tissue diseases
- Other rheumatic disease associations: sarcoidosis, IgG4
- Toxic myopathies: statin, colchicine/colcrys, alcohol, cocaine
- Endocrine: thyroid, diabetes
- Neurologic: neuropathies, dystrophies
- Mitochondrial myopathies
- Metabolic myopathies
- Cancer-associated: paraneoplastic, graft-versus-host disease (GVHD)
- Infectious: viral, human immunodeficiency virus (HIV)
- Other: eosinophilic, focal/nodular, macrophagic, granulmatous, orbital/ocular
Idiopathic Inflammatory Myopathies/Autoimmune-Mediated (AIM)
Epidemiology
- The AIM are the most common myopathies, but are still rare
- Annual incidence: adults: 5–10/million, children: 1–5/million
- Prevalence: 50–100 cases/million
Types of Autoimmune-Mediated Myopathies
- Polymyositis (PM)
- Pathogenesis: cytotoxic CD8+ T cells
- Clinical presentation: weeks to months of progressive proximal muscle weakness
- Unique features: interstitial lung disease (ILD), cardiac disease
- Treatment response: good
- Pathogenesis: cytotoxic CD8+ T cells
- Dermatomyositis (DM)
- Pathogenesis: C5b-9 MAC (membrane attack complex), CD4+ T cell perivascular inflammation
- Clinical presentation: weeks to months of proximal muscle weakness
- Unique features: dermatologic manifestations (see physical examination in AIM section)
- Treatment response: good
- Pathogenesis: C5b-9 MAC (membrane attack complex), CD4+ T cell perivascular inflammation
- Inclusion body myositis (IBM)
- Pathogenesis: neurodegenerative
- Clinical presentation: years of progressive muscle weakness
- Unique features: atrophy, asymmetric, distal weakness in addition to proximal weakness
- Treatment response: poor, significant disability
- Pathogenesis: neurodegenerative
- Immune-mediated necrotizing myopathy (IMNM)
- Pathogenesis: myofiber necrosis, degeneration/regeneration, few if any inflammatory cells
- Clinical presentation: not well described
- Unique features: can be drug induced/paraneoplastic
- Treatment response: can respond to immunosuppression
- Pathogenesis: myofiber necrosis, degeneration/regeneration, few if any inflammatory cells
- Myositis associated with connective tissue disease (CTD)
- Pathogenesis: probably a combination of mechanisms
- Clinical presentation: generally proximal muscle weakness, plus features of CTD
- Typically associated with:
- Scleroderma (16–93%)
- Lupus
- Mixed connective tissue disease (MCTD)
- Sjögrens
- Rheumatoid arthritis
- Scleroderma (16–93%)
- Symptoms may be mild to severe
- Pathogenesis: probably a combination of mechanisms
- Juvenile polymositis/dermatomyositis
- Pathogenesis: similar to adult
- Clinical presentation: similar to adult presentation, however DM is more common
- Unique features: painful subcutaneous calcifications can occur, and tend to be more common in pediatric populations
- Pathogenesis: similar to adult
- Amyopathic dermatomyositis
- Pathogenesis: same as DM
- Clinical presentation:
- Skin manifestations without muscle disease or elevated muscle enzymes
- ILD
- May be associated with pneumothoraces or pneumomediastinum
- ILD
- Skin manifestations without muscle disease or elevated muscle enzymes
- Pathogenesis: same as DM
Classification Criteria
The original criteria were defined by Bohan and Peter in 1975.
- These were devised prior to the discovery of myositis-specific antibodies and the recognition of IBM as a separate disease entity
- Patients were assessed by the following criteria:
- Symmetric, proximal muscle weakness
- Rash typical of DM
- Elevated muscle enzymes
- Myopathic changes on electromyography (EMG)
- Characteristic muscle biopsy without signs of other myopathies
- Symmetric, proximal muscle weakness
- Based on the pattern of the above, patients were divided into either probable or definite inflammatory myopathy
International Myositis Assessment and Clinical Studies Group (IMACS)
- Due to the complex nature of myopathies, the IMACS is making efforts to characterize the AIM (Table 6.1) by using a combination of clinical, serologic, histopathological markers, with the production of definite criteria underway
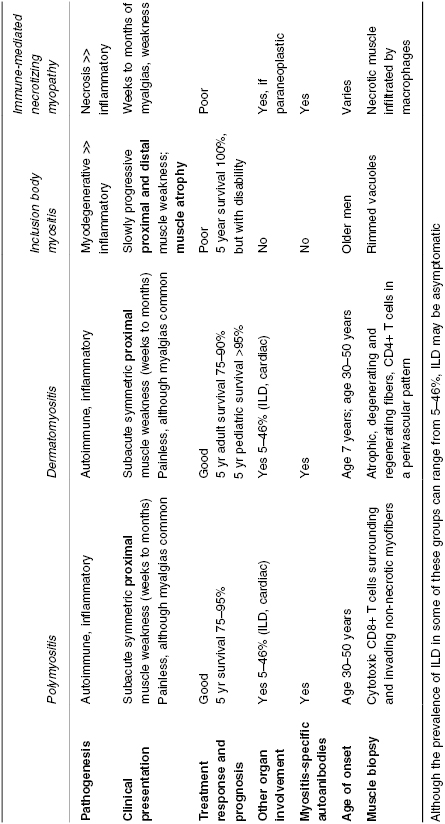
Table 6.1 Summary of classification considerations for AIM, incorporating clinical, serologic and histopathologic components.
Physical Examination in AIM
- Neurologic
- Weakness in proximal muscle groups of upper and lower extremities, neck flexors
- Muscle pain is not a primary feature
- Distal weakness is characteristic of IBM
- Muscle atrophy is characteristic of IBM or late PM/DM
- Note: a patient presenting with weakness over years, asymmetric/distal/facial weakness and scapular winging should prompt evaluation for dystrophy, not myopathy, as a cause of their weakness
- Weakness in proximal muscle groups of upper and lower extremities, neck flexors
- Musculoskeletal
- Synovitis can be present in overlap syndromes
- Dermatologic (primarily seen in DM)
- Heliotrope rash: violaceous papules around eyes
- Gottron papules: erythematous papules, plaques over MCPs, PIPs, DIPs
- Poikiloderma/photosensitive erythematous rash characterized by location:
- Shawl sign: upper back
- V sign: sun-exposed areas of upper chest
- Holster sign: lateral thighs
- Nail bed changes: periungual telangiectasias, cuticular hypertrophy
- Mechanics’ hands: rough, cracked skin over fingertips and lateral aspect of fingers, most commonly seen in antisynthetase syndrome
- Skin changes are typically very photosensitive
- Painful subcutaneous calcifications can also occur, seen primarily in juvenile DM and CTD overlap syndromes
- If dermatologic signs are seen without evidence of associated muscle disease, these patients are categorized as amyopathic dermatomyositis
- Shawl sign: upper back
- Heliotrope rash: violaceous papules around eyes
Laboratory Findings in AIM
- Muscle enzymes
- Creatine kinase (CK): most sensitive and specific
- Aldolase: can be elevated in isolation
- Lactate dehydrogenase (LDH)
- Creatine kinase (CK): most sensitive and specific
- Aspartate transaminase (AST)
- Alanine transaminase (ALT)
- Normal thyroid studies are needed to exclude thyroid disease as a cause of myopathy








