PROCEDURE 51 Total Hip Replacement for Intertrochanteric Hip Fractures
Indications
 All indications should be considered relative as the decision to perform total joint replacement surgery for intertrochanteric hip fractures remains controversial.
All indications should be considered relative as the decision to perform total joint replacement surgery for intertrochanteric hip fractures remains controversial. Patient factor prerequisites:
Patient factor prerequisites:• No major cardiovascular comorbidity (i.e., that would preclude a primary total hip replacement under elective circumstances)
 Relative injury-related indications (in the presence of an intertrochanteric or subtrochanteric fracture):
Relative injury-related indications (in the presence of an intertrochanteric or subtrochanteric fracture):• Complex proximal femoral fracture through osteopenic bone(fixation likely to result in significant malunion, including femoral neck shortening, weakness, and decreased function in a community ambulator)
• Total joint replacement for intertrochanteric hip fractures remains a controversial treatment option at this time. The lack of good quality information regarding the following issues hinders the resolution of this controversy:
 Does immediate total hip replacement result in a better outcome than salvage after failed fixation attempts?
Does immediate total hip replacement result in a better outcome than salvage after failed fixation attempts?
 Does immediate total hip replacement result in a better outcome than salvage after failed fixation attempts?
Does immediate total hip replacement result in a better outcome than salvage after failed fixation attempts?Examination/Imaging
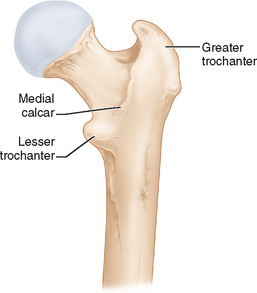
 Careful templating is mandatory to avoid hip instability and leg length inequality. It is better to template the intact side as the fracture significantly distorts the radiographic landmarks on the injured side. The following plain radiographic films are required for this purpose:
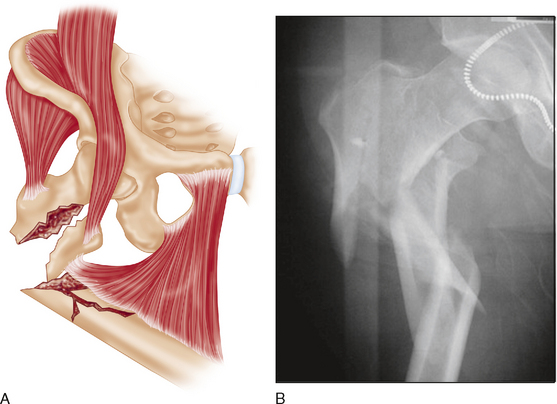
Careful templating is mandatory to avoid hip instability and leg length inequality. It is better to template the intact side as the fracture significantly distorts the radiographic landmarks on the injured side. The following plain radiographic films are required for this purpose:• Anteroposterior (AP) pelvis radiograph centered low to show both hip joints and the affected and intact proximal femurs, as in the AP pelvis radiograph in Figure 1, showing a complex osteopenic proximal femur fracture.
 Pathologic fractures demand a complete local and systemic workup to detect other lesions locally or in other body regions, and to stage the disease overall (prognosis and systemic treatment requirements).
Pathologic fractures demand a complete local and systemic workup to detect other lesions locally or in other body regions, and to stage the disease overall (prognosis and systemic treatment requirements).Portals/Exposures
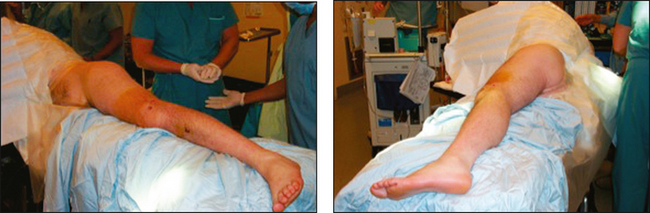
 An oblique incision is made from 2 to 5 cm above the posterior margin of the greater trochanter distally for approximately 8–10 cm (Fig. 7). The incision can be enlarged proximally and distally if needed depending on the size of the patient.
An oblique incision is made from 2 to 5 cm above the posterior margin of the greater trochanter distally for approximately 8–10 cm (Fig. 7). The incision can be enlarged proximally and distally if needed depending on the size of the patient. The iliotibial band is split from distal to proximal, extending into the interval between the tensor fascia lata and the gluteus maximus or into the lateral aspect of the gluteus maximus (Fig. 8).
The iliotibial band is split from distal to proximal, extending into the interval between the tensor fascia lata and the gluteus maximus or into the lateral aspect of the gluteus maximus (Fig. 8). The deep dissection depends on the precise nature of the fracture. The principles are as follows:
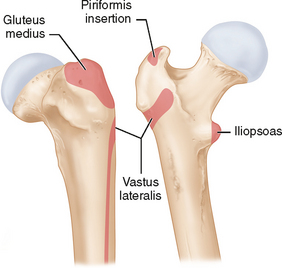
The deep dissection depends on the precise nature of the fracture. The principles are as follows:• The surgeon should spend some time analyzing the bone fragments and soft tissue attachments before detaching soft tissues. The gluteus medius is identified, and the gluteus minimus tendon palpated from anteriorly deep to the abductors. The relationship of muscle disruption to the trochanteric fragments is noted, and if possible areas of muscle disruption are worked through (using a transtrochanteric approach but without dividing the posterior soft tissue attachments from the trochanter).




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree