PROCEDURE 5 Humeral Shaft Fractures
Indications
INDICATIONS FOR OPEN REDUCTION AND INTERNAL FIXATION (ORIF)
• A primary radial nerve palsy can be treated expectantly, and in isolation is not an indication for surgery. Even a secondary nerve palsy, after reduction and splinting, is not considered an absolute indication for surgery by many surgeons.
• Randomized trials have consistently shown that, for routine humeral shaft fractures, ORIF with plate fixation has superior results compared to IM nailing. The main reason for the difference is the higher incidence of postoperative pain and functional limitations, as well as increased rates of reoperation and fracture nonunion with humeral nails. ORIF remains the “gold standard” in the treatment of diaphyseal fractures of the humerus.
Examination/Imaging
 Examination
Examination• Initial assessment and resuscitation of the trauma patient by Advanced Trauma Life Support® or similar protocol
• History and physical examination, including prior injuries or surgery involving the injured extremity
• Neurologic examination and documentation of motor and sensory function of the axillary, musculocutaneous, median, ulnar, and in particular radial nerves
 Imaging
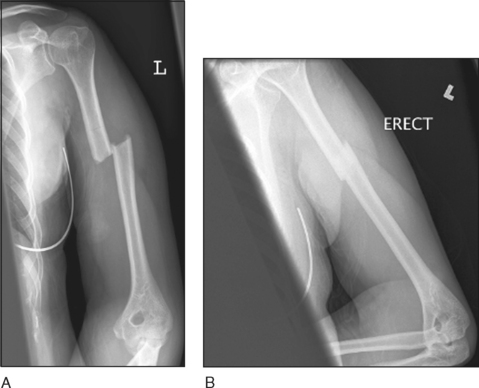
Imaging• Plain radiographs, including anteroposterior (AP) (Fig. 1A) and lateral (Fig. 1B) views of the humerus, are the mainstay of diagnosis and decision making. These should include the elbow and shoulder joints, as well as any other suspected ipsilateral injuries detected on physical examination.
• Fractures of the midshaft or more proximal humerus are best addressed through an anterolateral approach. This allows excellent proximal access, including fixation of proximal humerus fractures, but has limited distal access approaching the antecubital fossa.
• Fractures distal to the midshaft of the humerus are best addressed through a posterior approach. This allows excellent distal exposure, from the elbow joint distally to the surgical neck of the humerus, with proximal dissection limited by the crossing of the axillary nerve.
• Alternatively, a lateral approach may be used for distal fractures, with the advantage of supine positioning.
Surgical Anatomy
• Anterolateral approach
 Adequate visualization and mobilization of the radial nerve will result in a lower risk of nerve injury than blind retraction and potential stretching.
Adequate visualization and mobilization of the radial nerve will result in a lower risk of nerve injury than blind retraction and potential stretching.
 Adequate visualization and mobilization of the radial nerve will result in a lower risk of nerve injury than blind retraction and potential stretching.
Adequate visualization and mobilization of the radial nerve will result in a lower risk of nerve injury than blind retraction and potential stretching.• Posterior approach
 Adequate visualization and mobilization of the radial nerve is mandatory to ensure the nerve is not entrapped in the fracture site or beneath the plate, to avoid the need to re-explore the nerve in the event of postoperative nerve palsy. Careful but thorough mobilization will result in a lower incidence of nerve injury than blind retraction and potential stretching.
Adequate visualization and mobilization of the radial nerve is mandatory to ensure the nerve is not entrapped in the fracture site or beneath the plate, to avoid the need to re-explore the nerve in the event of postoperative nerve palsy. Careful but thorough mobilization will result in a lower incidence of nerve injury than blind retraction and potential stretching.
 Adequate visualization and mobilization of the radial nerve is mandatory to ensure the nerve is not entrapped in the fracture site or beneath the plate, to avoid the need to re-explore the nerve in the event of postoperative nerve palsy. Careful but thorough mobilization will result in a lower incidence of nerve injury than blind retraction and potential stretching.
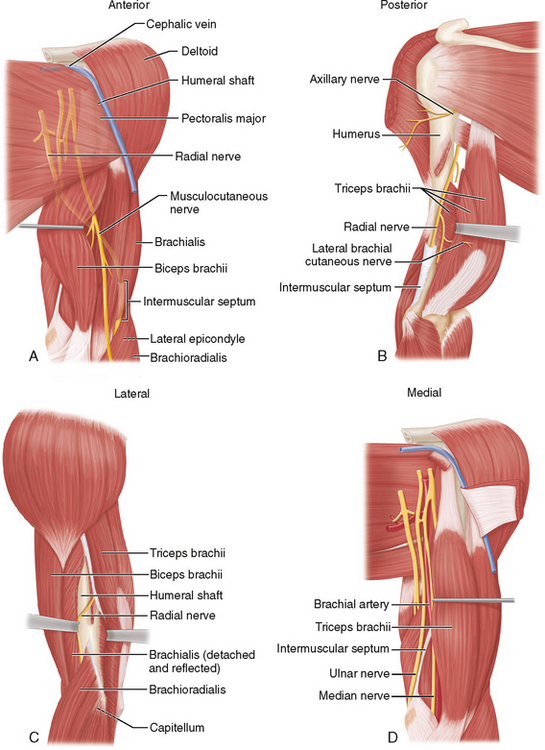
Adequate visualization and mobilization of the radial nerve is mandatory to ensure the nerve is not entrapped in the fracture site or beneath the plate, to avoid the need to re-explore the nerve in the event of postoperative nerve palsy. Careful but thorough mobilization will result in a lower incidence of nerve injury than blind retraction and potential stretching. Anterolateral approach (Fig. 2A)
Anterolateral approach (Fig. 2A)• The cephalic vein is a useful landmark to the interval between the deltoid (axillary innervation) and pectoralis major (pectoral nerve innervation) proximally.
• The musculocutaneous nerve runs along the undersurface of the biceps and should be identified and retracted medially with the biceps muscle (musculocutaneous innervation).
• The radial nerve pierces the intermuscular septum, entering the anterior arm approximately 12 cm proximal to the lateral epicondyle, and should be identified in the interval between the brachioradialis and brachialis.
 Posterior approach (Fig. 2B)
Posterior approach (Fig. 2B)• The radial nerve crosses the posterior humerus obliquely in the spiral groove, from approximately 20 cm proximal to the medial epicondyle to 12 cm proximal to the lateral epicondyle, and then pierces the intermuscular septum, entering the anterior arm.
 Medial approach (Fig. 2D)
Medial approach (Fig. 2D)• The medial approach is within an intraneural plane, with the ulnar nerve posterior to the intermuscular septum, and the median nerve and brachial artery located anteriorly.
Positioning
FOR ORIF
• Anterolateral approach
 Ensure the patient is positioned far enough laterally on the operating table to allow imaging of the humerus through a radiolucent armboard.
Ensure the patient is positioned far enough laterally on the operating table to allow imaging of the humerus through a radiolucent armboard.
 Ensure the patient is positioned far enough laterally on the operating table to allow imaging of the humerus through a radiolucent armboard.
Ensure the patient is positioned far enough laterally on the operating table to allow imaging of the humerus through a radiolucent armboard.• Posterior approach
 Prone positioning requires a secure airway, neutral position of the neck, and adequate eye protection.
Prone positioning requires a secure airway, neutral position of the neck, and adequate eye protection.
 For lateral positioning, consider the use of a chest (axillary) roll to avoid brachial plexus compression (Fig. 6), and pad pressure points appropriately.
For lateral positioning, consider the use of a chest (axillary) roll to avoid brachial plexus compression (Fig. 6), and pad pressure points appropriately.




 Prone positioning requires a secure airway, neutral position of the neck, and adequate eye protection.
Prone positioning requires a secure airway, neutral position of the neck, and adequate eye protection. For lateral positioning, consider the use of a chest (axillary) roll to avoid brachial plexus compression (Fig. 6), and pad pressure points appropriately.
For lateral positioning, consider the use of a chest (axillary) roll to avoid brachial plexus compression (Fig. 6), and pad pressure points appropriately.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree