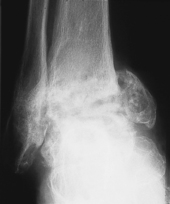
A 72-year-old lady presents to the clinic concerned that she was walking on the outside of her foot. Clinical examination shows that she has a chronically discharging leg sinus (Fig. 32.1). This had been diagnosed as a varicose ulcer. A radiograph showed evidence of bone destruction (Fig. 32.2).
1 What is the likely cause of the radiological appearances?
2 This lady was suffering from minimal pain yet her ankle progressively adopted a varus deformity. What description is applied to painless arthritis?
3 How would you investigate this lady and what treatment is appropriate?
 |
| Fig. 32.1 |
 |
| Fig. 32.2 |
Septic arthritis
2 Painless joint arthritis was described in patients with neurosyphilis by Charcot in 1858. The term ‘Charcot joint’ is now used as a generic term for joint destruction secondary to impaired sensation. The changes are most commonly seen in patients with diabetes mellitus although syphilis (tabes dorsalis), syringomyelia and congenital indifference to pain should also be considered.
3 A swab was sent for culture and sensitivity, but no organisms were grown. This was perhaps not surprising as the patient had been on several courses of antibiotics but both her erythrocyte sedimentation rate, at 86 mm/h, and C-reactive protein, at 350 mg/l, were greatly elevated.
Drainage, with curettage of any necrotic material, is required to hasten healing. In this instance, however, such a procedure would almost certainly have destroyed any residual weight-bearing capacity that the patient had, and the end result would probably have been an amputation.
It was no surprise when the microbiologist finally reported that the infection was due to tuberculosis. The patient was commenced on triple therapy (rifampicin, isoniazid and pyrazinamide) and the discharge diminished dramatically. Eighteen months after starting therapy the radiographic appearance was as shown in Figure 32.3. The patient had no pain and was walking in a surgical shoe with a heel flare, albeit using a stick outside. Although the degree of joint subluxation will almost certainly mean that she will need to wear a leg caliper in the future, this would clearly be preferable to either a joint fusion or amputation. A fusion would not only be technically difficult to achieve in the presence of such significant bone destruction, but it is unlikely that the lady would tolerate a further 6–8 weeks in a plaster cast.
Key points
• All patients should be tested for diabetes mellitus.
• Consider tuberculosis as a cause of chronic sepsis.
Further reading
Dhillon, MS; Nagi, ON, Tuberculosis of the foot and ankle, Clinical Orthopaedics and Related Research 398 (2002) 107; 13.
Laing, P, Surgical management of the Charcot foot, The Diabetic Foot 3 (2000) 44; 8.
Case 33
The patient indicates that his pain arises in his great toe and extends into the dorsum of his foot. Pain occurs after walking for about 5–10 minutes. The pain becomes so intense that he has to stop and rest before the pain eases and he can walk once more. He is also troubled with cramps at night that frequently disturb his sleep. He is a heavy smoker.
On removing his shoes, there is an obvious pallor of his right foot (Fig. 33.1).
1 Which eponym is used to describe the test conducted in Figure 33.2 and what is the physiological principle behind this test?
3 What is your diagnosis and what would be your pathway of care for this patient?
 |
| Fig. 33.1 |
 |
| Fig. 33.2 |
Critical limb ischaemia
This is a useful test to use in conjunction with measurement of the ankle brachial pressure indices when calcification of the arteries is suspected.
2 In the presence of significant disease a number of features can be observed.
With the limbs elevated:
With the limbs dependent:
• the rate of refilling of veins will be sluggish on the affected side
• the time taken for the pallor to subside is also relevant and this time is increased on the right side
• there is increased rubor (dusky red colouration) of the foot as a result of prolonged deprivation of oxygen, known as reactive hyperaemia (see Fig. 33.4). Compare the colour with that evident in Figure 33.1.
3 Critical limb ischaemia. This condition threatens life and limb. A suggested pathway of care is illustrated in Table 33.1.
| Symptoms | Pathway |
|---|---|
| Intermittent claudication without ulceration | Encourage exercise to open up collateral vessels. Smoking cessation. Monitor. |
| Rest pain | Refer to vascular surgeon. Check blood pressure and cholesterol levels, with appropriate drug management if appropriate. |
| Ulceration/gangrene | Establish extent of atherosclerosis. Consider intervention such as grafting, bypass surgery or amputation. |
In this case, the patient was seen urgently by a vascular surgeon. Specialized investigations including Doppler scanning and a femoral angiogram revealed extensive atheroma in the femoral and iliac arteries. A cross-over graft was necessary from the right femoral artery but although, his peripheral arterial circulation improved to 60% of normal, he was unable to return to work.
Lumbar sympathectomy is a minimally invasive procedure with a low complication rate. Three randomized controlled trials have failed to identify any objective benefits for lumbar sympathectomy. However, subjective improvements in symptoms for patients with highly symptomatic critical leg ischaemia have been consistently demonstrated in ten cohort studies, with sustained symptom improvements in approximately 60% of patients. Lumbar sympathectomy should be considered for symptomatic patients with critical leg ischaemia as an alternative to amputation in patients with otherwise viable limbs.
Key points
• Claudication and rest pains are an indication of significant peripheral arterial disease.
• Buerger’s limb elevation is a quick, easy test that does not require expensive equipment.
• Abstinence from tobacco products is the only way to prevent disease progression.
Further reading
Paraskevas, KI; Liapis, CD; Briana, DD; Mikhailidis, DP, Thromboangiitis obliterans (Buerger’s disease): searching for a therapeutic strategy, Angiology 58 (2007) 75–84.
Sanni, A; Hamid, A, Is sympathectomy of benefit in critical leg ischaemia not amenable to revascularisation?. Best BETs. (2005) ; www.bestbets.org (2005).
Sasajima, T; Kubo, Y; Izumi, Y; Inaba, M; Goh, K, Plantar or dorsalis pedis artery bypass in Buerger’s disease, Annals of Vascular Surgery 8 (1994) 248; 57.
Case 34
A 40-year-old holidaymaker is out walking through wet grass adjacent to a Scottish links golf course. He is aware of a sharp ‘stab’ on the top of his foot. Within minutes he is unable to bear weight and on removing his sock, he notices that his skin has been punctured (Fig. 34.1). Six hours later his entire leg is bruised and swollen up to the knee.
1 What is the likely predator?
2 What investigations are appropriate?
3 What should be his acute management?
4 Where may antivenom be obtained?
 |
| Fig. 34.1 |
Snake bite
1 The adder (Vipera berus –Fig. 34.2) is the only indigenous venomous snake in the UK and snakebite is rare but still, as elsewhere in the world, potentially lethal. In the US the two main families of venomous snakes are the Crotalidae (pit vipers, including the rattlesnake, cottonmouth and copperhead) and the Elapidae (coral snakes).
After a bite on the foot or ankle there is rapid peripheral swelling and a spreading inflammatory process (similar to cellulitis) will be evident. Haemorrhagic blebs develop at the site of the bite within 6–36 hours. Palpation of the groin will reveal regional lymphadenopathy and systemic effects are soon apparent. Generally the patient will become nauseous, and vomiting, diarrhoea, incontinence, vasoconstriction and pronounced tachycardia are common. Angio-oedema with swelling of the face and tongue leading to airway obstruction and hypotension may be fatal.
2 Investigations should include examination of a blood film and measurement of serum creatine kinase (indicative of muscle necrolysis). Bleeding is rare but may be secondary to thrombocytopenia. An electrocardiograph will exclude any myocardial ischaemia.
4 Antivenom is obtained through the major hospital casualty departments sourced generally from a National Poisons Centre. Care should always be taken if antivenom is administered as this may also induce anaphylaxis.
 |
| Fig. 34.2 |
Key points
• Venomous pit vipers have triangular heads, elliptic eyes, heat-sensing pits on the sides of their heads, a single row of ventral scales and rattles on the tail.
• Non-venomous pit vipers have rounded heads, spherical eyes, a double row of ventral scales and no rattle.
• Venomous elapids have short fangs, round pupils, a double row of subcaudal scales and red bands bordered by yellow or white as shown in Figure 34.3. A few non-venomous species in the US only are identified by the black band approximating to the red (‘Red to yellow, kill a fellow. Red to black, venom lack’).
• Pressurization will delay venom spread by collapsing small veins and lymphatics.
Further reading
Aurerback, PS; Donner, HJ; Weiss, EA, Snake and reptile bites, In: Field guide to wilderness medicine (1999) St Louis, Mosby, p. 253; 65;
Nuchpraryoon, I; Garner, P, Interventions for preventing reactions to snake antivenom. Cochrane Database of Systematic Reviews. (1999) ; Issue 4.
Warrell, DA, Treatment of bites by adders and exotic venomous snakes, British Medical Journal 331 (2005) 1244; 7.
Case 35
This young nurse presented with a 12-week history of discolouration of her toenail (Fig. 35.1). She first became aware of the lesion when on a ‘holiday in the sun’. According to the patient, the lesion has remained static in size since that time.
< div class='tao-gold-member'>




1 Why is the history of this lesion atypical?
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree