PROCEDURE 44 Anterior Approaches to the Acetabulum
Introduction
 This chapter provides an overview of the anterior surgical approaches for the treatment of acetabular fractures. The keys to treatment include understanding the radiographs, which allows determination of fracture characteristics; use of fracture characteristics to determine the need for surgery and make an appropriate choice of operative approach; and finally, selection of methods of achieving and maintaining anatomic reduction to allow the best possible outcome (Letournel and Judet, 1993; Matta, 1996).
This chapter provides an overview of the anterior surgical approaches for the treatment of acetabular fractures. The keys to treatment include understanding the radiographs, which allows determination of fracture characteristics; use of fracture characteristics to determine the need for surgery and make an appropriate choice of operative approach; and finally, selection of methods of achieving and maintaining anatomic reduction to allow the best possible outcome (Letournel and Judet, 1993; Matta, 1996). The Judet-Letournel classification for acetabular fractures is used by most surgeons around the world. This classification divides the most common fracture patterns into five “elementary” (a part or all of at least one supporting column is detached) and five “associated” (a combination of at least two elementary patterns) types (Judet et al., 1964; Letournel, 1980).
The Judet-Letournel classification for acetabular fractures is used by most surgeons around the world. This classification divides the most common fracture patterns into five “elementary” (a part or all of at least one supporting column is detached) and five “associated” (a combination of at least two elementary patterns) types (Judet et al., 1964; Letournel, 1980).• The five elementary types are posterior wall, anterior wall, posterior column, anterior column, and transverse. The transverse fracture is not “simple” but is included in this group as a result of its purity.
 The goals of treatment reflect those for any articular injury: anatomic reduction of the articular surface; a stable, congruent joint with restored contact area; stable fixation to allow early mobilization of the joint and the patient; and respecting the biology.
The goals of treatment reflect those for any articular injury: anatomic reduction of the articular surface; a stable, congruent joint with restored contact area; stable fixation to allow early mobilization of the joint and the patient; and respecting the biology. The goal of acetabular surgery is to expose, reduce, and stabilize a particular injury pattern through a single, nonextensile approach (Matta, 1986). The two approaches most often used to accomplish that goal are the Kocher-Langenbeck for injuries involving the posterior structures, and the ilioinguinal for those involving the anterior structures (Letournel and Judet, 1993).
The goal of acetabular surgery is to expose, reduce, and stabilize a particular injury pattern through a single, nonextensile approach (Matta, 1986). The two approaches most often used to accomplish that goal are the Kocher-Langenbeck for injuries involving the posterior structures, and the ilioinguinal for those involving the anterior structures (Letournel and Judet, 1993).Indications
 The operative indications include loss of articular congruence, greater than 2 mm of displacement, a posterior wall fragment that involves more than 20% of the articular surface (controversial), and any fracture that involves the superior articular surface (Letournel and Judet, 1993; Matta, 1996; Tornetta, 2001). The focus of this chapter is the anterior incisions and their modifications.
The operative indications include loss of articular congruence, greater than 2 mm of displacement, a posterior wall fragment that involves more than 20% of the articular surface (controversial), and any fracture that involves the superior articular surface (Letournel and Judet, 1993; Matta, 1996; Tornetta, 2001). The focus of this chapter is the anterior incisions and their modifications. The indications for the ilioinguinal approach include patterns of fracture of the anterior wall or column, anterior column plus posterior hemitransverse fracture, and the associated both-column, and rarely the transverse, fracture.
The indications for the ilioinguinal approach include patterns of fracture of the anterior wall or column, anterior column plus posterior hemitransverse fracture, and the associated both-column, and rarely the transverse, fracture.• It can be utilized for some anterior wall fractures and rarely transverse fractures in which the major displacement is in the anterior column (Letournel, 1993; Matta, 1986). It can also be utilized to reduce the anterior column in a T-shaped fracture, when a staged or sequential approach is indicated.
 Other anterior approaches can be used to facilitate open reduction and internal fixation of acetabular fractures. These include the iliofemoral approach, the modified Stoppa approach, and modifications and extensions of the ilioinguinal approach.
Other anterior approaches can be used to facilitate open reduction and internal fixation of acetabular fractures. These include the iliofemoral approach, the modified Stoppa approach, and modifications and extensions of the ilioinguinal approach.• The indications for the iliofemoral approach include low anterior column fractures, anterior wall fractures, or when access to the hip joint is desired, such as with a femoral head fracture.
• The anterior Stoppa approach was originally described for hernia surgery (Stoppa, 1989; Stoppa et al., 1984). It has since been modified by Cole and Bolhofner (1994) for use with certain types of acetabular fractures. It allows improved access to the quadrilateral plate and posterior column, which may be required in certain patterns such as anterior column or wall, anterior plus posterior hemitransverse, transverse or T-shaped, and associated both-column fractures.
• In some cases the surgeon may need to have improved access to the anterior pelvis, such as for an anterior wall fracture or low anterior column fracture, and/or intra-articular access to the hip joint (femoral head fracture).
♦ In these instances, the iliofemoral approach may be combined with the ilioinguinal approach, with a distal vertical extension of the ilioinguinal approach (Kellam and Tile, 1995).
♦ Other options involve modification of the skin incision for the ilioinguinal approach (lower in the region of the anterior superior iliac spine [ASIS]), as described by Kloen et al. (2002).
Examination/Imaging
 A detailed clinical examination is completed to assess neurovascular status as well as the overall condition of the patient. The examination of the affected hip will be limited by pain, but it is important to rule out an associated dislocation. Clues to an anterior dislocation include shortening, external rotation, and slight abduction of the limb.
A detailed clinical examination is completed to assess neurovascular status as well as the overall condition of the patient. The examination of the affected hip will be limited by pain, but it is important to rule out an associated dislocation. Clues to an anterior dislocation include shortening, external rotation, and slight abduction of the limb. Radiographic evaluation starts with an anteroposterior (AP) radiograph followed by oblique views (Judet views) to visualize the anterior and posterior components of the acetabulum.
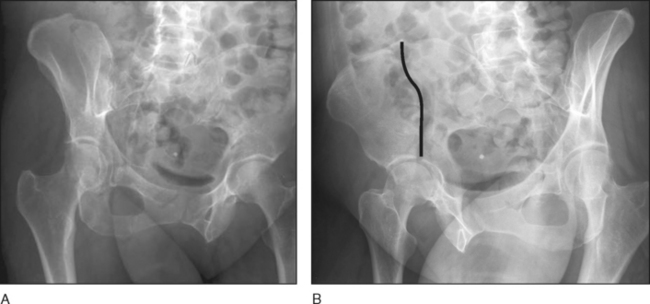
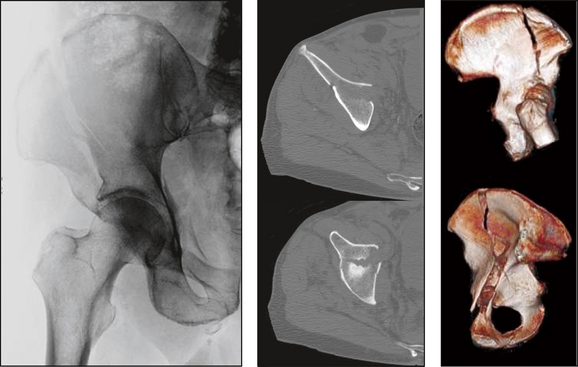
Radiographic evaluation starts with an anteroposterior (AP) radiograph followed by oblique views (Judet views) to visualize the anterior and posterior components of the acetabulum.• Figure 1 shows obturator (Fig. 1A) and iliac (Fig. 1B) oblique (Judet) views demonstrating a high anterior column fracture (fracture line drawn in black).
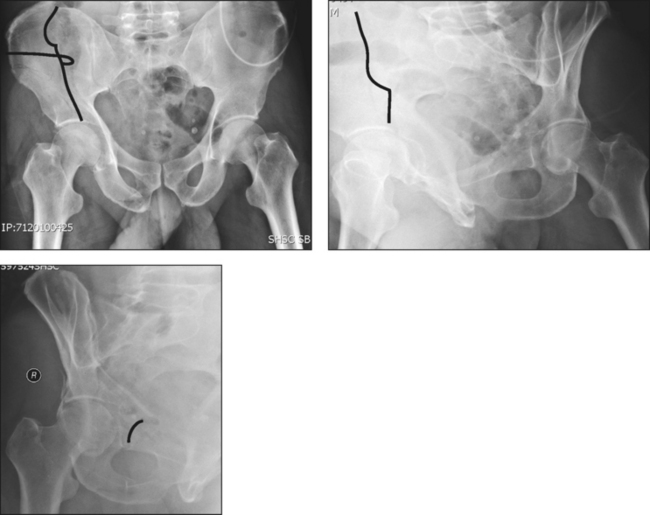
• In Figure 2, AP and oblique views show a low anterior column fracture (fracture line drawn in black) in a 49-year-old man who fell off a ladder.
 If the patient is hemodynamically stable, computed tomography (CT) scanning is completed to provide further information regarding the injury pattern, as for the high anterior column fracture seen in Figure 4.
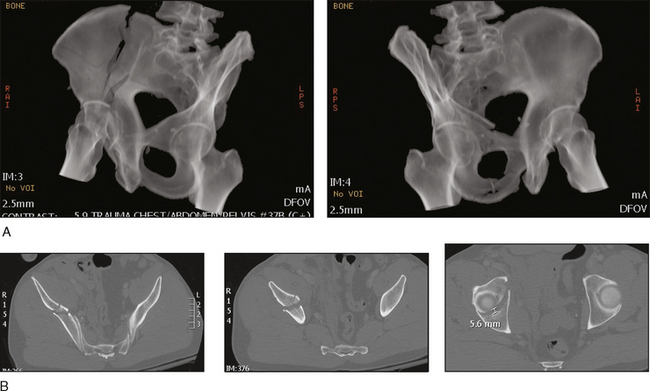
If the patient is hemodynamically stable, computed tomography (CT) scanning is completed to provide further information regarding the injury pattern, as for the high anterior column fracture seen in Figure 4.• In Case 1, volume-rendered oblique radiographic views (Fig. 5A) and axial CT scans (Fig. 5B) confirm anterior column involvement only.
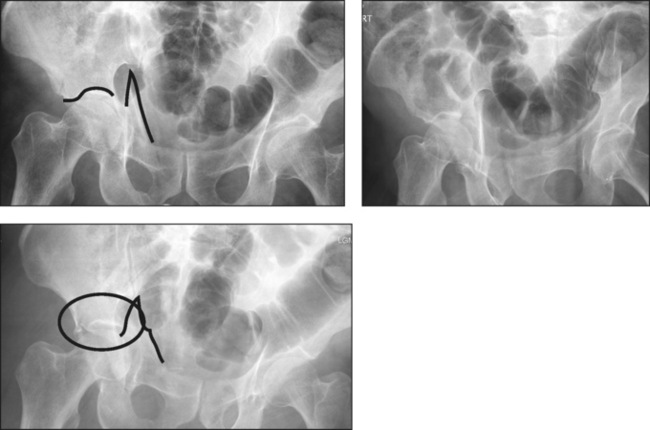
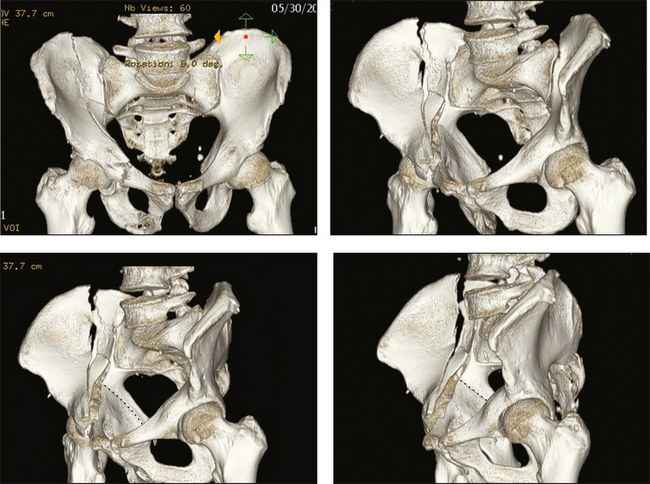
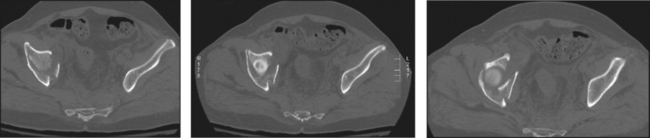
• In Case 2, three-dimensional CT provides information regarding anterior column displacement and comminution (Fig. 6; undisplaced fracture line into posterior column drawn in black). If this fracture were complete, the fracture pattern would likely have been designated an associated both-column fracture. Axial CT slices (Fig. 7) demonstrate involvement of the anterior wall and quadrilateral surface.
Surgical Anatomy
 Ilioinguinal approach
Ilioinguinal approach• Structures at risk include the lateral femoral cutaneous nerve of the thigh, which most frequently lies within 1 cm of the medial aspect of the ASIS; however, variations exist, including lateral to the ASIS. This nerve is usually found deep to the inguinal ligament, and is most often cut during dissection just medial to the ASIS.
• The approach involves development of three windows (see Portals/Exposures below). During dissection between the psoas muscle (together with the femoral nerve, which lies in the substance of the psoas) and the external iliac vessels, aggressive retraction can damage these structures. In addition to damage to these structures, there is often a perforating vessel through the iliopectineal fascia that must be ligated or cauterized.
• Deep to the external iliac vessels, in the retropubic area, are vessels known as the “corona mortis.” This is a retropubic anastomosis between the external and internal (via the obturator) iliac vessels and is variable in caliber and occurrence. Thus, care must be taken when dissecting in this area. One study noted retropubic anastomoses in 37% of their ilioinguinal approaches, with 43% of the dissections noted to have multiple vessels along the superior pubic ramus (Matta, 1986). Two cadaver studies noted arterial anastomoses in 34% and 43%, venous anastomoses in 70% and 59%, and combined arterial and venous in 20% and 27%, respectively. It was also found in these two studies that 84% and 79% of the cadavers had at least one vessel that was a minimum of 2 mm in diameter (Teague et al., 1996; Tornetta et al., 1996).
• As dissection is carried deep in this area along the quadrilateral surface and the posterior column, the obturator vessels and nerve are visualized and need to be protected. In the posterior aspect, the L5 nerve lies within 2–3 cm of the sacroiliac joint (De Ridder et al., 1999; Hospodar et al., 1999; Kim et al., 1999).
 Iliofemoral approach
Iliofemoral approach• The disadvantage of this approach is that entire access to the anterior column is limited medially, such that screws inserted into plates applied through this approach must be directed medially away from the iliopectineal eminence to avoid violation of the hip joint.
• Structures at risk are similar to those for the ilioinguinal approach, and include the lateral femoral cutaneous nerve of the thigh. Also, aggressive medial retraction of the psoas can damage the femoral nerve and/or the external iliac vessels; and posteriorly, the L5 nerve lies within 2–3 cm of the sacroiliac joint (De Ridder et al., 1999; Hospodar et al., 1999; Kim et al., 1999). With distal dissection in the upper thigh, further damage to the lateral cutaneous nerve of the thigh, as well as to the ascending branch of the lateral circumflex femoral artery, can occur.
 Modified Stoppa approach
Modified Stoppa approach• To facilitate access to the anterior column, the first (lateral) window of the ilioinguinal approach is utilized. Therefore, the external iliac vessels and the femoral and ilioinguinal nerves are at lower risk. However, the obturator vessels and nerve as well as the lumbosacral trunk are at increased risk.
 Modified ilioinguinal approaches
Modified ilioinguinal approaches• Structures at risk are similar to those with the ilioinguinal approach. In addition, with the addition of a distal vertical limb (rarely performed), the distal dissection places the lateral cutaneous nerve of the thigh and the ascending branch of the lateral circumflex femoral artery at risk for injury.
Positioning
 Ilioinguinal approach
Ilioinguinal approach• The patient is positioned supine with a bump under the buttock and shoulder on the operative side.
• The patient can be positioned on the fracture table or on a radiolucent table with the leg free.
♦ The benefit of the fracture table is that in most cases the femoral head can be repositioned under the acetabular dome, using longitudinal—with or without lateral—traction.
♦ The benefit of the radiolucent table is that the leg is prepped into the field, and is free, allowing more utilization of the lateral window by means of increased hip flexion.
 Modified Stoppa approach
Modified Stoppa approach• The patient is positioned supine on a radiolucent table, but the unaffected (nonoperative) side is usually bumped up. This relates to the fact the rationale of the approach is to provide increased visualization of the quadrilateral plate and posterior column.
Portals/Exposures
 Ilioinguinal approach
Ilioinguinal approach