Section 4. Returning to play
Introduction240
Functional performance tests242
Sport-specific agility drills248
Plyometric training251
Additional power training253
The “fitness test”255
Introduction
“When can I play again?” is the million dollar question that all athletes want answered if they have been injured. The pressure on clinicians to get players back to competition as quickly as possible can be intense especially in professional sport. This pressure can come not only from the players themselves, but also from the coaching and management team and parents (in the case of young athletes). Effective goal setting that includes clinical, functional performance and sport-specific testing should be done routinely. These should be agreed from the outset and this can help to avoid any mismatch of expectation by the clinician, the athlete and members of the coaching staff and family.
There are many factors that can affect the return to training and competition, and these are not just based on the physiological aspects of healing. Psychologically, players are often not ready to return to the field even after biological healing has taken place. Most athletes will undergo a so-called ‘fitness test’ to see if they are fit to play. However, it is not just about the fitness test; the player should have successfully completed all the rehabilitation milestones and undertaken full participation in team practice and possibly some reserve / warm up games where practical. There may be numerous personnel involved in the rehabilitation of an injured player and each club has a different set up and processes. What is important is that in  each club there is a defined protocol for return to play and it is well understood which personnel, usually the team doctor and / or physiotherapist, are responsible for the final decision that a player is fit to play. Adoption of a clear policy can help avoid any conflict during this process and help protect the player concerned. Coaching staff have been known to put pressure on a player to return to play before they are ready.
each club there is a defined protocol for return to play and it is well understood which personnel, usually the team doctor and / or physiotherapist, are responsible for the final decision that a player is fit to play. Adoption of a clear policy can help avoid any conflict during this process and help protect the player concerned. Coaching staff have been known to put pressure on a player to return to play before they are ready.
Return to play criteria should include each of the following components:
• Pathology specific
• Sport specific
• Position specific for the given sport
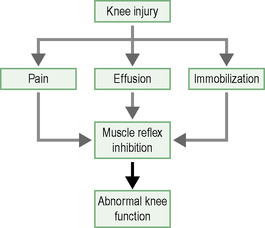
The late stage of rehabilitation assumes that the athlete has satisfactorily progressed through the early and middle stages of rehabilitation (see Section 3) and has no residual pain or swelling, 90% ROM and strength and good proprioception. These are the building blocks required in order to progress safely to higher demand functional performance tests, sports specific agility tests, power work and plyometric training. It is worth mentioning here that whilst athletes are continually re-assessed throughout the rehabilitation programme, in the late stage any swelling or pain induced by these activities will have an adverse effect on function and needs to be closely monitored (Fig 4.1). You don’t want an  athlete to get into a cycle of pain and swelling with activity. Athletes particularly prone to this are those who have sustained articular damage following a knee or ankle injury, e.g. ACL or talar dome injury.
athlete to get into a cycle of pain and swelling with activity. Athletes particularly prone to this are those who have sustained articular damage following a knee or ankle injury, e.g. ACL or talar dome injury.
Finally, it is worth remembering that certain injuries, e.g. hamstring injuries, and certain sports, such as rugby, have high recurrence rates of injury. Putting a player back too soon must increase their chances of re-injury. Well defined return to play criteria that are appropriate for the player’s injury, sport and position provide them and the clinician with the confidence that the player is ready to go back to full competition.
Functional performance tests
Generally, most sporting activity involves movement that requires a combination of both horizontal and vertical force production. Functional performance tests aim to simulate the forces encountered under sporting activity in a controlled environment. These tests have evolved because traditional outcome measures such as strength testing (this includes isokinetics) have only a weak to moderate relationship with functional tasks, i.e. performance. Also, strength and power has many manifestations and these can be quite specific and therefore should be tested within a functional context. Functional performance tests are highly suited for this purpose and should be incorporated into rehabilitation programmes as soon as it is safe to do so. They can be used as an objective outcome measure of progress from the middle stage right through to the end stage of the rehabilitation programme. In an ideal world athletes will have been screened for the tests that are relevant to their sport and therefore have baseline data for comparison following any injury. Functional performance tests are an indirect measure of all the following parameters:
Also, strength and power has many manifestations and these can be quite specific and therefore should be tested within a functional context. Functional performance tests are highly suited for this purpose and should be incorporated into rehabilitation programmes as soon as it is safe to do so. They can be used as an objective outcome measure of progress from the middle stage right through to the end stage of the rehabilitation programme. In an ideal world athletes will have been screened for the tests that are relevant to their sport and therefore have baseline data for comparison following any injury. Functional performance tests are an indirect measure of all the following parameters:
Joint mobility
Muscle flexibility
Muscle strength and power
Proprioception
Neuromuscular control
Dynamic balance
Agility
Pain
Athlete confidence
They can be especially useful at that difficult time when the athlete has been symptom-free for a while, has full ROM, is back to running and wants to short cut the last stage of the rehabilitation phase and go straight back to playing. These tests, alongside  sprint and agility drills, will often highlight the lack of full functional capacity and demonstrate to the athlete that, whilst they may feel good to go, there is still some work to do before they are ready.
sprint and agility drills, will often highlight the lack of full functional capacity and demonstrate to the athlete that, whilst they may feel good to go, there is still some work to do before they are ready.
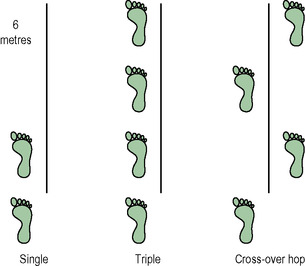
A battery of functional performance tests exist (Box 4.1), from a simple single leg-hop test to the more complex and demanding cross-over hop (Fig 4.2). These may be measured for height or distance or timed, depending on the test.
Box 4.1
| Single-leg hop | Vertical jump |
| Triple hop | Side jump |
| Stair / slope running | Shuttle runs |
| Figure of 8 drills | 6 m timed hop |
| Cross-over hop | Stair hop |
| Vertical-squat jump | Drop jump |
| Linear sprint |
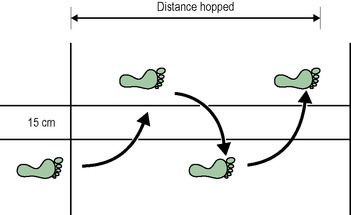
Hops for distance
These are very easy to perform. Place some tape on the floor. The athlete starts with their toes just behind the tape. The distance is measured from the front of the take-off toe to the front of the landing toe. For the cross-over hop two lines of tape are placed 15 cm apart (Fig 4.3).
 Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|