SECTION 4 Respiratory
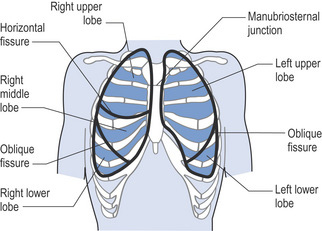
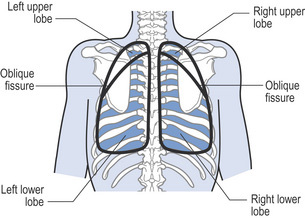
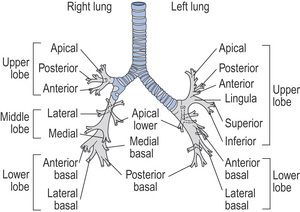
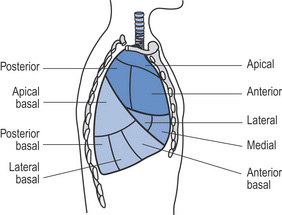
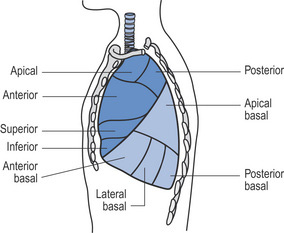
Respiratory anatomy illustrations
| Useful lung markings* | |
|---|---|
| Apex | Anterior – 2.5 cm above clavicles |
| Posterior – T1 | |
| Lower borders | Anterior – sixth rib |
| Posterior – T10/11 | |
| Mid-axilla – eighth rib | |
| Tracheal bifurcation | Anterior – manubriosternal junction |
| Posterior – T4 | |
| Right horizontal fissure | Anterior – fourth rib (above the nipple) |
| Oblique fissures | Anterior – sixth rib (below the nipple) |
| Posterior – T2/3 | |
| Left diaphragm | Anterior – sixth rib |
| Posterior – T10 | |
| Mid-axilla – eighth rib | |
| Right diaphragm | Anterior – fifth rib |
| Posterior – T9 | |
| Mid-axilla – eighth rib | |
* These lung markings are approximate and can vary between individuals.
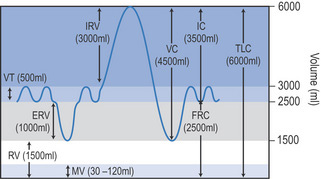
Respiratory volumes and capacities
Lung volumes
IRV (inspiratory reserve volume)
Maximum amount of air that can be inspired on top of a normal tidal inspiration
ERV (expiratory reserve volume)
Maximum amount of air that can be exhaled following a normal tidal expiration
Lung capacities
A capacity is the combination of two or more lung volumes
IC (inspiratory capacity)
The maximum volume of air that can be inspired after a normal tidal expiration

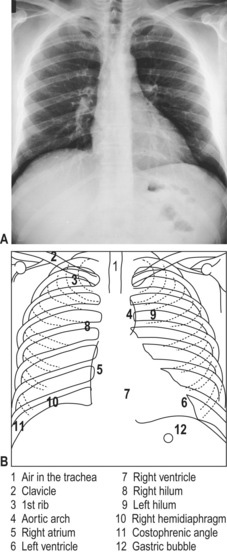
Chest X-rays
Analysing chest X-rays
Adopt a systematic approach when analysing X-rays (). You should check the following:
Is it anteroposterior (AP) or posteroanterior (PA)? Supine or erect?
Extrathoracic soft tissues
Trachea
Heart
Auscultation
Added sounds
Crackles
Voice sounds
In normal lung tissue, voice sounds are indistinct and unintelligible. When there is consolidation, sound is transmitted more clearly and loudly and speech can be distinguished. Voice sounds can be diminished in the presence of emphysema, pneumothorax and pleural effusion. They can be heard through a stethoscope (vocal resonance) or felt by hand (vocal fremitus).To test voice sounds patients can be asked to say or whisper ‘99’ repeatedly.
Interpreting blood gas values
| Arterial blood analysis | Reference ranges in adults |
|---|---|
| ph | 7.35−7.45 pH |
| PaO2 | 10.7–13.3 kPa (80–100 mmHg) |
| PaCO2 | 4.7–6.0 kPa (35–45 mmHg) |
| HCO3− | 22–26 mmol/L |
| Base excess | −2 to +2 |
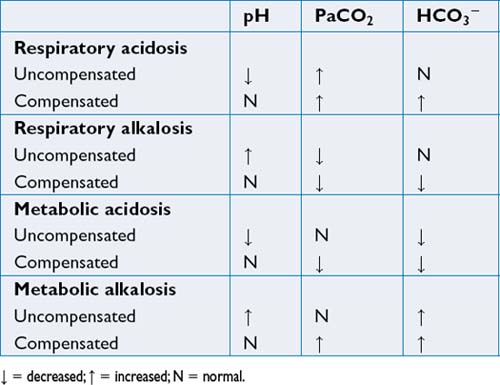
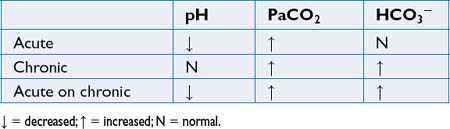
Assessing acid–base disorders
Assessing acid–base disorders involves examining the pH, PaCO2 and HCO3−:
Assessment
Nasal cannula
| To convert litres of O2 to FiO2 |
|---|
| RA≈ 21% FiO2 |
| 1 L/min ≈ 24% FiO2 |
| 2 L/min ≈ 28% FiO2 |
| 3 L/min ≈ 32% FiO2 |
| 4 L/min ≈ 36% FiO2 |
| 5 L/min ≈ 40% FiO2 |
| 6 L/min ≈ 44% FiO2 |
RA=room air.
> 6 L/min has little effect on FiO2 and may lead to irritation and drying of the nasal mucosa.
Sputum analysis (Middleton & Middleton 2008, with permission)
| Description | Causes | |
|---|---|---|
| Saliva | Clear watery fluid | |
| Mucoid | Opalescent or white | Chronic bronchitis without infection, asthma |
| Muco- purulent | Slightly discoloured, but not frank pus | Bronchiectasis, cystic fibrosis, pneumonia |
| Purulent | Thick, viscous: | Haemophilus Pseudomonas Pneumococcus, Mycoplasma Klebsiella |
| Frothy | Pink or white | Pulmonary oedema |
| Haemoptysis | Ranging from blood specks to frank blood, old blood (dark brown) | Infection (tuberculosis, bronchiectasis), infarction, carcinoma, vasculitis, trauma, also coagulation disorders, cardiac disease |
| Black | Black specks in mucoid secretions | Smoke inhalation (fires, tobacco, heroin), coal dust |
Modes of mechanical ventilation
Intermittent mandatory ventilation (IMV)
Delivers a preset number of breaths at a preset tidal volume and flow rate but allows the patient to take spontaneous breaths between machine-delivered breaths.
High-frequency ventilation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree