PROCEDURE 4 Proximal Humerus Fractures
Indications
 Prosthetic replacement of the proximal humerus for fractures is reserved for situations of poor bone stock and fracture patterns that will not allow stable internal fixation or will affect viability of the humeral head.
Prosthetic replacement of the proximal humerus for fractures is reserved for situations of poor bone stock and fracture patterns that will not allow stable internal fixation or will affect viability of the humeral head.• Note that isolated deltoid muscle paralysis is not considered a contraindication to arthroplasty for proximal humerus fractures—outcomes can be “of limited goals” but satisfactory.
• While preservation of the humeral head in 3-part fractures may be the preferred method of treatment, arthroplasty will have a more positive outcome in cases with:
• It has been recommended that a subset of patients with “valgus impacted 4-part fractures” be treated with open reduction and internal fixation.
 In these injuries, the humeral head is impacted upon the humeral shaft and, while the tuberosities are fractured, they are still in close approximation to the head and shaft.
In these injuries, the humeral head is impacted upon the humeral shaft and, while the tuberosities are fractured, they are still in close approximation to the head and shaft.
 Note that in these patients the head is not dislocated or displaced laterally and some contact with the glenoid is maintained.
Note that in these patients the head is not dislocated or displaced laterally and some contact with the glenoid is maintained.
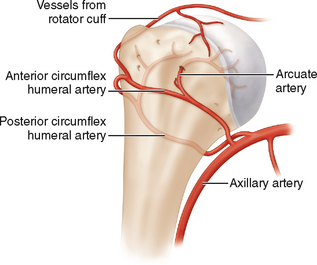
 If lateral displacement is found, then the medial periosteal vessels that perfuse the articular segment may be ruptured and avascular necrosis is more likely to result. Hence internal fixation would not be the treatment of choice.
If lateral displacement is found, then the medial periosteal vessels that perfuse the articular segment may be ruptured and avascular necrosis is more likely to result. Hence internal fixation would not be the treatment of choice.
 In these injuries, the humeral head is impacted upon the humeral shaft and, while the tuberosities are fractured, they are still in close approximation to the head and shaft.
In these injuries, the humeral head is impacted upon the humeral shaft and, while the tuberosities are fractured, they are still in close approximation to the head and shaft. Note that in these patients the head is not dislocated or displaced laterally and some contact with the glenoid is maintained.
Note that in these patients the head is not dislocated or displaced laterally and some contact with the glenoid is maintained. If lateral displacement is found, then the medial periosteal vessels that perfuse the articular segment may be ruptured and avascular necrosis is more likely to result. Hence internal fixation would not be the treatment of choice.
If lateral displacement is found, then the medial periosteal vessels that perfuse the articular segment may be ruptured and avascular necrosis is more likely to result. Hence internal fixation would not be the treatment of choice.Examination/Imaging
DETAILED HISTORY AND PHYSICAL
IMAGING STUDIES
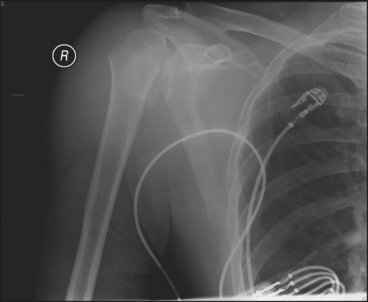
 Trauma series radiographs of the injured shoulder are obtained. These include:
Trauma series radiographs of the injured shoulder are obtained. These include:• True anteroposterior view of the scapula, 30–40° oblique to the coronal plane of the body (Fig. 1)
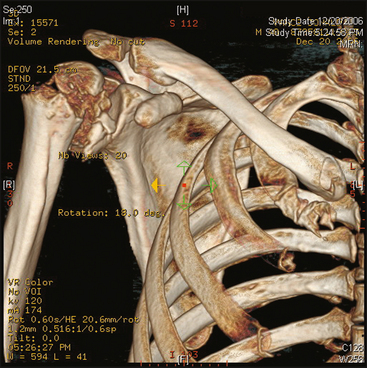
 Computed tomography is useful if the radiographs are not satisfactory for determining location of fracture lines, fracture displacement, or the quality of the articular surface. Figure 2 shows a three-dimensional reconstruction of the fracture shown in Figure 1.
Computed tomography is useful if the radiographs are not satisfactory for determining location of fracture lines, fracture displacement, or the quality of the articular surface. Figure 2 shows a three-dimensional reconstruction of the fracture shown in Figure 1. Note the importance of imaging of the contralateral shoulder. This is helpful in determining the appropriate length, which is important for prosthesis placement.
Note the importance of imaging of the contralateral shoulder. This is helpful in determining the appropriate length, which is important for prosthesis placement.Surgical Anatomy
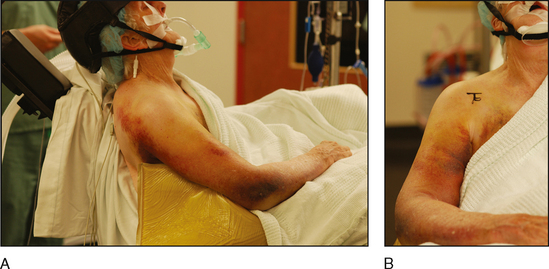
 The patient’s age or medical condition can affect the quality of the bone and the vascular supply to the humeral head (Fig. 3). In this setting internal fixation may become less attractive and prosthetic arthroplasty may be the preferred option.
The patient’s age or medical condition can affect the quality of the bone and the vascular supply to the humeral head (Fig. 3). In this setting internal fixation may become less attractive and prosthetic arthroplasty may be the preferred option.• The arcuate artery, a continuation of the ascending branch of the anterior humeral circumflex artery, enters the humerus at the area of the intertubercular groove, and its branches supply both the greater and the lesser tuberosities.
Positioning
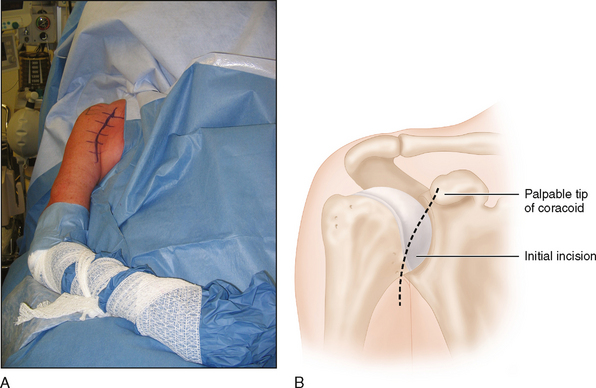
 Commonly a table in the modified beach chair position is used that has a cutaway section at the shoulder allowing for greater access to the affected shoulder posteriorly (Fig. 4A and 4B).
Commonly a table in the modified beach chair position is used that has a cutaway section at the shoulder allowing for greater access to the affected shoulder posteriorly (Fig. 4A and 4B). The area is appropriately prepped and draped from the midclavicle to below the axilla. The arm is draped free, allowing for full movement throughout the procedure.
The area is appropriately prepped and draped from the midclavicle to below the axilla. The arm is draped free, allowing for full movement throughout the procedure.Portals/Exposures
 All 2-part, most 3-part, and some 4-part acute proximal humerus fractures are well treated by closed reduction as well as by open reduction and internal fixation techniques.
All 2-part, most 3-part, and some 4-part acute proximal humerus fractures are well treated by closed reduction as well as by open reduction and internal fixation techniques.DISSECTION
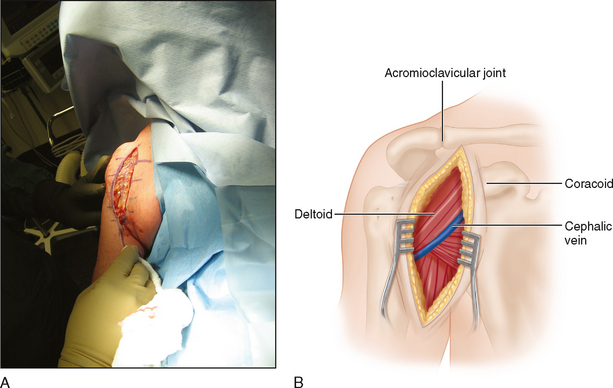
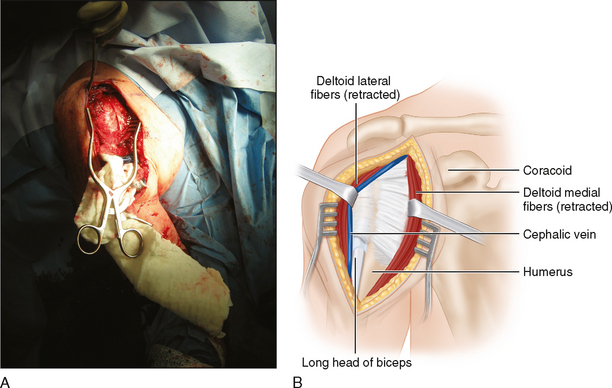
 The cephalic vein is immediately identified in the deltopectoral muscular interval (Fig. 6A and 6B).
The cephalic vein is immediately identified in the deltopectoral muscular interval (Fig. 6A and 6B). Identification of the coracoid and its originating muscles (conjoined tendon) will define the medial limits of dissection.
Identification of the coracoid and its originating muscles (conjoined tendon) will define the medial limits of dissection.• A broad retractor may be placed under the conjoined tendon and muscles in order to protect the medial neurovascular structures (Fig. 7A and 7B).
 The glenohumeral joint can be easily identified by finding the long head of the biceps distally and following it proximally back to the superior aspect of the glenoid.
The glenohumeral joint can be easily identified by finding the long head of the biceps distally and following it proximally back to the superior aspect of the glenoid.FRACTURE EXPOSURE
 Large bone fragments should be retained as they may be important in ultimately determining the appropriate prosthetic height.
Large bone fragments should be retained as they may be important in ultimately determining the appropriate prosthetic height. Identification of fracture fragments is usually dependent upon their position relative to the long head of the biceps.
Identification of fracture fragments is usually dependent upon their position relative to the long head of the biceps.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree