PROCEDURE 39 Compartment Syndrome
Introduction
 Compartment syndrome is caused by elevated intracompartmental pressure (ICP) leading to microvascular compromise. Without decompression of the compartment, ischemia and cell death occur.
Compartment syndrome is caused by elevated intracompartmental pressure (ICP) leading to microvascular compromise. Without decompression of the compartment, ischemia and cell death occur. The impact of increased compartment pressures and their sequelae have long been recognized, but the current understanding of acute compartment syndrome was developed in the 1970s. Acute compartment syndrome is considered to be the result of raised tissue pressure within a closed osseofascial compartment compromising microcirculatory perfusion.
The impact of increased compartment pressures and their sequelae have long been recognized, but the current understanding of acute compartment syndrome was developed in the 1970s. Acute compartment syndrome is considered to be the result of raised tissue pressure within a closed osseofascial compartment compromising microcirculatory perfusion. Surgical decompression of the affected compartment by fasciotomy was suggested over 100 years ago (Volkmann, 1881). The utility of fasciotomy as prophylaxis against the development of contractures was later demonstrated in experimental studies as well as clinical use (Rorabeck, 1984). To this day, fasciotomy remains the only established treatment for managing an acute compartment syndrome.
Surgical decompression of the affected compartment by fasciotomy was suggested over 100 years ago (Volkmann, 1881). The utility of fasciotomy as prophylaxis against the development of contractures was later demonstrated in experimental studies as well as clinical use (Rorabeck, 1984). To this day, fasciotomy remains the only established treatment for managing an acute compartment syndrome.PATHOPHYSIOLOGY OF ACUTE COMPARTMENT SYNDROME
 Compartment syndromes occur when the tissue pressure within an enclosed space exceeds the capillary perfusion pressure, leading to microvascular compromise and ischemia. As ICP rises, there is a disruption of microvascular perfusion, reducing oxygen and nutrient delivery to a point where perfusion no longer meets the tissue demand.
Compartment syndromes occur when the tissue pressure within an enclosed space exceeds the capillary perfusion pressure, leading to microvascular compromise and ischemia. As ICP rises, there is a disruption of microvascular perfusion, reducing oxygen and nutrient delivery to a point where perfusion no longer meets the tissue demand. Three major theories attempt to explain the pathophysiology of microvascular dysfunction and ischemia:
Three major theories attempt to explain the pathophysiology of microvascular dysfunction and ischemia:• The critical closing pressure theory suggests there is a critical pressure at which active closure of small arterioles will occur as the transmural pressure (the difference between intravascular pressure and tissue pressure) drops.
• The microvascular occlusion theory proposes the existence of an absolute compartment pressure that results in compartment syndrome. Since normal capillary pressure at rest is approximately 25 mm Hg, an increase in tissue pressure to a similar level is thought to reduce capillary blood flow, leading to ischemia and eventual muscle necrosis.
 The high metabolic demand of skeletal muscle makes it the most vulnerable tissue in a limb affected by acute compartment syndrome. Both the magnitude and duration of increased compartment pressure have major effects on muscle viability. The reduced local blood flow to skeletal muscle causes ischemia and eventually leads to cell death.
The high metabolic demand of skeletal muscle makes it the most vulnerable tissue in a limb affected by acute compartment syndrome. Both the magnitude and duration of increased compartment pressure have major effects on muscle viability. The reduced local blood flow to skeletal muscle causes ischemia and eventually leads to cell death. Although ischemia is the predominant mechanism in the development of compartment syndrome, other factors are also important.
Although ischemia is the predominant mechanism in the development of compartment syndrome, other factors are also important.• Recent evidence suggests that most compartment syndromes are the result of a “low-flow” ischemic mechanism, in contrast to complete ischemia. Since the tissue pressure does not exceed the systolic blood pressure, there is the potential for some continued perfusion in the affected compartment. This phenomenon is analogous to a reperfusion injury following complete ischemia, and includes the release of reactive oxygen metabolites as well as pronounced neutrophil activation (Lawendy et al., 2007; Sadasivan et al., 1997).
• Neutrophil activation further contributes to microvascular dysfunction and blood flow abnormalities in acute compartment syndrome.
• Evidence suggests that both inflammation and ischemia cause cellular injury in acute compartment syndrome. Prolonged pressure elevation exacerbates microcirculatory impairment, increases reperfusion injury, and markedly depletes intramuscular high-energy phosphates, with resultant irreversible ultrastructural tissue damage.
Indications
 Indications for surgical treatment of compartment syndrome include the presence of compartment syndrome, or an impending compartment syndrome.
Indications for surgical treatment of compartment syndrome include the presence of compartment syndrome, or an impending compartment syndrome.• Because of the severe adverse consequences of a missed compartment syndrome, most orthopedic surgeons recommend an inclusive approach to surgical treatment. Any patient with signs of, or significant risk factors for, compartment syndrome should be considered for fasciotomy independent of anatomic location.
Examination/Imaging
 Early diagnosis of acute compartment syndrome is critical to its successful management and subsequent clinical outcome. Failure of timely diagnosis is the single most important cause of adverse outcomes (Matsen et al., 1980; McQueen et al., 1996).
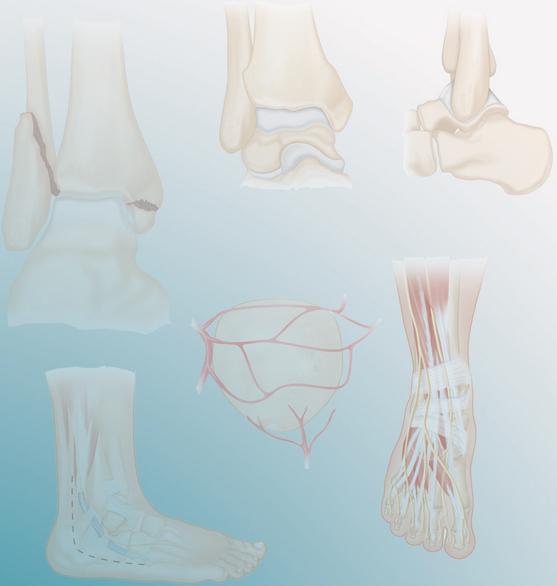
Early diagnosis of acute compartment syndrome is critical to its successful management and subsequent clinical outcome. Failure of timely diagnosis is the single most important cause of adverse outcomes (Matsen et al., 1980; McQueen et al., 1996). Early diagnosis of compartment syndrome is facilitated by recognition of patient risk factors, understanding of the early clinical symptoms of compartment syndrome, and the judicious use of compartment pressure monitoring (McQueen et al., 1996). Risk factors for the development of acute compartment syndrome include male gender, youth, tibial fracture, high-energy forearm fracture, high-energy femoral diaphyseal fracture, and bleeding diathesis or anticoagulation.
Early diagnosis of compartment syndrome is facilitated by recognition of patient risk factors, understanding of the early clinical symptoms of compartment syndrome, and the judicious use of compartment pressure monitoring (McQueen et al., 1996). Risk factors for the development of acute compartment syndrome include male gender, youth, tibial fracture, high-energy forearm fracture, high-energy femoral diaphyseal fracture, and bleeding diathesis or anticoagulation. Missed or late diagnosis of acute compartment syndrome can result in serious complications such as muscle infarction, muscle contracture, secondary deformity, weakness, and neurologic dysfunction (Matsen et al., 1980). Other less common sequelae include infection, gram-negative sepsis, amputation, and end-organ involvement.
Missed or late diagnosis of acute compartment syndrome can result in serious complications such as muscle infarction, muscle contracture, secondary deformity, weakness, and neurologic dysfunction (Matsen et al., 1980). Other less common sequelae include infection, gram-negative sepsis, amputation, and end-organ involvement.• Time from onset to necrosis is variable, with an accepted upper limit of 6 hours. Determination of the exact time of onset of acute compartment syndrome is often difficult, as it may not parallel the onset of injury. Thus, ongoing assessment of the patient at risk is important in identifying a potential delayed-onset acute compartment syndrome.
• Missed or late diagnosis is often a result of clinical inexperience, lack of suspicion, or a confusing clinical presentation. Altered pain perception, as seen with changes in level of consciousness, regional anesthesia, patient-controlled analgesia, and nerve injury, are all risk factors for late diagnosis. Maintaining an appropriate index of suspicion is important in preventing the negative sequelae of late-diagnosed acute compartment syndrome as well as malpractice litigation.
CLINICAL DIAGNOSIS
 Disproportionate pain relative to the injury and pain on passive muscle stretch (PPS) are recognized as the first symptoms of acute compartment syndrome. Progressively increasing analgesia requirements may be a sign of disproportionate pain and an underlying compartment syndrome.
Disproportionate pain relative to the injury and pain on passive muscle stretch (PPS) are recognized as the first symptoms of acute compartment syndrome. Progressively increasing analgesia requirements may be a sign of disproportionate pain and an underlying compartment syndrome.• Pain that is produced upon plantar flexion of the foot or toes in an individual with an anterior acute compartment syndrome of the leg is an example of PPS. Both pain out of proportion to injury and PPS are the most sensitive clinical findings (19%) and are often the only findings that precede ischemic dysfunction in the nerves and muscles of the affected compartment. While the specificity of both pain measures is high (97%), the sensitivity is disturbingly poor (19%).
• Pain as a diagnostic criterion fails to identify a high percentage of individuals with acute compartment syndrome (Ulmer, 2002). The low false-positive rate suggests that the absence of pain is a more useful measure in ruling out acute compartment syndrome. However, an adequate level of suspicion must be maintained as the absence of pain may indicate individual variation, altered states of pain perception, compartment syndrome of the deep posterior compartment, or missed acute compartment syndrome that has resulted in altered sensation.
 Sensory changes are first noted approximately 1 hour after the onset of ischemia.
Sensory changes are first noted approximately 1 hour after the onset of ischemia.• Hypesthesias and paresthesias in the dermatomal distribution of the nerve(s) of the involved compartment are typically the first neurologic signs of acute compartment syndrome. As a clinical measure of acute compartment syndrome, paresthesia has a sensitivity of 13% and a specificity of 98% (Ulmer, 2002). Hypesthesias and paresthesias of the first web space indicate involvement of the deep peroneal nerve and anterior compartment syndrome, while numbness of the dorsum of the foot may indicate lateral compartment syndrome with compression of the superficial peroneal nerve. These signs may also be caused by direct trauma to the nerve.
 A swollen, tense compartment resulting from increased ICP is recognized as an early physical sign of acute compartment syndrome. These measures may not be evident with isolated involvement of a deep compartment. Dressings and casts should be removed to accurately assess swelling. The lack of a pulse is not a feature of acute compartment syndrome, and the presence of a pulse does not exclude it.
A swollen, tense compartment resulting from increased ICP is recognized as an early physical sign of acute compartment syndrome. These measures may not be evident with isolated involvement of a deep compartment. Dressings and casts should be removed to accurately assess swelling. The lack of a pulse is not a feature of acute compartment syndrome, and the presence of a pulse does not exclude it. Diagnosis of acute compartment syndrome requires careful evaluation of the entire clinical presentation. Ulmer (2002) found that the probability of acute compartment syndrome rose from approximately 25% when either pain, PPS, paresthesia, or paresis was present to 93% when three of these clinical findings were present concurrently. As noted, individual symptoms and signs are far from perfect in the diagnosis of compartment syndrome, but require careful interpretation owing to the tragic sequelae of a misdiagnosis.
Diagnosis of acute compartment syndrome requires careful evaluation of the entire clinical presentation. Ulmer (2002) found that the probability of acute compartment syndrome rose from approximately 25% when either pain, PPS, paresthesia, or paresis was present to 93% when three of these clinical findings were present concurrently. As noted, individual symptoms and signs are far from perfect in the diagnosis of compartment syndrome, but require careful interpretation owing to the tragic sequelae of a misdiagnosis.COMPARTMENT PRESSURE MONITORING
• The role of ICP measurement in acute compartment syndrome remains controversial. The comparative benefit of ICP measurements relative to clinical assessment is unclear. Further, definition of an ICP measurement that determines the need for fasciotomy is similarly unclear.
• Fasciotomy of the involved compartments remains the “gold standard” for treatment of compartment syndrome.
• Nonoperative measures have a limited role. There is little dispute regarding the severe consequences of delaying fasciotomy once the diagnosis of compartment syndrome has been made. Medical management at this time is restricted to an adjunctive role supplemental to fasciotomy.
 The therapeutic effects of mannitol have been investigated in animal studies. Case studies have reported success at averting fasciotomy in the context of clinically diagnosed compartment syndrome.
The therapeutic effects of mannitol have been investigated in animal studies. Case studies have reported success at averting fasciotomy in the context of clinically diagnosed compartment syndrome.
 Hyperbaric oxygen is thought to reduce edema within the affected compartment by oxygen-induced vasoconstriction while maintaining oxygen perfusion at lower perfusion pressure. Although this may be an effective adjunct to fasciotomy, it has limited availability. A recent review of the literature found that hyperbaric oxygen is effective in improving wound healing, reducing amputation rate, and lowering surgical procedure rate.
Hyperbaric oxygen is thought to reduce edema within the affected compartment by oxygen-induced vasoconstriction while maintaining oxygen perfusion at lower perfusion pressure. Although this may be an effective adjunct to fasciotomy, it has limited availability. A recent review of the literature found that hyperbaric oxygen is effective in improving wound healing, reducing amputation rate, and lowering surgical procedure rate.
 The therapeutic effects of mannitol have been investigated in animal studies. Case studies have reported success at averting fasciotomy in the context of clinically diagnosed compartment syndrome.
The therapeutic effects of mannitol have been investigated in animal studies. Case studies have reported success at averting fasciotomy in the context of clinically diagnosed compartment syndrome. Hyperbaric oxygen is thought to reduce edema within the affected compartment by oxygen-induced vasoconstriction while maintaining oxygen perfusion at lower perfusion pressure. Although this may be an effective adjunct to fasciotomy, it has limited availability. A recent review of the literature found that hyperbaric oxygen is effective in improving wound healing, reducing amputation rate, and lowering surgical procedure rate.
Hyperbaric oxygen is thought to reduce edema within the affected compartment by oxygen-induced vasoconstriction while maintaining oxygen perfusion at lower perfusion pressure. Although this may be an effective adjunct to fasciotomy, it has limited availability. A recent review of the literature found that hyperbaric oxygen is effective in improving wound healing, reducing amputation rate, and lowering surgical procedure rate. Measurement of ICP is a valuable tool for providing objective criteria for the diagnosis of acute compartment syndrome.
Measurement of ICP is a valuable tool for providing objective criteria for the diagnosis of acute compartment syndrome. To ensure accurate ICP measurements, proper technique is crucial. ICP measurements should be taken at the level of the fracture as well as at sites up to 5 cm proximal and distal to the injury, to capture the peak ICP value (Heckman et al., 1994). Pressures should also be measured in the other compartments of the affected limb to ensure that a compartment syndrome is not missed.
To ensure accurate ICP measurements, proper technique is crucial. ICP measurements should be taken at the level of the fracture as well as at sites up to 5 cm proximal and distal to the injury, to capture the peak ICP value (Heckman et al., 1994). Pressures should also be measured in the other compartments of the affected limb to ensure that a compartment syndrome is not missed. Techniques for measuring ICP include needle manometer, wick catheter, slit catheter, and electronic transducer–tipped catheters.
Techniques for measuring ICP include needle manometer, wick catheter, slit catheter, and electronic transducer–tipped catheters.• The needle manometer consists of a 20-ml syringe full of air that is attached to a column that contains both air and saline. The ICP is the pressure required to flatten the meniscus between the saline and the air. While this technique is simple and low cost, it is the least reliable as the needle can easily be occluded.
• The wick catheter is an adaptation of the needle manometer in which fibers project from the end of the catheter. The fibers prevent tissue plugging, thus maintaining patency of the catheter to improve accuracy.
• The slit catheter is another modification of the needle manometer technique that relies on the principle of increased surface area and increased patency. The tip of the catheter is cut longitudinally, forming plastic petals. A fluid column connected to a transducer measures pressure. Advantages of the slit catheter include prolonged use due to the open design of the catheter tip and the ability to break up blood clots in vivo by the application of pressure over the catheter tip. Accuracy is similar to the wick catheter.
• Transducer-tipped catheters, designed with the transducer housed in the catheter tip, have improved the accuracy of compartment pressure measurements. These include the the solid-state transducer intracompartmental catheter, an infusion-based system, and the electronic transducer-tipped system. Electronic techniques are independent of limb position and the height of the pressure transducer and do not require calibration. Disadvantages of these devices are cost and difficulty with resterilization.