PROCEDURE 38 Repair of Tarsometatarsal Joint (Lisfranc) Fracture-Dislocation
Indications
 The treatment goals for tarsometatarsal (TMT) joint injuries are to obtain proper joint alignment and congruity and maintain joint stability.
The treatment goals for tarsometatarsal (TMT) joint injuries are to obtain proper joint alignment and congruity and maintain joint stability. Nonoperative treatment is preferred for patients with TMT joint sprains.
Nonoperative treatment is preferred for patients with TMT joint sprains.• These are defined as pain on weight bearing and palpation without any radiographic instability, and nondisplaced ligamentous injuries.
• The indications for nonoperative treatment include less than 2 mm of displacement in any plane and no joint line instability with weight-bearing or stress radiographs.
• These injuries can be treated in a short-leg non–weight-bearing cast for 6 weeks with repeat stress views 10 days postinjury.
Examination/Imaging
PHYSICAL EXAMINATION
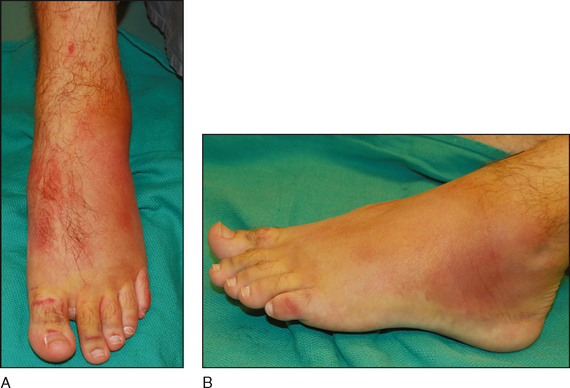
 Pain, swelling, or echymosis over any area of the TMT joint complex is usually present (Fig. 1A and 1B).
Pain, swelling, or echymosis over any area of the TMT joint complex is usually present (Fig. 1A and 1B). Pain with passive dorsiflexion or plantar flexion of individual metatarsal (MT) heads or pain in the midfoot with attempted single-leg heel rise can point to a Lisfranc injury.
Pain with passive dorsiflexion or plantar flexion of individual metatarsal (MT) heads or pain in the midfoot with attempted single-leg heel rise can point to a Lisfranc injury.IMAGING STUDIES
 Radiographic investigations include plain radiographs, stress radiographs, and computed tomography scans.
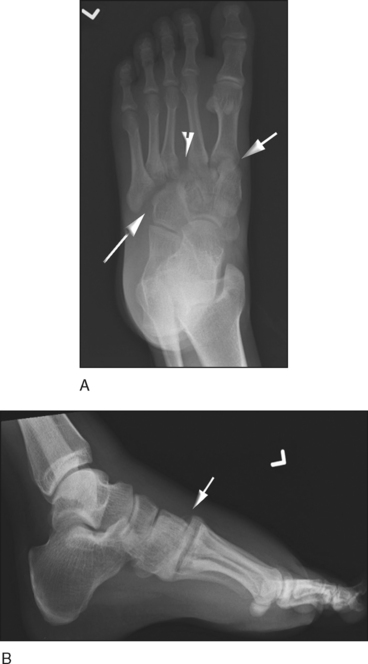
Radiographic investigations include plain radiographs, stress radiographs, and computed tomography scans. On plain radiographs, the following relationships should be maintained in the normal foot:
On plain radiographs, the following relationships should be maintained in the normal foot:• Lateral (Fig. 2B)
♦ The second TMT joint aligns on its dorsal surface uninterrupted with the tarsal bone proximally and the MT base distally.
 Any disturbance of the normal alignment on any one radiographic investigation may indicate a Lisfranc injury.
Any disturbance of the normal alignment on any one radiographic investigation may indicate a Lisfranc injury.• Avulsion fractures around the TMT joint—the “fleck” sign: an avulsion of the medial base of the second MT from the attachment of the Lisfranc ligament, as seen in Case 1 (Fig. 3A and 3B)
 Stress views can be performed to further assess the stability of the TMT complex. This can be done with the hindfoot stabilized and forefoot placed in supination/pronation or adduction/abduction.
Stress views can be performed to further assess the stability of the TMT complex. This can be done with the hindfoot stabilized and forefoot placed in supination/pronation or adduction/abduction.• Displacement greater than 2 mm of widening between the bases of the first and second MTs is considered ligamentous compromise.
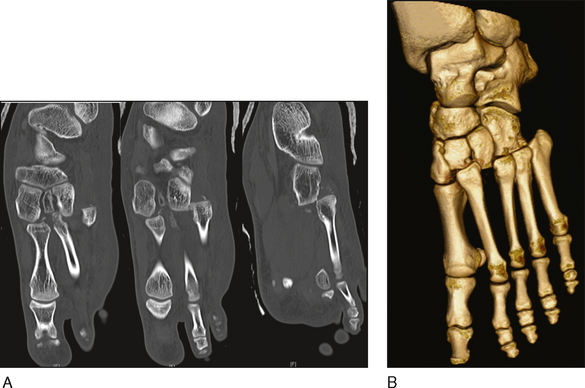
 Computed tomography—both standard (Fig. 5A) and three-dimensional (Fig. 5B), as for Case 1—can also be used to better evaluate subtle Lisfranc injuries or for preoperative assessment of other concurrent fractures.
Computed tomography—both standard (Fig. 5A) and three-dimensional (Fig. 5B), as for Case 1—can also be used to better evaluate subtle Lisfranc injuries or for preoperative assessment of other concurrent fractures.Surgical Anatomy
 The TMT joint is complex and is divided into the medial and lateral columns (Fig. 6).
The TMT joint is complex and is divided into the medial and lateral columns (Fig. 6).• The medial column is further divided into the medial and middle legs.
♦ The medial leg includes the first MT and medial cuneiform. This leg has three times more motion than the middle leg.
 The stability of the transmetatarsal arch is derived from the Roman arch keystone effect at the base of the second MT.
The stability of the transmetatarsal arch is derived from the Roman arch keystone effect at the base of the second MT. Additional stability of the TMT joint complex is provided by the dorsal and plantar interosseous capsuloligamentous restraints (Fig. 7A and 7B).
Additional stability of the TMT joint complex is provided by the dorsal and plantar interosseous capsuloligamentous restraints (Fig. 7A and 7B). The bases of the second through fifth MTs are bound by dense transverse metatarsal interosseous ligaments, with the dorsal ligaments weaker than the plantar ones.
The bases of the second through fifth MTs are bound by dense transverse metatarsal interosseous ligaments, with the dorsal ligaments weaker than the plantar ones. The base of the second MT is joined to the first TMT joint by a medial interosseous ligament connecting the medial plantar aspect of the second MT base to the plantar lateral medial cuneiform.
The base of the second MT is joined to the first TMT joint by a medial interosseous ligament connecting the medial plantar aspect of the second MT base to the plantar lateral medial cuneiform.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree