PROCEDURE 37 Calcaneus Fractures
Indications
 Significant change of shape or morphologic shift in calcaneal structure such that footwear would be problematic
Significant change of shape or morphologic shift in calcaneal structure such that footwear would be problematic• Nonoperative treatment is advised for older patients, and for patients with less injury or nondisplaced intra-articular fractures. If Böhler’s angle is greater than 15°, the patient will do relatively well regardless of operative or nonoperative treatment if the joint is not displaced.
• Nonoperative care is also advised in the medically unwell, such as patients with diabetes or peripheral vascular disease, and for smokers unwilling to stop smoking.
• Operative techniques are generally performed with a full open technique. Percutaneous techniques may be used for those cases with large calcaneal fragments or in the marginal medical patient where a full open reduction may result in skin or wound complications.
• Results of operative treatment for displaced intra-articular calcaneal fractures have shown improvement over nonoperative care in certain groups of patients, especially those who are young, female, have simple fractures, and have fractures that have very accurate reductions. Those patients in whom operative treatment has been shown to not make a difference include older patients, worker’s compensation patients, or those in whom Böhler’s angle is near normal.
Examination/Imaging
 Physical examination
Physical examination• Calcaneal fractures involve a severe amount of soft tissue injury with the impaction of the heel to a hard surface upon which it has landed. The soft tissue injury that results from the impact is often as bad as, or worse than, the calcaneal fracture beneath the skin.
• Careful observation for open wounds—especially medially beneath the sustentaculum tali and posteriorly around the Achilles tendon insertion—is mandatory.
♦ Appearance of soft tissue blisters will often occur over the initial 24 hours. These may be serous or hemorrhagic. The fracture can produce significant soft tissue tenting.
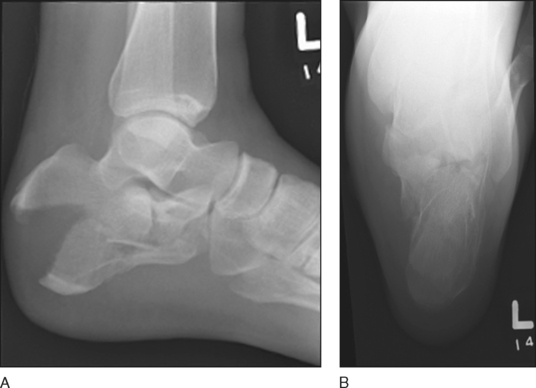
 Plain radiographs: lateral of the foot and Harris axial view
Plain radiographs: lateral of the foot and Harris axial view• The lateral radiograph (Fig. 1A) identifies the significance of impaction (Böhler’s angle loss). The normal Böhler’s angle is between 25° and 40°. Any loss of Böhlers angle to less than 15° is a significant injury, as those patients with a Böhlers angle that is greater than 15° can often be treated nonoperatively if there is not an associated significant articular surface disruption.
• The Harris axial view (if taken well) may show the articular surface, the primary fracture line, or the number of pieces of the posterior facet (Fig. 1B). It will also demonstrate the size of the “constant” piece that is used to act as a solid piece of bone for later reconstruction of the rest of the calcaneus.
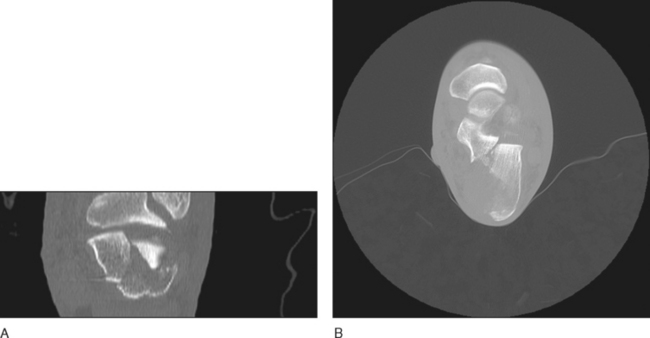
 Computerized tomography
Computerized tomography• Obtaining 2-mm axial (Fig. 2A) and coronal (Fig. 2B) cuts of both the normal and injured foot is advised.
Surgical Anatomy
• The soft tissue approach is not acceptable while there is marked swelling in the 3- to 10-day period of time immediately after the injury. It is much better in the period after this (10–17 days), but late surgery (after 21 days) is also not advised because of fracture healing.
• The soft tissue flap must be treated with utmost care for both surgical approach and closure to prevent infection and wound breakdown.
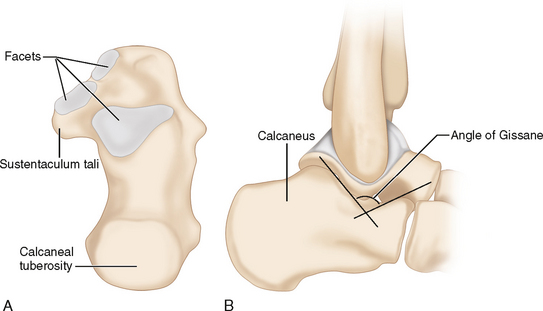
 Bony anatomy (Fig. 3A)
Bony anatomy (Fig. 3A)• The posterior facet is the largest of the three facets with a very small middle and anterior facet medially on top of the sustentaculum tali.
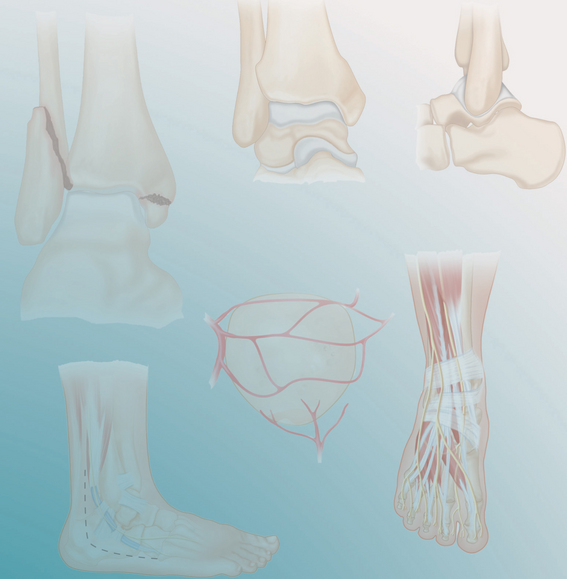
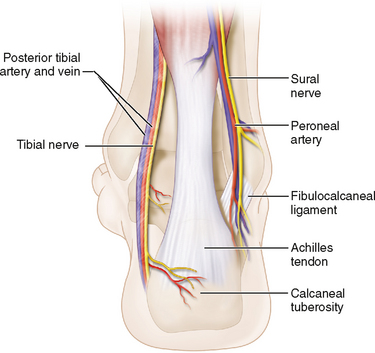
 Neurovascular anatomy (Fig. 4)
Neurovascular anatomy (Fig. 4)• There is no internervous intermuscular plane, but it is thought that there is a watershed area between the vascular supply involving the peroneal artery laterally and superiorly and the posterior tibial artery (from the heel pad).
 Musculotendinous anatomy (see Fig. 4)
Musculotendinous anatomy (see Fig. 4)• The insertion of the Achilles tendon on the calcaneal tuberosity is the strongest tendinous structure of the hindfoot.
Positioning
• Extra equipment such as laminar spreaders, Schanz pins, fluoroscopy, reduction clamps, and bone graft substitute are often useful.
 Lateral positioning of the patient is advised, with careful padding of all bony prominences. The upright foot should be somewhat posterior for easy access.
Lateral positioning of the patient is advised, with careful padding of all bony prominences. The upright foot should be somewhat posterior for easy access.Portals/Exposures
 The skin incision is an extended L approach based upon a full-thickness flap that relies upon subperiosteal dissection.
The skin incision is an extended L approach based upon a full-thickness flap that relies upon subperiosteal dissection.• It is usually initiated midway between the fibula and the Achilles tendon (Fig. 5), extending down to the lateral aspect of the distal calcaneus, where there is a change in skin texture (the glabrous/nonglabrous border).
• It is then extended distally to the base of the fifth metatarsal. A full-thickness flap is developed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree