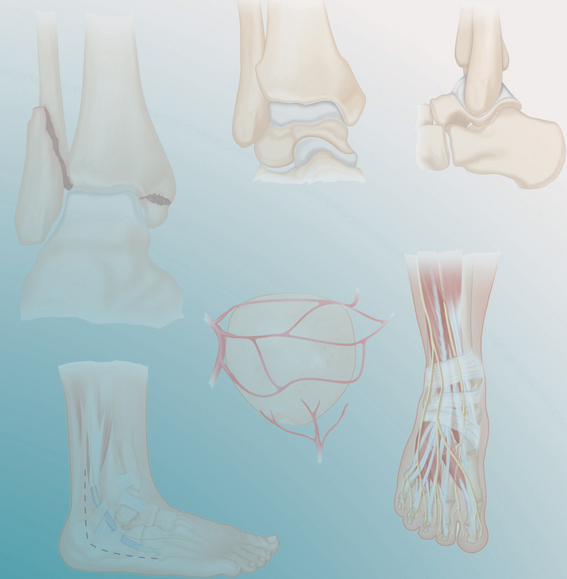
PROCEDURE 30 Proximal Tibia Fractures: External Fixation II
Indications
 Fractures involving both the medial and lateral columns of the proximal tibia (Schatzker types 5 and 6)
Fractures involving both the medial and lateral columns of the proximal tibia (Schatzker types 5 and 6) When the condition of the soft tissues prohibits the use of standard open reduction and internal fixation (ORIF) techniques
When the condition of the soft tissues prohibits the use of standard open reduction and internal fixation (ORIF) techniques• The use of circular external fixation (CEF) for fractures of the proximal tibia is challenging and requires training in the use of these devices. Unless the principles of articular fracture management are carefully followed, use of the device, in and of itself, will not result in a good outcome.
• The term circular external fixation in this procedure is being used for both standard Ilizarov circular external fixation and hybrid circular external fixation.
• It is suggested that this technique be undertaken by an individual who is trained in the application and management of CEF. While the procedure is theoretically straightforward, there are many subtleties that, in the absence of hands-on training, are difficult to describe in text. This procedure does not describe the specific details of frame application; however, it does discuss the general steps; the procedure as written relies on substantial knowledge of the use of these devices on the part of the reader.
Examination/Imaging
 Physical examination should include particular attention to the soft tissues. There should be wrinkling of the skin, and fracture blisters should be nonbloody and out of the surgical zones. The neurologic and vascular status should be carefully documented.
Physical examination should include particular attention to the soft tissues. There should be wrinkling of the skin, and fracture blisters should be nonbloody and out of the surgical zones. The neurologic and vascular status should be carefully documented. If suspicion of deep venous thrombosis exists, appropriate evaluations and treatment should be undertaken.
If suspicion of deep venous thrombosis exists, appropriate evaluations and treatment should be undertaken. Plain radiographs of the knee and tibia are obtained to
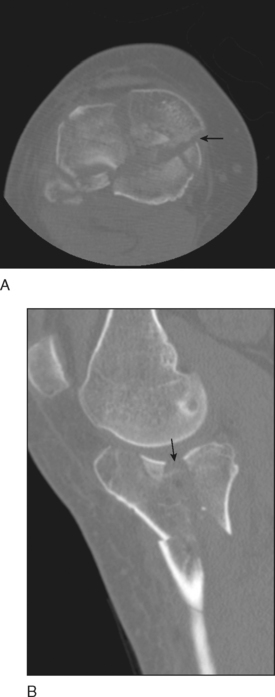
Plain radiographs of the knee and tibia are obtained to• Look for depression of the lateral tibial platueau on both the AP (Fig. 1A) and lateral (Fig. 1B) projections.
 A computed tomography (CT) scan provides useful information in cases of articular fractures. The images should include standard axial images as well as coronal and sagittal reconstructed images.
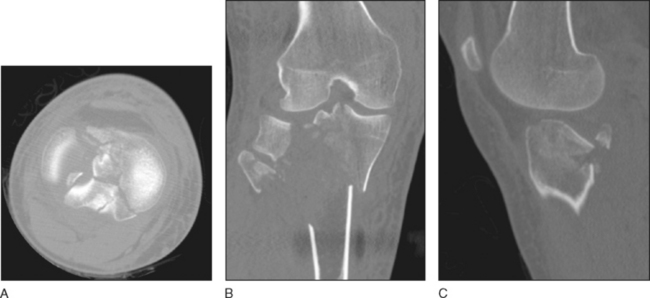
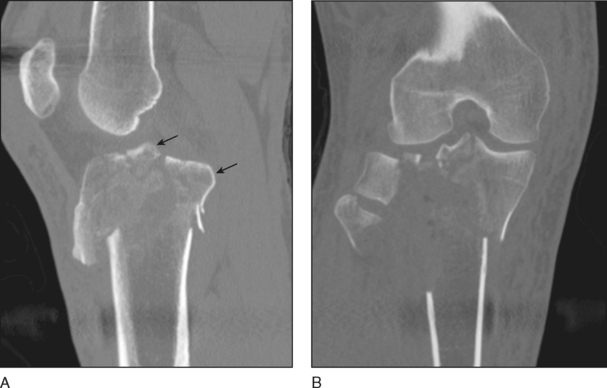
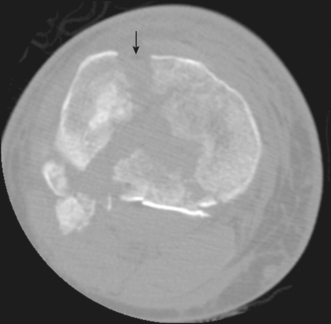
A computed tomography (CT) scan provides useful information in cases of articular fractures. The images should include standard axial images as well as coronal and sagittal reconstructed images.• CT images provide a more complete understanding of the articular injury, including coronal fractures of the medial plateau (Fig. 2A and 2B), the location and extent of depression/splitting of the lateral surface (Fig. 3A–C), the size of the articular fragments, and bony avulsions of the anterior cruciate ligament (Fig. 4A, arrows) and tibial insertion of the posterior cruciate ligament (Fig. 4B)
• They also assist in determining surgical approaches. For example, an anterolateral cortical fracture identified on axial images (Fig. 5, arrow) may be exploited as a window to the lateral joint surface.
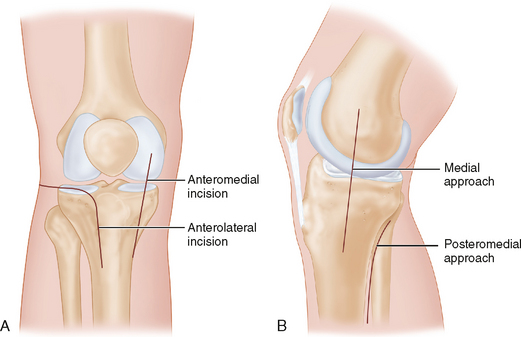
• These injuries may be treated with a variety of dedicated proximal tibial plates, both locking and nonlocking, medial and lateral, through one or two surgical approaches (anterolateral and/or posteromedial).
• Nonreconstructive treatment may be used for very severe injuries that are thought to not be reconstructible, patients who, by age, are candidates for total knee replacement, patients who are nonambulators, or cases in which soft tissue injuries preclude safe surgical management. In such cases, spanning external fixation or external splinting may be used, followed by other surgery or no surgery.
Surgical Anatomy
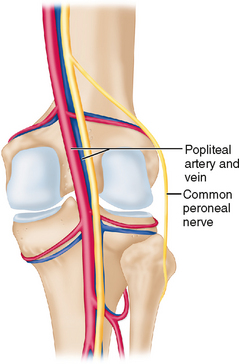
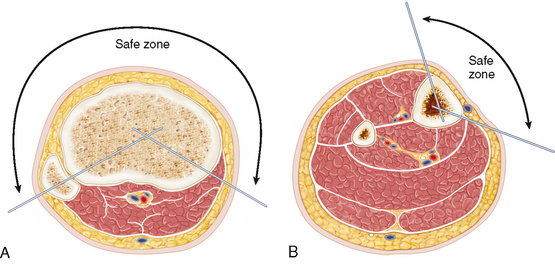
 The perimeter safe zone for the proximal tibia is from the head of the fibula laterally to the posteromedial border of the tibia medially (Fig. 7A). No fine wires or half-pins should penetrate the posterior unsafe zone.
The perimeter safe zone for the proximal tibia is from the head of the fibula laterally to the posteromedial border of the tibia medially (Fig. 7A). No fine wires or half-pins should penetrate the posterior unsafe zone. In the diaphyseal portion of the tibia, the perimeter safe zone begins at the anterolateral border of the tibial spine and continues around to the posteromedial margin of the tibia (Fig. 7B).
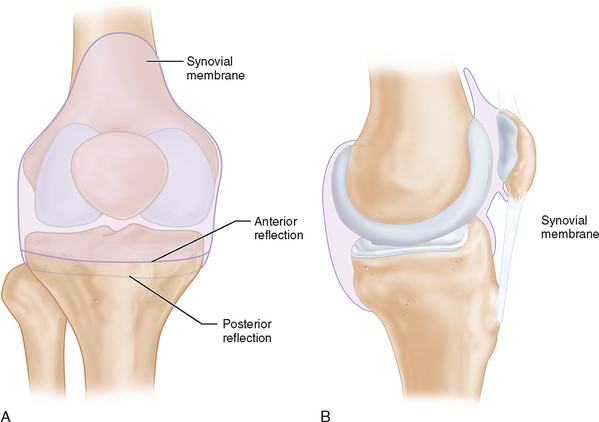
In the diaphyseal portion of the tibia, the perimeter safe zone begins at the anterolateral border of the tibial spine and continues around to the posteromedial margin of the tibia (Fig. 7B). To reduce the risk of infection, it is important that all fine wires and half-pins remain outside of the synovial reflection of the knee joint (Fig. 8A and 8B). For this reason, half-pins and wires should be no closer to the knee joint than 1 cm.
To reduce the risk of infection, it is important that all fine wires and half-pins remain outside of the synovial reflection of the knee joint (Fig. 8A and 8B). For this reason, half-pins and wires should be no closer to the knee joint than 1 cm.Positioning
 The patient is placed in the supine position using one of two tables:
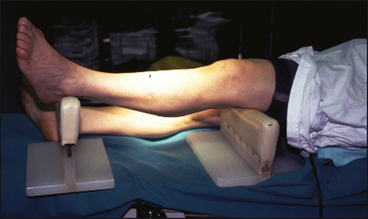
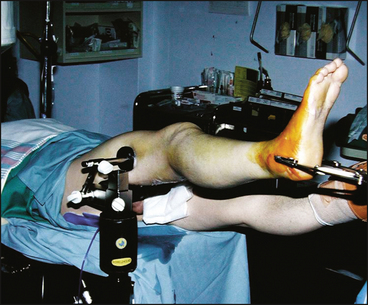
The patient is placed in the supine position using one of two tables:• A radiolucent table with the injured leg elevated by a device that supports the limb at the distal thigh and at the ankle (Fig. 9).
 With either technique, it is important that full access to the proximal tibia be maintained for articular reduction, for frame application, and for radiography.
With either technique, it is important that full access to the proximal tibia be maintained for articular reduction, for frame application, and for radiography.