PROCEDURE 3 Proximal Humerus Fractures
Indications
GENERAL INDICATIONS
 The decision to operate depends on the patient’s physiologic age/functional demands, fracture fragment displacement, and expected ability to reduce fragments and maintain fixation (as reflected by the “bone quality”).
The decision to operate depends on the patient’s physiologic age/functional demands, fracture fragment displacement, and expected ability to reduce fragments and maintain fixation (as reflected by the “bone quality”).SPECIFIC INDICATIONS
• Beware of posterior displacement of GT fractures not seen on standard radiograph (low threshold for computed tomography scan).
• Beware of LT fractures, which may be associated with posterior dislocation (instability, seizure disorder, alcohol withdrawal).
• Precise determination of “number of parts” in a given fracture remains challenging; 3/4-part fractures are grouped because of similar operative treatment.
 Displaced 2-part fractures (see Surgical Anatomy): most are treated with open reduction and internal fixation (ORIF).
Displaced 2-part fractures (see Surgical Anatomy): most are treated with open reduction and internal fixation (ORIF).• Greater tuberosity (GT) fractures
♦ Greater than 5 mm displacement in physiologically young active individual, overhead worker/athlete
Examination/Imaging
• Nonoperative treatment: predictable results are achieved with residual deficit for undisplaced fractures and some displaced fractures in the elderly treated nonoperatively.
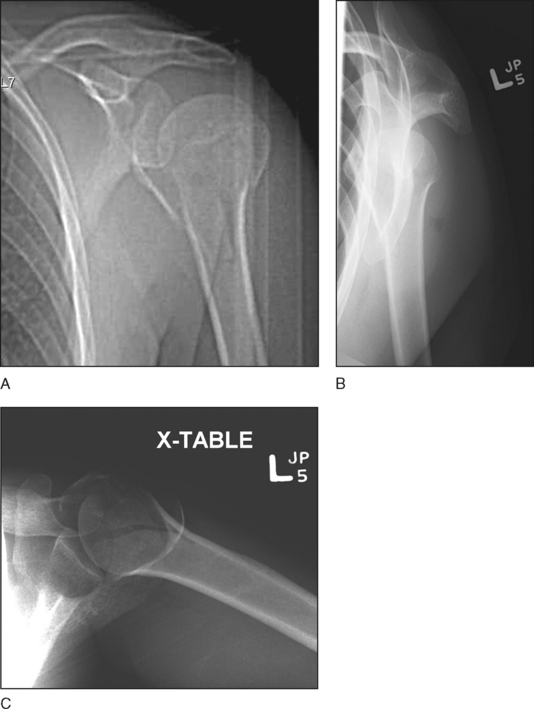
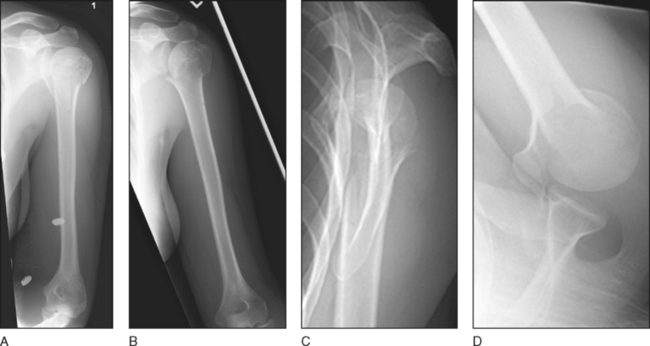
 Plain radiography: shoulder trauma series
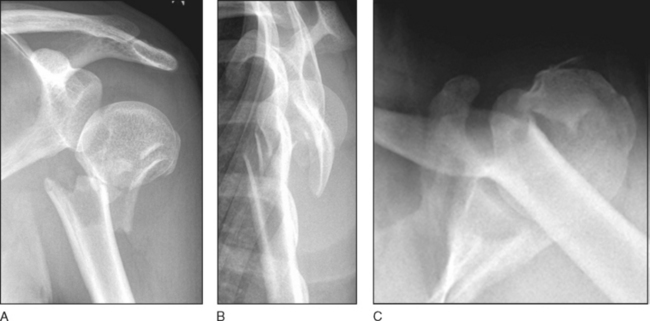
Plain radiography: shoulder trauma series• Anteroposterior (x-ray beam tangential to glenoid/perpendicular to the plane of the scapular body; Fig. 1A), trans-scapular lateral (Fig. 1B), and transaxillary (Fig. 1C) views will establish the diagnosis in most cases.
♦ Figure 3A and 3B shows an extensively comminuted surgical neck fracture in a polytraumatized 29-year-old female (Case 2).
♦ Figure 4A–C shows an unreducible isolated surgical neck fracture in a 25-year-old female (Case 3).
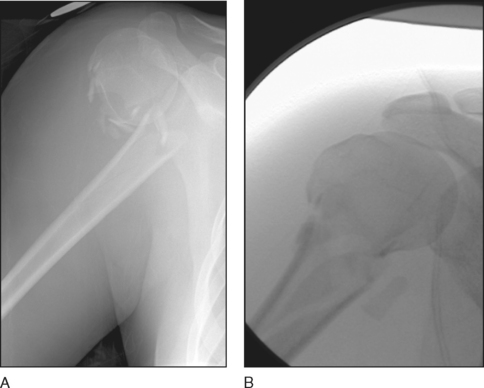
♦ Figure 5A and 5B shows a proximal humeral impacted valgus fracture in a 47-year-old female presenting after a fall from standing height onto her shoulder (Case 4).
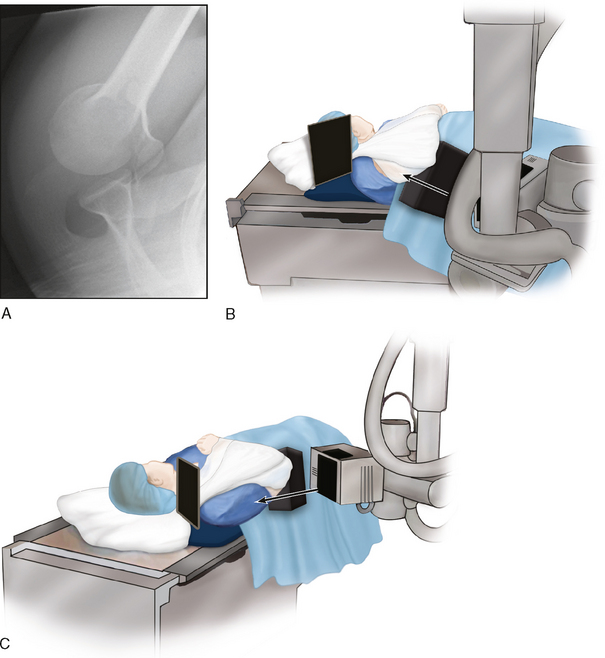
• Consider “bumped-up view” (aka “chicken wing” view) if the standard axillary view with the arm abducted is not clinically feasible (usually quite painful).
♦ To obtain an axial (axillary) view while the patient still comfortably wears a sling, the x-ray cassette is placed superior to the shoulder while the x-ray beam is centered in the axilla starting below the level of the x-ray table, aiming cephalad and anterior (Fig. 7A–C).
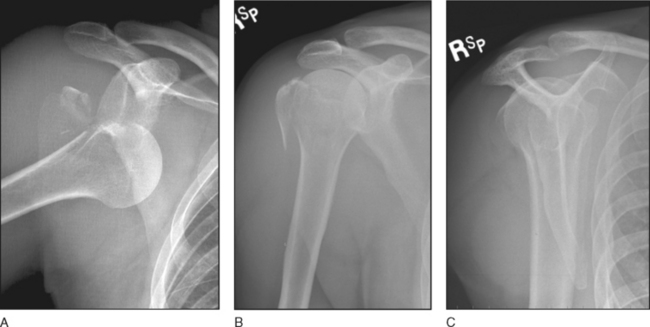
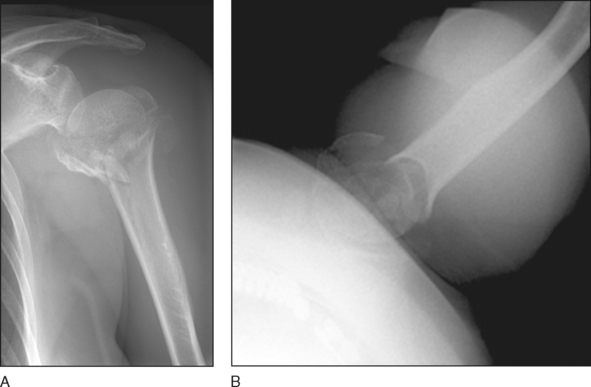
• Additional anteroposterior views of the proximal humerus in internal (Fig. 8A) and external (Fig. 8B) rotation that show the humerus free of the overlapping adjacent scapula help quantify the initial diagnosis and assist with assessment of healing in follow-up.
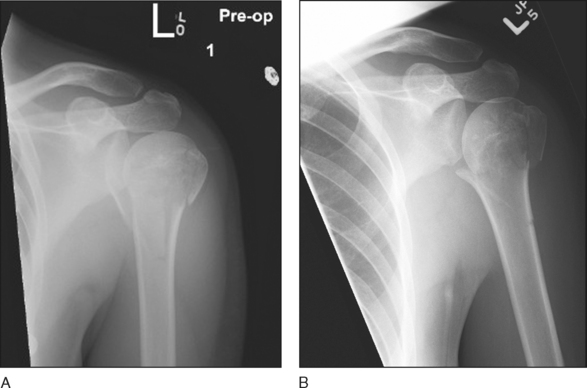
♦ Figure 9 shows a displaced proximal humeral fracture (Fig. 9A and 9B) and its reduction (Fig. 9C and 9D) in a 27-year-old female after a fall onto the left shoulder while snowboarding (Case 6). Note the use of internal (Fig. 9A) and external (Fig. 9B) rotation views to define the fracture preoperatively.
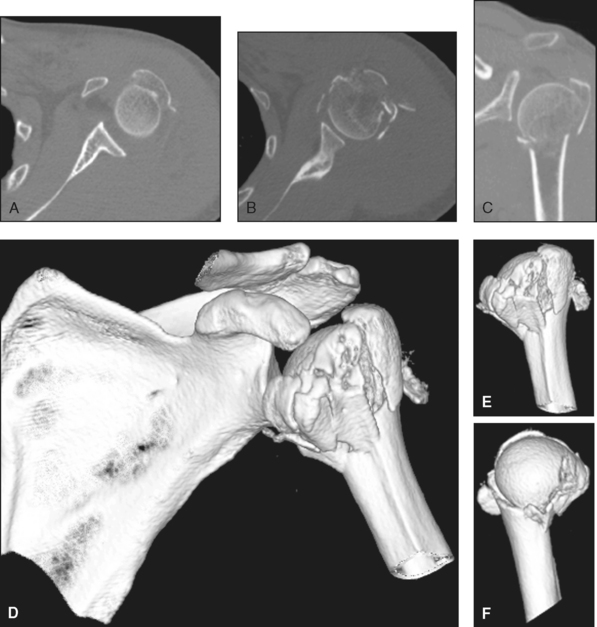
 Computed tomography (CT)
Computed tomography (CT)• Axial CT supplemented with two- and three-dimensional reconstruction is the most useful modality in fracture assessment and preoperative planning.
♦ Figure 10 shows axial (Fig. 10A–C) and three-dimensional reconstructed (Fig. 10D–F) CT images of the proximal humerus impacted valgus fracture in Case 4.
 Magnetic resonance imaging
Magnetic resonance imaging• This may be of value in detecting associated rotator cuff tears or adjacent ligament injuries (acromioclavicular, coracoclavicular); however, it is not practical in the acute trauma setting.
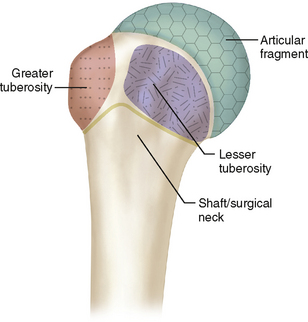
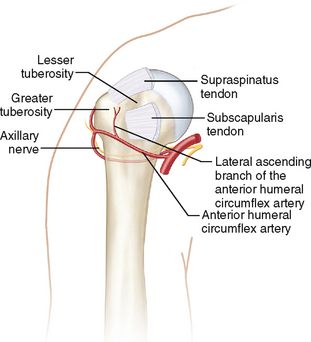
Surgical Anatomy
 Figure 12 shows the osseous anatomy and muscle attachment to the proximal humerus and the surrounding neurovascular structures.
Figure 12 shows the osseous anatomy and muscle attachment to the proximal humerus and the surrounding neurovascular structures. Trabecular and subchondral bone distribution in the proximal humerus is critical to fixation decisions.
Trabecular and subchondral bone distribution in the proximal humerus is critical to fixation decisions.Positioning
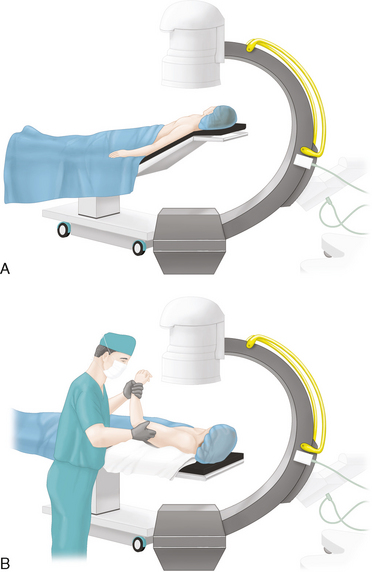
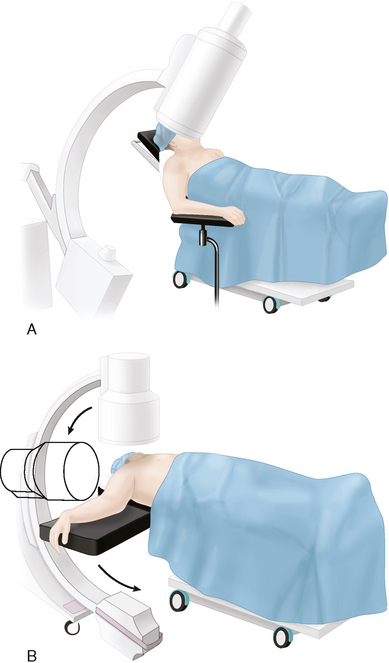
• Positioning it from the contralateral side (if the image intensifier gantry so allows) facilitates the imaging process (see Fig. 13).
 A radiolucent table facilitates intraoperative imaging, and the image intensifier’s position should also be planned as it is an important part of the procedure.
A radiolucent table facilitates intraoperative imaging, and the image intensifier’s position should also be planned as it is an important part of the procedure.Portals/Exposures
• Avoid excessive raising of the head in the beach chair position in the elderly (potential risk to cerebral and/or retinal perfusion).
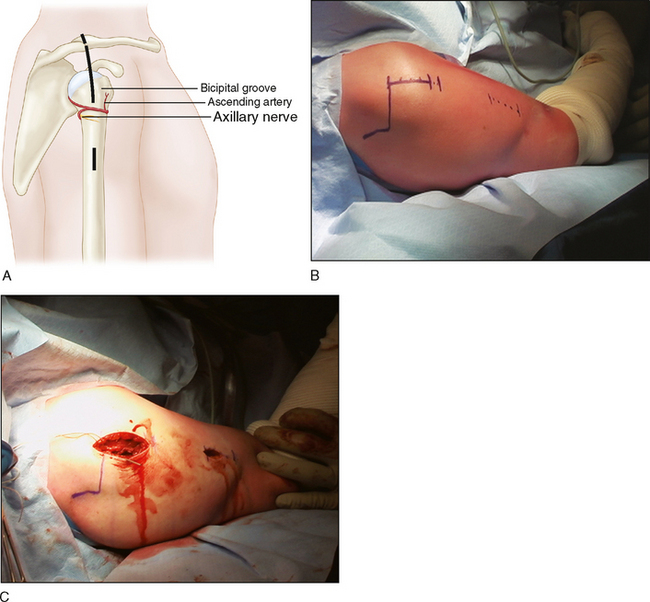
 Deltoid split lateral approach (Fig. 15A; see Video 1)
Deltoid split lateral approach (Fig. 15A; see Video 1)• Incision (Fig. 15B)
♦ The proximal incision is made from the anterolateral corner of the acromion to a maximum of 5 cm distally in line with the anteromedial deltoid raphe. The subdeltoid bursa is opened, and any hematoma evacuated (Fig. 15C)
♦ The proximal extension separates the anterior deltoid from the anterior trapezius at the lateral clavicle.
• Cuff tendons are identified and “tagged” with suture. The rotator cuff interval may be opened to improve deep fragment/joint visualization.
• If distal dissection is required for lateral plate placement, blunt finger dissection along the lateral cortex of the shaft will identify the axillary nerve (“like a piano cord”) and carefully mobilize it. This nerve may be visualized directly but is always palpated and protected by the surgeon’s finger.
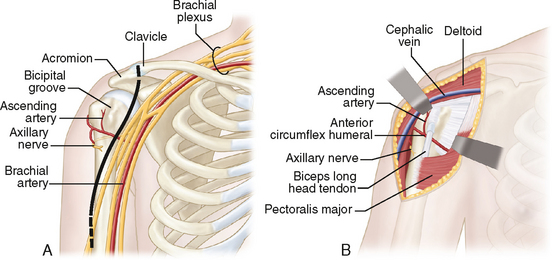
 Deltopectoral anterior approach (Fig. 16A)
Deltopectoral anterior approach (Fig. 16A)• A classic approach is used for exposure, with some specific fracture care steps carried out for reduction and fixation.
• An incision is made from the coracoid tip to the deltoid tuberosity. The cephalic vein is usually retracted laterally. The clavipectoral fascia is incised lateral to the conjoint tendon (Fig. 16B).
• Any hematoma is evacuated. The biceps tendon and tuberosities (on each side of it) are identified and cuff tendons are tagged.
• The arm is abducted to open the subdeltoid space, which is developed. A Hohmann retractor is placed above the tip of the coracoid to expose it superiorly.