PROCEDURE 29 Proximal Tibia Fractures: Intramedullary Nailing
Surgical Anatomy
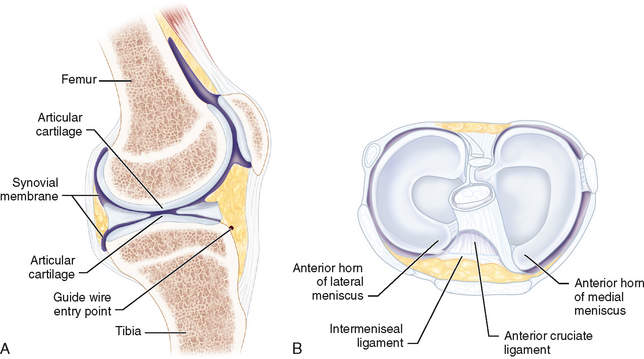
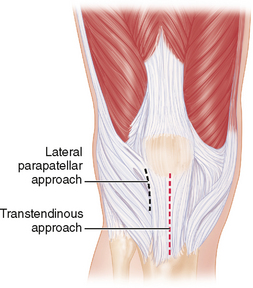
 The entry point in the proximal tibia (Fig. 2A) can endanger the menisci, intermeniscal ligament, and articular surface (Fig. 2B).
The entry point in the proximal tibia (Fig. 2A) can endanger the menisci, intermeniscal ligament, and articular surface (Fig. 2B).Positioning
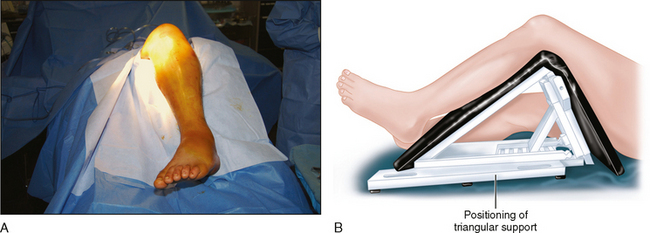
 An adjustable triangular frame is used to support the limb (Fig. 3A and 3B). This allows the knee to be supported in variable degrees of flexion during the procedure.
An adjustable triangular frame is used to support the limb (Fig. 3A and 3B). This allows the knee to be supported in variable degrees of flexion during the procedure. When maximal flexion is needed, we find it easier to slide the leg off the triangular frame and have an assistant hold it in the desired degree of flexion. This is mostly useful for insertion of the entry reamer, to ensure that the reamer enters the metaphysis parallel to the anterior cortex of the tibia.
When maximal flexion is needed, we find it easier to slide the leg off the triangular frame and have an assistant hold it in the desired degree of flexion. This is mostly useful for insertion of the entry reamer, to ensure that the reamer enters the metaphysis parallel to the anterior cortex of the tibia.