INTRODUCTION
An orthosis, a mechanical device that is fitted and applied to the body, is used to modify structural or functional characteristics of the neuromusculoskeletal system. To that end, orthotic treatment is often employed to relieve pain, manage deformities, and attenuate abnormal neuromuscular function. More specifically, orthotic treatment may be used to (1) prevent, reduce, or stabilize a deformity; (2) modify the range of motion of a joint; (3) add to the length or alter the shape of a segment; (4) compensate for weak muscle activity or control muscle hyperactivity; and (5) reduce or redistribute the load on tissues. Orthoses may be commonly referred to as braces or splints.
Rehabilitation physicians often work with orthotists. In conjunction with the physician, the orthotist designs and fabricates an orthosis to meet the specific needs of the patient. Proper fit and alignment of an orthosis is paramount in order for a patient to benefit from its use. An orthosis that is incorrectly fitted or uncomfortable does not confer the desired effect and may be cosmetically unacceptable to the patient. This orthosis is less likely to be worn and represents a missed opportunity to help a patient. In such cases the ill-fitting orthosis may be either modified or replaced.
It is the joint responsibility of the physician and the orthotist to ensure that an orthosis is fitted properly and that the patient is instructed in its proper use. In circumstances where a custom fit is not essential, a variety of prefabricated orthoses may be used. However, prefabricated devices are often difficult, if not impossible, to modify due to the lack of plasticity of the materials and their inherent fragility once tampered with. It is therefore still absolutely essential for the physician to ensure that the orthosis is appropriate and fits correctly.
UPPER EXTREMITY ORTHOTICS
The function of the upper extremity, in maneuvering the hand so that it may access and manipulate objects in space, is achieved through prehension, which is the act of taking hold, seizing, or grasping an object. The shoulder, elbow, and wrist function together to place the hand in a desired locale for fine and gross motor tasks. The main goal of upper extremity orthoses, therefore, is to maintain the function of the hand, either by restoring or preserving prehension itself, or by allowing optimal positioning of the hand in space in order to manipulate objects in the environment. In this regard five common goals in upper extremity orthotics are (1) substituting for weak or absent muscles, (2) protecting damaged or diseased segments by limiting loads or motion, (3) preventing deformity, (4) correcting contracture, and (5) attaching to other assistive devices.
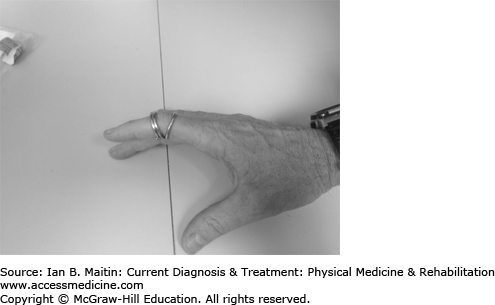
The swan-neck deformity is often seen in patients with rheumatoid arthritis and is characterized by hyperextension of the proximal interphalangeal (PIP) joint and flexion of the distal interphalangeal (DIP) joint. Finger–thumb orthoses such as the silver ring splint, the oval-eight splints, and thermoplastic splints can be used to correct the hyperextension of the PIP joint and prevent further progression of the deformity (Figure 28–1).
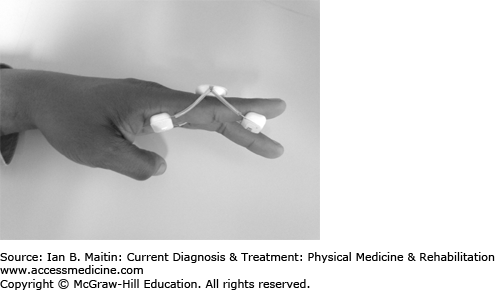
Like swan-neck deformity, the boutonnière deformity is also commonly seen in rheumatoid arthritis patients. But this deformity, conversely, produces flexion of the PIP joint and hyperextension of the DIP joint. The orthoses used are the same: finger–thumb orthoses such as the silver ring splint, the oval-eight splint, and thermoplastic splints. These correct the flexion of the PIP joint and prevent further progression of the deformity (Figure 28–2).
Mallet finger results from a tear or avulsion of the extensor tendon as it cross the DIP joint. Examination reveals a finger that lags in extension at the DIP. Splinting of the DIP joint in extension is aimed at allowing for healing of the torn or avulsed tendon in its shortened state.
Trigger finger results from inflammation of the flexor tendon as it courses through the first annular (A1) pulley. This produces a DIP joint that is stuck in flexion. A palpable nodule may be present at the point of inflammation. Splinting of the DIP joint in extension or the metacarpophalangeal (MCP) joint in slight flexion allows the inflammation to resolve and is part of the management of this ailment.
Patients with flexor tendon injury often have difficulty achieving full flexion at the PIP joint. Finger knuckle bender splints may be used to increase flexion in the affected joint. These splints have a point of pressure at the volar aspect of the PIP joint and points of counterpressure at the dorsal aspect of the proximal and middle phalanx, and utilize rubber bands to provide force to flex the joint. The goal of this orthosis is to increase range of motion with regard to flexion at the PIP joint.
In median or ulnar nerve injuries the MCP joint has a tendency to become hyperextended due to lack of muscle strength in the hand intrinsics. Opposition often is lost in solitary median nerve injuries. Hand–finger orthoses can be used to control the MCP joint of the fingers and thumb. A C-bar is used to maintain the web space. An opponens bar is used so that the thumb opposes the other fingers, placing it in a position to maintain pinch grip. The goal of these orthoses is to prevent contracture formation and preserve hand function to perform gross motor tasks. In the event that the MCP joint becomes contracted, the hand–finger knuckle bender splint (a dynamic hand–finger orthosis) can be used to stretch the MCP joint. Like the finger knuckle bender, it uses either rubber bands or wires to provide flexion force.
Patients with radial nerve injury may lack wrist and finger extension. Lack of wrist extension puts the finger flexors on slack and compromises grasp and full finger flexion. Dorsal wrist extension dynamic finger splints and static wrist volar cock-up splints are used in radial nerve injury to extend the wrist and allow the fingers to flex more effectively for grasping activities.
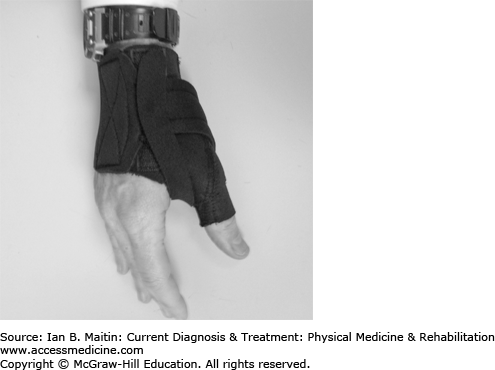
Carpal tunnel syndrome results from compression or inflammation of the median nerve as it courses under the transverse carpal ligament in the wrist. Wrist–hand–finger orthoses are used to control motion through the wrist and proximal hand, with the goal of providing symptom relief or conferring a mechanical advantage in order to improve prehension. In carpal tunnel syndrome, the wrist is placed into a few degrees of extension while allowing for freedom of thumb and finger movement (Figure 28–3). Immobilization of the wrist in carpal tunnel syndrome is thought to allow inflammation to resolve.
Gamekeeper’s thumb results from a tear of the ulnar collateral ligament of the thumb. Patients present with pain and swelling on the posterior medial aspect of the thumb and instability, with a tendency for the thumb to go into hyperabduction. A thumb spica splint is used to protect and immobilize the injured segment and allow it to heal (Figure 28–4).
De Quervain’s tenosynovitis results in pain at the base of the thumb or wrist. It is caused by inflammation of the extensor pollicis brevis and abductor pollicis longus tendon sheaths. Patients often have pain at the base of the thumb with thumb extension or ulnar deviation of the wrist. A thumb spica splint is used to immobilize the inflamed segment and allow it to heal.
A thumb spica splint may initially be used to manage fractures or ligamentous and neurovascular injuries of the thumb until the patient can be further evaluated by a hand specialist. In these cases the objective of the orthosis is to protect and immobilize the thumb in order to limit pain and allow use of the other digits. Dorsal wrist extension dynamic finger splints and static wrist volar cock-up splints are used in radial nerve injury to extend the wrist and allow the fingers to flex more effectively for grasping activities.
Arthritis of the first carpometacarpal joint may be treated with a long and short opponens splint. Resting wrist hand splints have been shown to give relief to symptomatic patients suffering from rheumatoid arthritis.
Patients with C6 tetraplegia often have preserved elbow flexion and wrist extension but do not have use of their hand and finger muscles. The tenodesis prehension orthosis takes advantage of the finger flexion that normally occurs passively with wrist extension to allow these patients to grasp objects.
Static progressive and dynamic elbow splints are often used to stretch flexion contracture of the elbow and improve range of motion after trauma.
Dynamic spring-assisted orthoses are available for patients with elbow flexor weakness.
Cubital tunnel syndrome results from compression of the ulnar nerve at the elbow. Patients often have sensory complaints and motor deficits in an ulnar distribution in the hand. Nocturnal splinting of the elbow at 30–35 degrees of flexion, the forearm in 10–20 degrees of pronation, and the wrist in neutral position has been shown to be effective in treating this condition. The objective of splinting is to reduce traction on the ulnar nerve and provide symptomatic relief.
The Sarmiento brace is a prefabricated nonarticular orthosis used for the conservative treatment of humeral shaft fractures. It remains the treatment of choice for nondisplaced or minimally displaced fractures, even in an era of newer intramedullary procedures and minimally invasive techniques. This orthosis is applied to the humerus and fastened with Velcro straps to maintain approximation of the distal and proximal aspects of the fracture. Bracing does not restore anatomic alignment to the fracture segment, but the end results are usually cosmetically and functionally acceptable. A benefit of this bracing method is that it allows for full range of motion at the elbow and shoulder and thus is effective in avoiding complications such as elbow flexion contracture and adhesive capsulitis.
Clavicular fractures account for 2.5–5% of all fractures, and various classification schemes have been developed to describe them. Classically, they were divided into three types: type I, involving the middle third of the clavicle; type II, involving the distal clavicle; and type III, involving the proximal clavicle. Types I and III may be treated conservatively with a figure-of-eight splint or shoulder sling. Type II may be treated with surgical fixation as these fractures have a high rate of nonunion. The objective of splinting for clavicular fractures is to maintain glenohumeral integrity and also to limit motion across the acromioclavicular (AC) and glenohumeral joints.
AC joint separation is a common injury in younger, physically active patients. These joint separations may be classified into six types. In type I, the AC ligaments are sprained; in type II, they are torn but the coracoclavicular (CC) ligaments are intact; in type III, the AC and CC ligaments are both torn; in type IV, the clavicle is displaced posteriorly; in type V, the AC and CC ligaments are torn and the deltotrapezial fascia are also torn, causing the scapula to droop inferiorly; and in type VI, AC injury occurs when the clavicle dislocates inferiorly to the coracoid. Types I and II may be treated conservatively with a sling. Types IV, V, and VI are treated operatively as there is high risk of morbidity due to dislocation and soft tissue damage. The treatment of type III AC joint separations is not as clear. These injuries may be treated conservatively with a shoulder sling initially; however, if there is persistent pain or disability an operative course may be pursued. The objective of splinting in the patient with an AC joint separation is to maintain glenohumeral integrity and also to limit motion across the AC and glenohumeral joints.
Glenohumeral dislocations may be treated with an adduction arm splint. Traditionally, the shoulder is also placed in internal rotation, but studies have shown that placement in neutral or even external rotation may be more beneficial. Several shoulder orthoses have been devised for stroke patients with post-stroke shoulder pain and issues with glenohumeral subluxation. These consist of various slings and arm trays that allow the shoulder to rest in a position of comfort and support the shoulder joint by compensating for muscles affected by the stroke. Patients may also neglect or have impaired sensation in the affected arm after a stroke, and these devices protect the upper limb from injury, keeping it in view and close to the body. The airplane splint and gunslinger orthosis can be used to immobilize the shoulder and keep the arm fixed in relation to the torso. These may be employed postoperatively after soft tissue repairs, fractures, and brachial plexus injuries. The balanced forearm orthosis is a shoulder–elbow–wrist–hand orthosis that supports the upper limb in a gravity-eliminated position so that patients with weakness in their shoulder flexors and elbow flexors (eg, high-level tetraplegia) can gain access to the face and mouth for feeding.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree