PROCEDURE 27 Operative Treatment of Fractures of the Patella
 Operative treatment of displaced patella fractures is the standard of care due to the increased incidence of nonunion and loss of extensor mechanism strength associated with nonoperative treatment and prolonged knee immobilization (Chen et al., 1998).
Operative treatment of displaced patella fractures is the standard of care due to the increased incidence of nonunion and loss of extensor mechanism strength associated with nonoperative treatment and prolonged knee immobilization (Chen et al., 1998). Current techniques include open reduction and internal fixation with screws or various forms of anterior tension band techniques and partial or total patellectomy.
Current techniques include open reduction and internal fixation with screws or various forms of anterior tension band techniques and partial or total patellectomy. Several studies have found that biodegradable materials or strong sutures yield similar clinical and biomechanical results when compared to traditional wire tension band techniques (Bostman et al., 1983; Hung et al., 1985; Jakobsen et al., 1985).
Several studies have found that biodegradable materials or strong sutures yield similar clinical and biomechanical results when compared to traditional wire tension band techniques (Bostman et al., 1983; Hung et al., 1985; Jakobsen et al., 1985).Examination/Imaging
PHYSICAL EXAMINATION
 Open knee wounds should be examined thoroughly to determine if they communicate with the fracture site or the knee joint.
Open knee wounds should be examined thoroughly to determine if they communicate with the fracture site or the knee joint. Full active or passive range of motion of the affected knee should be avoided until imaging has been obtained due to the potential for further injury to the patellar retinaculum or further fracture displacement.
Full active or passive range of motion of the affected knee should be avoided until imaging has been obtained due to the potential for further injury to the patellar retinaculum or further fracture displacement.IMAGING STUDIES
 Anteroposterior, lateral, and sunrise views of the affected patella should be obtained (Fig. 1A and 1B).
Anteroposterior, lateral, and sunrise views of the affected patella should be obtained (Fig. 1A and 1B). Magnetic resonance imaging may be used to identify marginal patella fractures or free osteochondral fragments. It may also help to identify concurrent ligamentous injuries.
Magnetic resonance imaging may be used to identify marginal patella fractures or free osteochondral fragments. It may also help to identify concurrent ligamentous injuries. Computed tomography may be used for evaluation of associated distal femoral or proximal tibial fractures.
Computed tomography may be used for evaluation of associated distal femoral or proximal tibial fractures.Surgical Anatomy
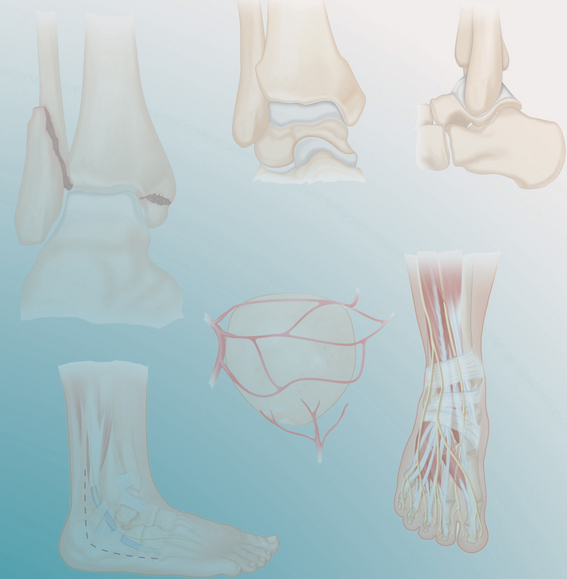
 The patella is a subcutaneous bone with minimal soft tissue covering. It is the largest sesamoid bone of the body and lies within the fascia lata and the fibers of the quadriceps tendon.
The patella is a subcutaneous bone with minimal soft tissue covering. It is the largest sesamoid bone of the body and lies within the fascia lata and the fibers of the quadriceps tendon. The upper three fourths of the posterior surface of the patella is covered with articular cartilage that is divided into major medial and lateral facets.
The upper three fourths of the posterior surface of the patella is covered with articular cartilage that is divided into major medial and lateral facets. The patella is served by both extraosseous and intraosseous vascular systems.
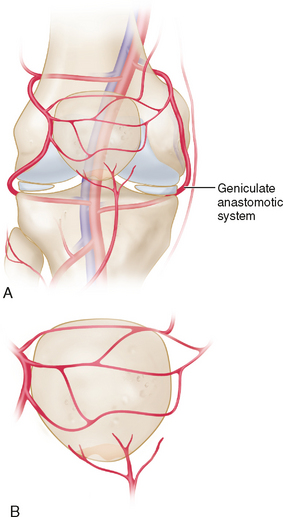
The patella is served by both extraosseous and intraosseous vascular systems.• The primary blood supply to the patella is from branches of the geniculate anastomotic system around the knee (Fig. 2A).
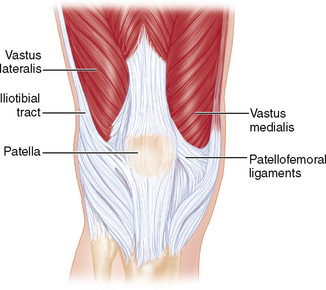
 The patella is surrounded and anchored by a strong retinaculum derived from the deep fibers of the tensor fascia lata in combination with fibers from the vastus medialis, vastus lateralis, iliotibial tract, and patellofemoral ligaments (Fig. 3).
The patella is surrounded and anchored by a strong retinaculum derived from the deep fibers of the tensor fascia lata in combination with fibers from the vastus medialis, vastus lateralis, iliotibial tract, and patellofemoral ligaments (Fig. 3). The patellar tendon originates at the apex of the patella and inserts onto the tibial tubercle, blending with the patellar retinaculum and the iliotibial tract fibers (see Fig. 3).
The patellar tendon originates at the apex of the patella and inserts onto the tibial tubercle, blending with the patellar retinaculum and the iliotibial tract fibers (see Fig. 3).Positioning
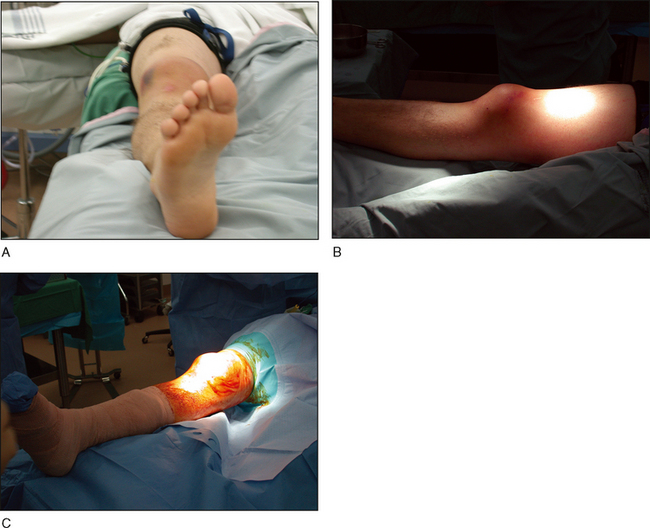
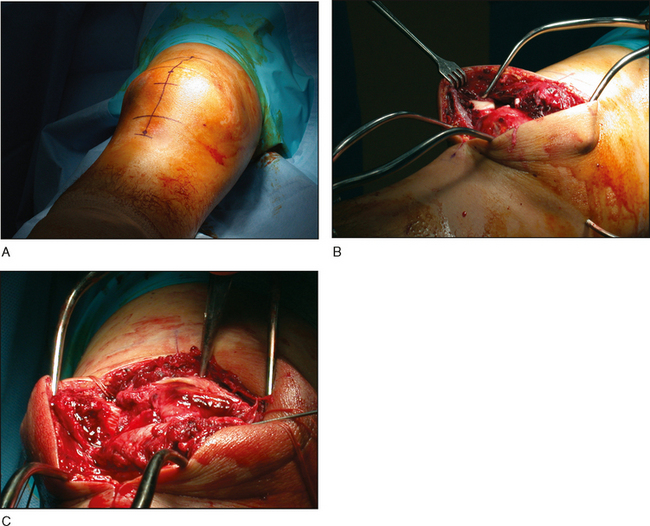
 The procedure is performed with the patient in the supine position on a radiolucent table with a tourniquet on the proximal thigh (Fig. 4A and 4B).
The procedure is performed with the patient in the supine position on a radiolucent table with a tourniquet on the proximal thigh (Fig. 4A and 4B). Prior to tourniquet inflation, gentle traction on the quadriceps/patellar fragment will keep the tendon nearer to anatomic length prior to reduction.
Prior to tourniquet inflation, gentle traction on the quadriceps/patellar fragment will keep the tendon nearer to anatomic length prior to reduction. A bump should be placed under the ipsilateral hip to help internally rotate the knee to a neutral position.
A bump should be placed under the ipsilateral hip to help internally rotate the knee to a neutral position. The leg must be free draped to allow easy flexion/extension of the knee throughout the surgery (Fig. 4C).
The leg must be free draped to allow easy flexion/extension of the knee throughout the surgery (Fig. 4C).Portals/Exposures
 Medial and lateral full-thickness flaps are developed and exposure of both retinacula is obtained (Fig. 5B).
Medial and lateral full-thickness flaps are developed and exposure of both retinacula is obtained (Fig. 5B).Procedure: Irrigation and Débridement of Open Fractures
 Due to the risk of bone and intra-articular infections, irrigation and débridement of the fracture should be performed within 6–8 hours.
Due to the risk of bone and intra-articular infections, irrigation and débridement of the fracture should be performed within 6–8 hours.STEP 1
 All nonviable tissue and bone fragments should be resected with the exception of large osteochondral fragments, which may need to be retained.
All nonviable tissue and bone fragments should be resected with the exception of large osteochondral fragments, which may need to be retained.