PROCEDURE 26 Knee Dislocations
Indications
Examination/Imaging
 Magnetic resonance imaging (MRI)
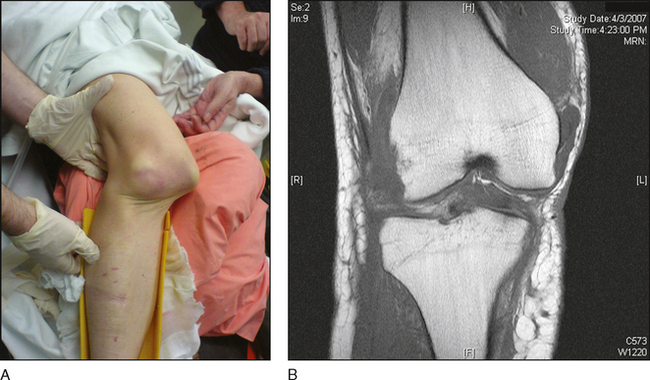
Magnetic resonance imaging (MRI)• MRI provides additional information, such as the residual subluxation shown in Figure 1B, but does not replace the clinical examination!
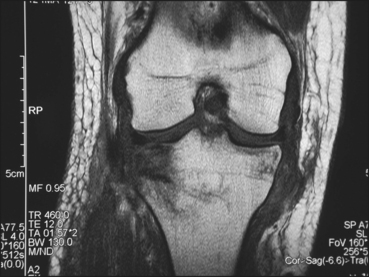
• It can be very helpful in delineating ligamentous injury, such as the medial collateral ligament injury shown in Figure 2.
• Management of combined anterior cruciate ligament (ACL)/medial collateral ligament (MCL) injuries is debatable. They can be treated conservatively initially in a hinged brace to let the MCL heal, followed by reconstruction of the ACL as needed.
• Nonoperative treatment is generally not recommended for most two-ligament injuries, or for any three- and four-ligament injuries. The results are unpredictable, with either recurrent instability or stiffness being likely. Recent literature contains multiple articles confirming that operative treatment gives better functional results.
• One can temporize while working up a patient for surgery by placing him or her in a knee immobilizer. Usually spanning external fixation is not required (if performed, pin tracks should be kept away from proposed incisions).
• Surgical treatment (reconstruction or repair) should be the mainstay of care in most patients, who should ideally be reconstructed/repaired acutely (within 2 weeks—anatomy is more definable at 1 week as compared to 2 weeks).
• If the dislocation is irreducible, the patient must be treated operatively.
 Performing closed reduction immediately, in either the emergency room or the operating room, is essential to improve chances of limb salvage (i.e., the risk of amputation increases the longer the knee is dislocated).
Performing closed reduction immediately, in either the emergency room or the operating room, is essential to improve chances of limb salvage (i.e., the risk of amputation increases the longer the knee is dislocated).
 Performing closed reduction immediately, in either the emergency room or the operating room, is essential to improve chances of limb salvage (i.e., the risk of amputation increases the longer the knee is dislocated).
Performing closed reduction immediately, in either the emergency room or the operating room, is essential to improve chances of limb salvage (i.e., the risk of amputation increases the longer the knee is dislocated).Surgical Anatomy
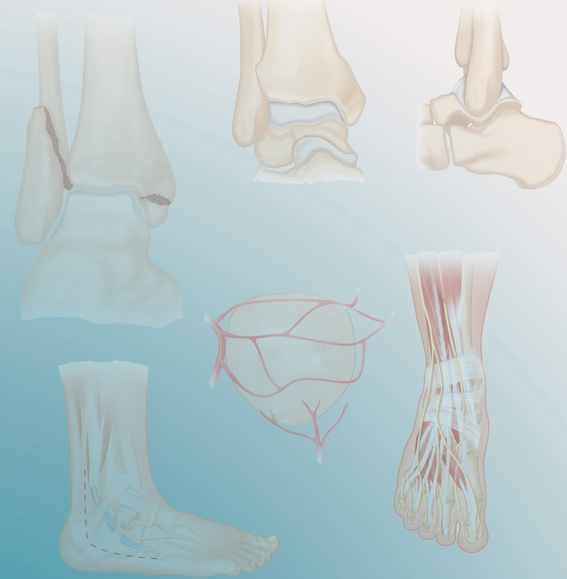
 The surgeon should be familiar with the origins and insertions of the various ligaments that are injured:
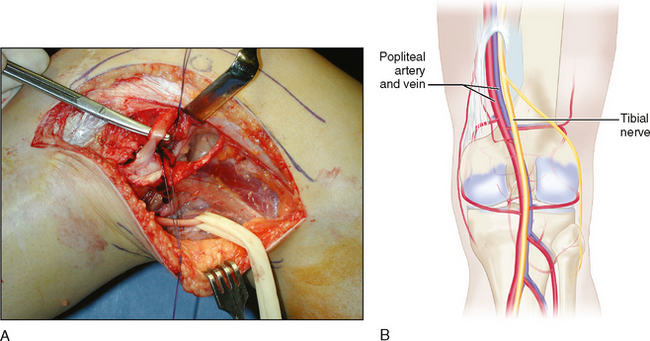
The surgeon should be familiar with the origins and insertions of the various ligaments that are injured: The surgeon should be familiar with the neurovascular anatomy of the knee.
The surgeon should be familiar with the neurovascular anatomy of the knee.• Course of the common peroneal nerve about the knee (inferior to the biceps, running around the fibular neck) for lateral repairs/reconstructions (Fig. 3A)
Portals/Exposures
 For chronic cruciate reconstructions (i.e., ACL or PCL), the surgeon can cheat closer to the midline with arthroscopic portals.
For chronic cruciate reconstructions (i.e., ACL or PCL), the surgeon can cheat closer to the midline with arthroscopic portals. For acute reconstructions, an open anterior incision with a medial parapatellar arthrotomy (similar to total knee replacement) can give good access to the ACL, PCL, and MCL if a medial flap is developed (Fig. 5).
For acute reconstructions, an open anterior incision with a medial parapatellar arthrotomy (similar to total knee replacement) can give good access to the ACL, PCL, and MCL if a medial flap is developed (Fig. 5). For lateral and posterolateral corner procedures, a lateral-based incision provides excellent exposure (see Fig. 5).
For lateral and posterolateral corner procedures, a lateral-based incision provides excellent exposure (see Fig. 5). The surgeon may need to incorporate fasciotomy incisions if there is a vascular injury requiring repair.
The surgeon may need to incorporate fasciotomy incisions if there is a vascular injury requiring repair.• Standard self-retaining retractors/Gelpis and Hohmann retractors to keep the patella lateral while working on the notch
• A lateral incision can run from Gerdy’s tubercle on the tibia to just anterior to the lateral epicondyle of the femur, and continue longitudinally up the femoral shaft.
• Putting the scope through the notch to the back of the knee and turning the post to view medially can help transilluminate the correct placement of a posteromedial portal (especially with a 70° scope).
• Reducing the posterior translation of the tibia to a forward position can also be extremely helpful in inserting a posteromedial cannula.