PROCEDURE 25 Supracondylar Femur Fractures
Indications
 Retrograde nailing is an option in AO/OTA Classification type A, C1, or C2 distal femur fractures (i.e., supracondylar fractures with or without intercondylar fracture, and without significant condylar comminution). The supracondylar fracture line must be proximal enough to allow placement of at least two distal locking screws.
Retrograde nailing is an option in AO/OTA Classification type A, C1, or C2 distal femur fractures (i.e., supracondylar fractures with or without intercondylar fracture, and without significant condylar comminution). The supracondylar fracture line must be proximal enough to allow placement of at least two distal locking screws.Examination/Imaging
• Options for operative management include lateral locked plating, 95° dynamic condylar screw, or blade-plate fixation. These can be done through traditional open approachs or minimimally invasive approaches.
• Temporary spanning external fixation may be used if patient or soft tissue concerns preclude immediate definitive fixation. If a nail is to be used after external fixation for definitive management, the time interval for exchange should be kept to a minimum to decrease the risk of intramedullary sepsis (Bhandari et al., 2005).
 Physical examination
Physical examination• The usual mechanism of injury is an axial load in combination with a varus, valgus, or rotational force.
• In older patients with poor bone quality such an injury may result from a simple fall on a flexed knee, but in younger patients high-energy trauma is often required.
• The physical examination must include a thorough assessment to rule out the possibility of additional injury.
♦ One must assess for the possible presence of concomitant fracture of the pelvis, ipsilateral acetabulum, femoral neck, femoral shaft, patella, tibial plateau, and tibial shaft.
♦ Ligamentous stability of the ipsilateral knee must also be assessed, although this may be difficult in the initial postinjury period.
♦ The femoral and popliteal arteries are at risk of injury (especially in the setting of posterior dislocation of the knee), and circulation should be assessed by palpating for the popliteal, dorsalis pedis, and posterior tibialis pulses.
• In a trauma situation, one must consider the broader picture and conduct the appropriate trauma assessment according to Advanced Trauma Life Support guidelines (American College of Surgeons, 2002).
• On inspection, tenderness, swelling, and deformity are typical findings. The classic deformity is a combination of shortening, apex posterior angulation, and posterior displacement of the distal fragment. Gross deformity should be gently reduced and the limb splinted in preparation for imaging.
 Plain radiographs
Plain radiographs• Minimum imaging includes anteroposterior (AP) (Fig. 1A) and lateral (Fig. 1B) views of the knee, femur, and hip, as well as an AP view of the pelvis.
• Additional 45° oblique views of the fracture site should be considered for evaluation of complex intra-articular fractures or fractures not clearly delineated on standard views.
 Computed tomography is useful for diagnosis and preoperative planning of suspected complex intra-articular fractures and osteochondral lesions.
Computed tomography is useful for diagnosis and preoperative planning of suspected complex intra-articular fractures and osteochondral lesions. Magnetic resonance imaging is useful in the evaluation of suspected ligamentous and musculotendinous injuries.
Magnetic resonance imaging is useful in the evaluation of suspected ligamentous and musculotendinous injuries. Angiography may be indicated in the setting of diminished or absent pulses, an expanding hematoma, or arterial bleeding through an open wound. Given that the site of vascular disruption is usually at the site of the fracture, the use of arteriography should be at the discretion of the vascular surgeon and may be done as a “one-shot” examination in the operating room.
Angiography may be indicated in the setting of diminished or absent pulses, an expanding hematoma, or arterial bleeding through an open wound. Given that the site of vascular disruption is usually at the site of the fracture, the use of arteriography should be at the discretion of the vascular surgeon and may be done as a “one-shot” examination in the operating room.Surgical Anatomy
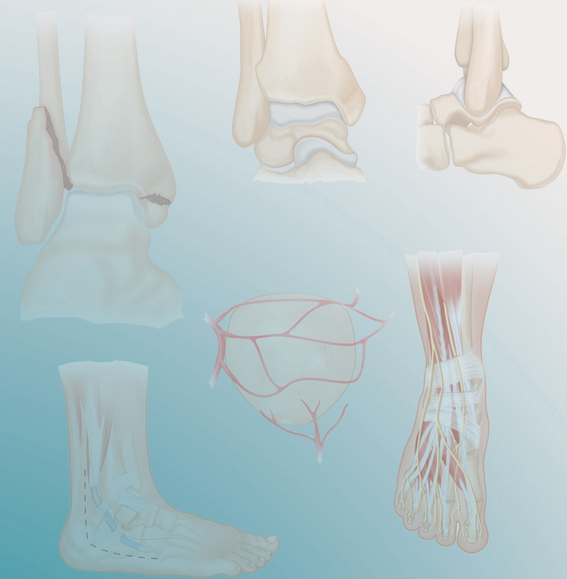
 Bony anatomy (Fig. 2A and 2B)
Bony anatomy (Fig. 2A and 2B)• “Supracondylar” indicates the zone between the femoral condyles and the junction of the metaphysis with the diaphysis (distal 9–15 cm of femur).
• At the distal diaphyseal-metaphyseal junction, the femur flares in the coronal plane into the medial and lateral condyles, and in the sagittal plane the condyles bulge posteriorly. Thus, the central axis of the femoral shaft projects onto the center of the intercondylar notch, 0.5–1 cm anterior to the origin of the posterior cruciate ligament, at the margin of the patellofemoral articular surface.
• The axis of the femoral shaft is normally at 9° (range 7–11°) of valgus angulation relative to a line drawn perpendicular to the distal condylar surface.
 Muscular and ligamentous attachments (Fig. 3)
Muscular and ligamentous attachments (Fig. 3)• The quadriceps (rectus femoris, vastus medialis, vastus intermedius, and vastus lateralis), hamstrings (biceps femoris, semitendinosus, semimem-branosus), adductor magnus, and medial and lateral heads of the gastrocnemius effect the primary deforming forces acting on the distal femur.
 Neurovascular structures (Fig. 4)
Neurovascular structures (Fig. 4)• The femoral artery and vein pass posteriorly through the adductor hiatus of the adductor magnus in close association with the medial aspect of the femur in the high supracondylar region and continue in close association with the distal femur as they wind posteriorly through the popliteal fossa.
• Superior lateral and superior medial genicular arteries branch off from the femoral artery near the superior border of the femoral condyles and course anteriorly, encircling the condyles.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree