PROCEDURE 24 Supracondylar Femur Fractures
Surgical Anatomy
• Alternatives to open reduction and internal fixation include retrograde intramedullary nailing, cast or brace treatment, and (rarely) revision total knee arthroplasty.
• Prep the limb as high as possible and use a sterile tourniquet during the entire case. If necessary, do the articular reduction under tourniquet control and deflate for the reduction of the condyles to the shaft.
• Preparation and exposure of the ipsilateral iliac crest may be useful if bone grafting is anticipated.
• Use of a femoral distractor or external fixator can greatly aid in reduction of the fracture (especially intra-articular components).
 The most important structure at risk is the superficial femoral artery, which enters the popliteal fossa around 10 cm proximal to the knee joint as it passes through the adductor magnus. (Be especially cautious with the medial approach.)
The most important structure at risk is the superficial femoral artery, which enters the popliteal fossa around 10 cm proximal to the knee joint as it passes through the adductor magnus. (Be especially cautious with the medial approach.) Soft tissues
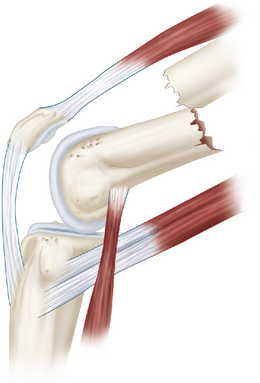
Soft tissues• The quadriceps muscle anteriorly (rectus femoris, vastus medialis, vastus intermedius, and vastus lateralis) is separated from the posterior compartment (hamstring muscles) by the medial and lateral intermuscular septa. These large muscles shorten the fracture, and their force must be overcome in reduction techniques.
 Bone
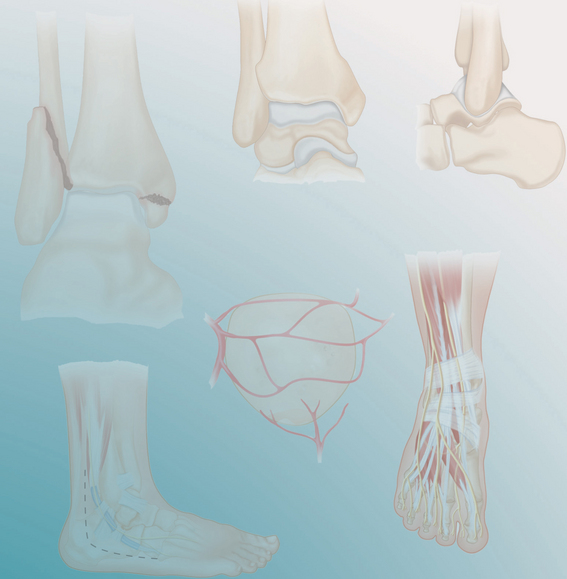
Bone• The distal femur has many unique features that are critical to understand for reduction and fixation techniques.
• The metaphysis widens at the end of the femoral diaphysis and supports the femoral condyles. Anteriorly, a shallow articular concavity between the condyles provides a contact surface for the patella. Posteriorly, the intercondylar fossa separates the condyles and is the attachment area for the cruciate ligaments.
• In the lateral projection, the femoral shaft aligns with the anterior half of the lateral condyle (Fig. 2).
• The lateral femoral condyle is larger anterior to posterior than the medial condyle and has a flat lateral surface. The medial condyle is wider posteriorly, and this creates the trapezoidal shape to the distal femur when viewed end on (Fig. 3). This is extremely important in placing fixation devices to avoid errant hardware placement and to avoid malreductions such as medial translation.
Positioning
 The most widely accepted position for fixation of supracondylar femur fractures is with the patient supine on a radiolucent table. This allows for C-arm fluoroscopy intraoperatively.
The most widely accepted position for fixation of supracondylar femur fractures is with the patient supine on a radiolucent table. This allows for C-arm fluoroscopy intraoperatively. The operative hip can be elevated on a sandbag, rolled flannel, or intravenous solution bag to rotate the femur and knee into a true AP projection.
The operative hip can be elevated on a sandbag, rolled flannel, or intravenous solution bag to rotate the femur and knee into a true AP projection. The knee is usually draped free with a sterile tourniquet and partially flexed over a radiolucent support (Fig. 4).
The knee is usually draped free with a sterile tourniquet and partially flexed over a radiolucent support (Fig. 4).Portals/Exposures
• Preoperative planning will give a better understanding of the fracture, the exposure required, and the equipment necessary for reduction and fixation. This is especially true if a tibial tubercle osteotomy is anticipated.
 Most supracondylar fractures can be reduced and stabilized through a single lateral approach. The exceptions to this would be medial condyle fractures and extensively comminuted intra-articular fractures.
Most supracondylar fractures can be reduced and stabilized through a single lateral approach. The exceptions to this would be medial condyle fractures and extensively comminuted intra-articular fractures. Surgical technique should include careful soft tissue handling, indirect reduction where possible, anatomic articular reconstruction, and restoration of limb length, rotation, and alignment.
Surgical technique should include careful soft tissue handling, indirect reduction where possible, anatomic articular reconstruction, and restoration of limb length, rotation, and alignment. Bone grafts should be used where necessary, and stable fixation should be achieved to allow for early active rehabilitation.
Bone grafts should be used where necessary, and stable fixation should be achieved to allow for early active rehabilitation. For the single lateral approach, a straight lateral incision is made over the distal femur extending to the midpoint of the lateral condyle (Fig. 5A). The incision should stay anterior to the lateral collateral ligament.
For the single lateral approach, a straight lateral incision is made over the distal femur extending to the midpoint of the lateral condyle (Fig. 5A). The incision should stay anterior to the lateral collateral ligament.• Proximally the incision can be extended as high as necessary depending on the length of the fracture, reduction technique, and implant chosen (Fig. 5B). The proximal incision is completed after the articular reduction has been achieved if possible.
• Distally, the incision can be extended across the knee joint and then curved anteriorly to the lateral border of the tibial tubercle.
• The fascia lata is incised in line with the skin incision, and the anterior fibers of the iliotibial band are divided distally. The approach continues through the joint capsule and synovium, taking care to ligate the superior lateral geniculate artery and not damage the lateral meniscus.
• Next the vastus lateralis is elevated from the intermuscular septum and any perforating vessels are ligated (Fig. 6A and 6B). Only as much soft tissue is elevated as necessary for the reduction and fixation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree