PROCEDURE 21 Subtrochanteric Fractures: Plate Fixation
Indications
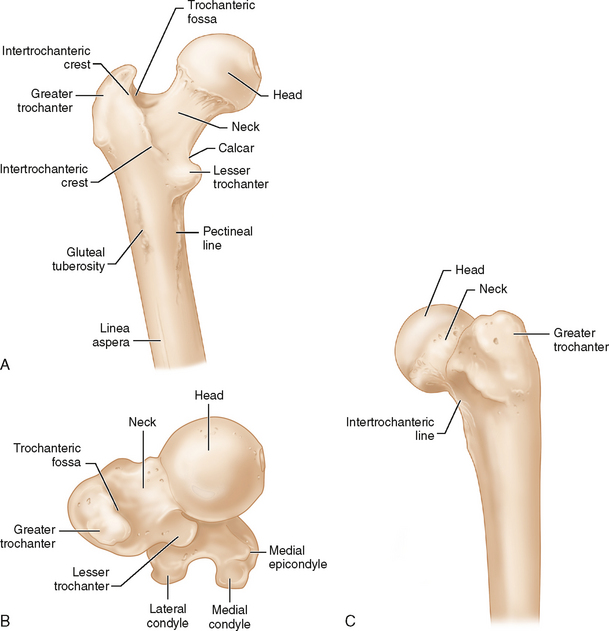
FRACTURE PATTERNS AND REPAIR OPTIONS
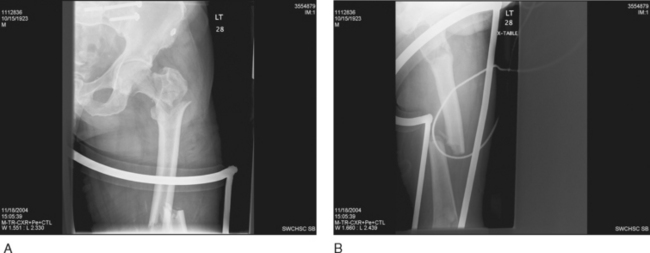
 Simple subtrochanteric fracture pattern (Fig. 2)
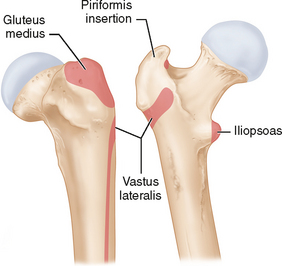
Simple subtrochanteric fracture pattern (Fig. 2)• Absolute stability via open reduction, lag screw fixation, plus compression or neutralization plating
 Base-of-neck and intertrochanteric fractures that extend into the subtrochanteric region
Base-of-neck and intertrochanteric fractures that extend into the subtrochanteric region• These fractures are considered separate from pure subtrochanteric fractures because the base of the femoral neck and the intertrochanteric region cannot be spanned or bridged using the usual techniques of relative stability.
• Sliding implants that allow dynamic compression across these areas must provide some limitation to sliding of the proximal fragment or excessive shaft medialization will occur because the normal trochanteric lateral buttress is usually compromised.
• Avoid bridge plating of simple metaphyseal and diaphyseal fracture patterns. Alternatives include:
 Simple fracture patterns can be treated with absolute stability using lag screw or compression plating techniques.
Simple fracture patterns can be treated with absolute stability using lag screw or compression plating techniques.
 Alternatively, simple fracture patterns can be treated with relative stability and a long working length (between proximal and distal screws) to minimize stress concentration. This can be achieved with an intramedullary nail or a long bridge plate, leaving plenty of space between screws proximal and distal to the fracture.
Alternatively, simple fracture patterns can be treated with relative stability and a long working length (between proximal and distal screws) to minimize stress concentration. This can be achieved with an intramedullary nail or a long bridge plate, leaving plenty of space between screws proximal and distal to the fracture.
 Simple fracture patterns can be treated with absolute stability using lag screw or compression plating techniques.
Simple fracture patterns can be treated with absolute stability using lag screw or compression plating techniques. Alternatively, simple fracture patterns can be treated with relative stability and a long working length (between proximal and distal screws) to minimize stress concentration. This can be achieved with an intramedullary nail or a long bridge plate, leaving plenty of space between screws proximal and distal to the fracture.
Alternatively, simple fracture patterns can be treated with relative stability and a long working length (between proximal and distal screws) to minimize stress concentration. This can be achieved with an intramedullary nail or a long bridge plate, leaving plenty of space between screws proximal and distal to the fracture.• Beware plating fracture patterns that are relatively simple but without medial calcar support.
 Plating requires either soft tissue stripping to facilitate absolute stability, with calcar reconstitution via open reduction and lag screw fixation, or minimally invasive fixed-angle bridge plating with a long working length. However, if the fracture pattern is relatively simple, it is difficult to avoid stress concentration with this technique (even if a long working length is used).
Plating requires either soft tissue stripping to facilitate absolute stability, with calcar reconstitution via open reduction and lag screw fixation, or minimally invasive fixed-angle bridge plating with a long working length. However, if the fracture pattern is relatively simple, it is difficult to avoid stress concentration with this technique (even if a long working length is used).
 Plating requires either soft tissue stripping to facilitate absolute stability, with calcar reconstitution via open reduction and lag screw fixation, or minimally invasive fixed-angle bridge plating with a long working length. However, if the fracture pattern is relatively simple, it is difficult to avoid stress concentration with this technique (even if a long working length is used).
Plating requires either soft tissue stripping to facilitate absolute stability, with calcar reconstitution via open reduction and lag screw fixation, or minimally invasive fixed-angle bridge plating with a long working length. However, if the fracture pattern is relatively simple, it is difficult to avoid stress concentration with this technique (even if a long working length is used).NAILING VERSUS PLATING
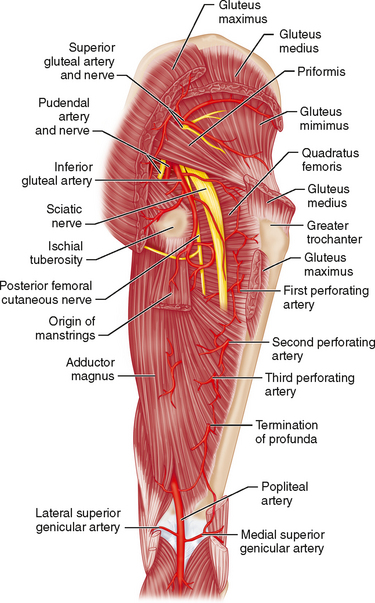
 Biomechanically, a round nail resists bending in all directions, whereas the laterally positioned plate is weakest in resisting varus forces.
Biomechanically, a round nail resists bending in all directions, whereas the laterally positioned plate is weakest in resisting varus forces. In osteoporotic bone, screw fixation (which is essential for successful plating) is suboptimal. Locking plate/screws and bone augmentation with cement or bone substitute can help with screw purchase.
In osteoporotic bone, screw fixation (which is essential for successful plating) is suboptimal. Locking plate/screws and bone augmentation with cement or bone substitute can help with screw purchase. The nail position in the canal, versus the lateral plate position, provides a small biomechanical advantage due to a shorter distance from the body weight to the fulcrum (the nail or plate).
The nail position in the canal, versus the lateral plate position, provides a small biomechanical advantage due to a shorter distance from the body weight to the fulcrum (the nail or plate). When employing relative stability, long nails automatically provide for a long “working length” (the distance between the screws proximal and distal to a fracture) to span fractures. When using plates, it is important to similarly consider the working length between the screws closest to the fracture proximally and distally to minimize stress concentration and failure.
When employing relative stability, long nails automatically provide for a long “working length” (the distance between the screws proximal and distal to a fracture) to span fractures. When using plates, it is important to similarly consider the working length between the screws closest to the fracture proximally and distally to minimize stress concentration and failure.• Dynamic compression versus locked anatomic fixation for complex proximal femoral fractures in the neck or intertrochanteric region with subtrochanteric extension
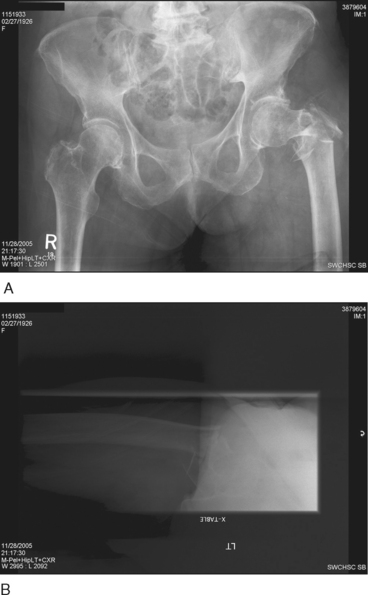
 Dynamic compression via sliding screw/plate implants results in malunion. However, nonsliding devices result in stress risers and possible nonunion with implant failure or screw penetration into the hip joint.
Dynamic compression via sliding screw/plate implants results in malunion. However, nonsliding devices result in stress risers and possible nonunion with implant failure or screw penetration into the hip joint.
 Dynamic compression via sliding screw/plate implants results in malunion. However, nonsliding devices result in stress risers and possible nonunion with implant failure or screw penetration into the hip joint.
Dynamic compression via sliding screw/plate implants results in malunion. However, nonsliding devices result in stress risers and possible nonunion with implant failure or screw penetration into the hip joint.• Immediate total hip replacement for complex proximal femoral fractures
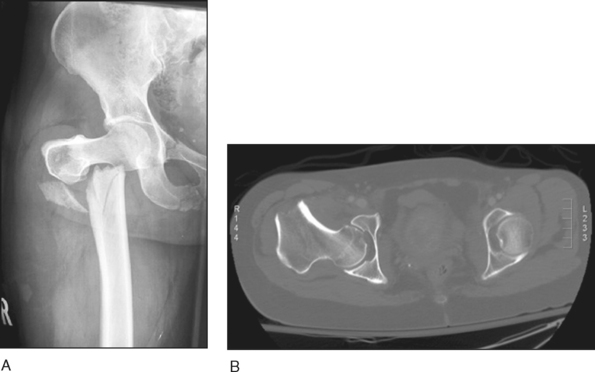
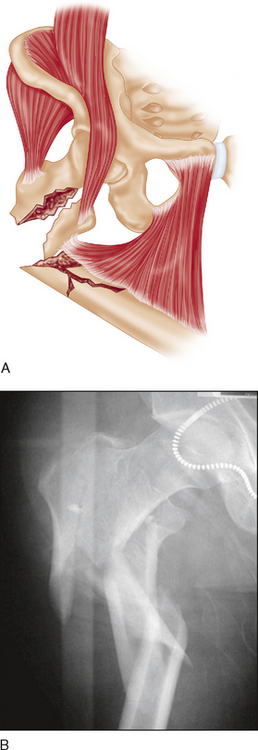
 In certain complex proximal femoral fractures involving poor-quality bone, such as the very comminuted proximal femoral fracture in an elderly osteopenic patient shown in Figure 4, total hip replacement may be an option.
In certain complex proximal femoral fractures involving poor-quality bone, such as the very comminuted proximal femoral fracture in an elderly osteopenic patient shown in Figure 4, total hip replacement may be an option.
 In certain complex proximal femoral fractures involving poor-quality bone, such as the very comminuted proximal femoral fracture in an elderly osteopenic patient shown in Figure 4, total hip replacement may be an option.
In certain complex proximal femoral fractures involving poor-quality bone, such as the very comminuted proximal femoral fracture in an elderly osteopenic patient shown in Figure 4, total hip replacement may be an option.• Note the anterior bow of the femur on a full-length lateral radiograph.
 A marked anterior femoral bow is common in the elderly and could result in a long plate sitting off the femur over a portion of its length. Care must be taken to ensure that the plate can be secured to the bone proximally and distally.
A marked anterior femoral bow is common in the elderly and could result in a long plate sitting off the femur over a portion of its length. Care must be taken to ensure that the plate can be secured to the bone proximally and distally.
 A marked anterior femoral bow is common in the elderly and could result in a long plate sitting off the femur over a portion of its length. Care must be taken to ensure that the plate can be secured to the bone proximally and distally.
A marked anterior femoral bow is common in the elderly and could result in a long plate sitting off the femur over a portion of its length. Care must be taken to ensure that the plate can be secured to the bone proximally and distally.Examination/Imaging
 Physical examination
Physical examination• Poor soft tissues, degloving injuries, and open wounds: may require a modification of the approach and implants chosen
 A plain anteroposterior (AP) radiograph of the pelvis enables comparison with the opposite side (especially useful for complex proximal femoral fractures of the intertrochanteric region or base of neck region).
A plain anteroposterior (AP) radiograph of the pelvis enables comparison with the opposite side (especially useful for complex proximal femoral fractures of the intertrochanteric region or base of neck region). Plain full-length AP and lateral radiographs of the femur, including the hip and knee joints, should be obtained.
Plain full-length AP and lateral radiographs of the femur, including the hip and knee joints, should be obtained. Rarely, computed tomography can be useful to identify the precise nature of the fracture pattern in the trochanteric region. For example, involvement of the piriformis fossa requires special techniques when performing piriformis start point nailing.
Rarely, computed tomography can be useful to identify the precise nature of the fracture pattern in the trochanteric region. For example, involvement of the piriformis fossa requires special techniques when performing piriformis start point nailing.Positioning
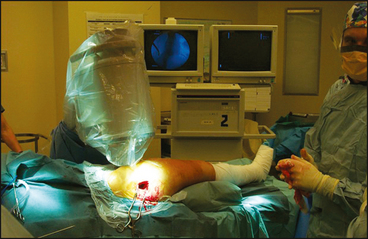
 Lateral versus supine position
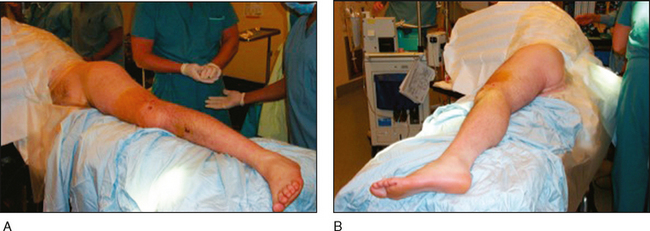
Lateral versus supine position• The lateral position is often preferred as it greatly facilitates reduction by moving the distal segment when an intact iliopsoas insertion results in flexion of the proximal fragment (Fig. 11).
• Comparing length and rotation to the other limb is difficult in the lateral position. However, the amount of rotation (in degrees) of the injured limb can readily be determined in the lateral position (see Procedure Step 1).
• When using the lateral position, the length of the intact leg should be determined before positioning. Options to measure the intact side include: