PROCEDURE 17 Femoral Neck Fractures
Indications
 Displaced fractures in individuals 65–75 years of age with good bone density and high functional demands
Displaced fractures in individuals 65–75 years of age with good bone density and high functional demands• Nonoperative management in the form of bed rest with early bed-to-chair mobilization may be utilized in elderly individuals in whom an unacceptably high risk of perioperative complications exists or in nonambulatory patients with minimal pain. It should be avoided whenever possible due to multiple, well-recognized complications.
• Internal fixation may take the form of cannulated screws or fixed-angle devices, most commonly a sliding hip screw. Fixed-angle devices may be preferred in fractures with more vertical orientation and basicervical fractures.
• Hemiarthroplasty or total hip arthroplasty tends to be standard treatment for patients 75 years of age or greater and may be considered in individuals with premorbid degenerative joint disease or in low-demand patients 65–75 years old with displaced fractures in whom a high risk of osteonecrosis exists.
Examination/Imaging
 Clinical diagnosis of a hip fracture is usually obvious in elderly individuals with a history of low-energy trauma.
Clinical diagnosis of a hip fracture is usually obvious in elderly individuals with a history of low-energy trauma.• Patients typically complain of groin pain and may hold the affected extremity in a position of flexion and external rotation. Shortening of the injured leg is usually present.
 Palpation of the greater trochanter and pubic rami may elicit tenderness and can provide clues as to the nature of injury (intertrochanteric vs. femoral neck fracture) and associated injuries (pubic rami fractures).
Palpation of the greater trochanter and pubic rami may elicit tenderness and can provide clues as to the nature of injury (intertrochanteric vs. femoral neck fracture) and associated injuries (pubic rami fractures). Elderly individuals with a femoral neck fracture due to a low-energy fall should have a thorough head-to-toe examination. In addition, appropriate laboratory and radiographic investigations should be ordered to rule out any underlying causes of the trauma (e.g., transient ischemic attack/cerebrovascular accident, congestive heart failure, myocardial infarction) as well as any associated injuries, such as subdural hematoma and ipsilateral upper extremity injury.
Elderly individuals with a femoral neck fracture due to a low-energy fall should have a thorough head-to-toe examination. In addition, appropriate laboratory and radiographic investigations should be ordered to rule out any underlying causes of the trauma (e.g., transient ischemic attack/cerebrovascular accident, congestive heart failure, myocardial infarction) as well as any associated injuries, such as subdural hematoma and ipsilateral upper extremity injury. Young individuals with hip fractures due to high-energy trauma should be assessed and resuscitated according to Advanced Trauma Life Support guidelines.
Young individuals with hip fractures due to high-energy trauma should be assessed and resuscitated according to Advanced Trauma Life Support guidelines. Plain radiographs
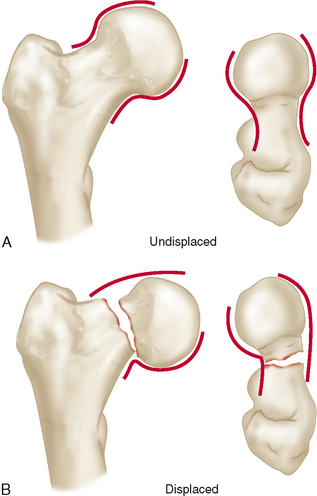
Plain radiographs• Standard imaging includes anteroposterior (AP) views of the hip (in 15° of internal rotation if possible) (Fig. 1A) and pelvis with a shoot-through lateral view of the affected hip (Fig. 1B).
• The images should be evaluated for impaction, displacement, and posterior comminution (best appreciated on the lateral) as well as for signs of degenerative joint disease (i.e., joint space narrowing, osteophytes, subchondral cysts, or sclerosis) and associated pelvic ring injuries. Comparison with the contralateral hip may allow detection of subtle impaction or displacement.
 Technetium bone scan
Technetium bone scan• A bone scan is used to diagnose occult femoral neck fractures in individuals with negative plain radiographs in whom suspicion of a femoral neck fracture remains high.
 Computed tomography (CT)
Computed tomography (CT)• CT may be used in the diagnosis of femoral neck fractures and is often already available in individuals involved in high-energy trauma who have undergone CT scanning of the pelvis (Fig. 2A and 2B).
 MRI
MRI• MRI is as accurate as radionuclide bone scanning in the diagnosis of occult femoral neck fracture, with increased sensitivity when performed in the first 24 hours following injury (Rizzo et al., 1993).
• It is useful in assessing for other causes of hip pain, including osteonecrosis, stress fracture, and neoplasia, in individuals with an atypical presentation.
Surgical Anatomy
 Improved outcomes in the treatment of femoral neck fractures can be attained with a thorough understanding of bony anatomy and vascular supply of the proximal femur. Perioperative decision making based on this information can ensure fracture treatment using the most appropriate method. This can help lead to avoidance of the complications most commonly seen with this injury.
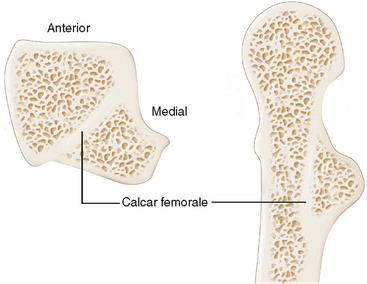
Improved outcomes in the treatment of femoral neck fractures can be attained with a thorough understanding of bony anatomy and vascular supply of the proximal femur. Perioperative decision making based on this information can ensure fracture treatment using the most appropriate method. This can help lead to avoidance of the complications most commonly seen with this injury. Osseous anatomy
Osseous anatomy• When viewed from the lateral side, the femoral neck lies anterior to the midaxis of the proximal femur due to a large posterior overhang of the greater trochanter. This must be kept in mind when inserting fixation devices to avoid posterior penetration of the femoral neck.
• The calcar femorale is a dense, vertical plate of bone arising from the cortex under the lesser trochanter in the posteromedial femur and projecting laterally to the greater trochanter (Fig. 3). It is thicker medially than laterally and is the site of origin of strong internal trabeculations that support the weight-bearing dome of the femoral head. The calcar femorale acts to reinforce the posteroinferior femoral neck, and unrecognized comminution of this region may lead to failure of fixation.
 Vascular anatomy
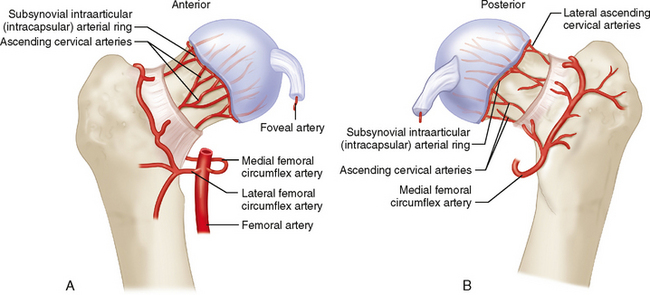
Vascular anatomy• The arterial supply of the femoral neck and head consists of:
♦ An extracapsular arterial ring at the base of the femoral neck formed by braches of the medial and lateral femoral circumflex arteries.
♦ Branches of the extracapsular arterial ring ascending on the femoral neck—the retinacular vessels—of which the lateral group are most important.
• Intracapsular anastomosis of the retinacular vessels occurs to form the subsynovial intracapsular arterial ring, which sends branches—the epiphyseal arteries—into the femoral head. The lateral epiphyseal artery, which is the terminal branch of the medial femoral circumflex artery, has been shown to supply the majority of the femoral head.
• A well-leg holder is required to position the unaffected extremity out of the fluoroscopy field. Alternatively, the uninjured extremity may be placed in wide abduction attached to a boot on the second leg extension of the fracture table.
Positioning
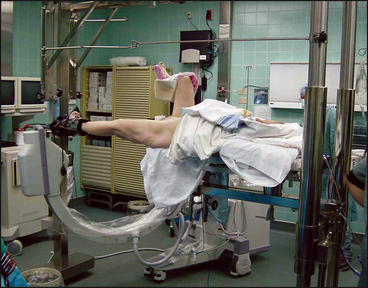
 Internal fixation of femoral neck fractures is performed in the supine position on a fracture table regardless of the fixation method chosen: multiple parallel screws or a sliding hip screw.
Internal fixation of femoral neck fractures is performed in the supine position on a fracture table regardless of the fixation method chosen: multiple parallel screws or a sliding hip screw. After induction of regional or general anesthesia and insertion of a Foley catheter, the patient is transferred to the fracture table.
After induction of regional or general anesthesia and insertion of a Foley catheter, the patient is transferred to the fracture table. After placement of a well-padded countertraction post, the unaffected leg is placed in a well-leg holder at 90° of flexion and mild abduction to facilitate positioning for fluoroscopy. Bony prominences, especially the fibular head with the closely associated peroneal nerve, should be well padded (Fig. 5).
After placement of a well-padded countertraction post, the unaffected leg is placed in a well-leg holder at 90° of flexion and mild abduction to facilitate positioning for fluoroscopy. Bony prominences, especially the fibular head with the closely associated peroneal nerve, should be well padded (Fig. 5). The fluoroscopy unit is now positioned as necessary to ensure that proper AP and lateral images of the affected hip may be obtained.
The fluoroscopy unit is now positioned as necessary to ensure that proper AP and lateral images of the affected hip may be obtained. If the fracture is displaced, closed reduction is now performed.
If the fracture is displaced, closed reduction is now performed.• Many femoral neck fractures can be reduced using the method of Whitman.
♦ The affected leg is secured in a well-padded boot in neutral position with gentle traction applied by the fracture table. The leg is gently abducted and internally rotated while viewing the reduction under image intensification. The medial spike of the femoral head should be supported by the calcar femorale.
♦ Reduction of the fracture is confirmed by restoration of the normal S-shaped curves of the cortex formed by the concave femoral neck and convex femoral head (Fig. 6). A varus reduction should not be accepted due to increased rates of failure of fixation (Chua et al., 1998).
• If closed reduction in extension is not successful, a single attempt in flexion should be carried out.
♦ The affected hip is flexed to 90° and, with slight internal rotation, traction is applied in line with the femur. Next, the internal rotation is maintained as the leg is circumducted into abduction and brought into extension.
 The affected hip is then prepped using antiseptic solution and the surgical field squared off with towels. A vertical, transparent sterile drape with an adhesive region for application over the incision site is then applied. The fluoroscopy unit is thus excluded from the sterile field (Fig. 7).
The affected hip is then prepped using antiseptic solution and the surgical field squared off with towels. A vertical, transparent sterile drape with an adhesive region for application over the incision site is then applied. The fluoroscopy unit is thus excluded from the sterile field (Fig. 7).