PROCEDURE 15 Scaphoid Fracture Fixation
Indications
 Displaced scaphoid fractures (1-mm gap visible on radiographs) should be treated with open reduction and internal fixation.
Displaced scaphoid fractures (1-mm gap visible on radiographs) should be treated with open reduction and internal fixation.• Extra-articular minimally displaced fractures do not necessarily need open reduction and internal fixation.
• Reduction of the cartilage, or the perimeter of the scaphoid, is more important than bone apposition.
Examination/Imaging
 Physical examination of the anatomical snuff-box without ulnar deviation of the wrist can be misleading.
Physical examination of the anatomical snuff-box without ulnar deviation of the wrist can be misleading. Radiographs at the time of injury should include a maximally ulnar-deviated posteroanterior (PA) view in order to rule out fracture.
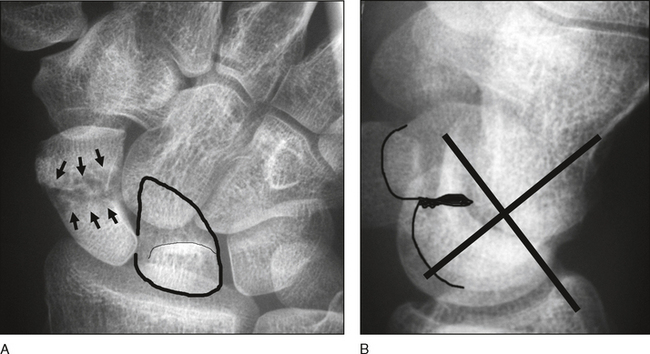
Radiographs at the time of injury should include a maximally ulnar-deviated posteroanterior (PA) view in order to rule out fracture.• Figure 1 shows radiographs of a scaphoid waist fracture with delayed union. There is shortening of the scaphoid on the PA view with an obvious cyst (Fig. 1A, arrows). The lunate is triangular in shape (outlined area) as it has slipped into a dorsal intercalated segment instability (DISI) position.
• On a lateral view (Fig. 1B), the lunate is tilted into DISI and the scapholunate angle is about 90°. There is a pronounced humpback deformity of the scaphoid itself (tracing outlining volar scaphoid) where the scaphoid has effectively folded into the cyst (large black void). This type of delayed union needs structural bone grafting from the volar side. A large iliac crest graft may be needed. Computed tomography (CT) scans are more helpful in this problem (see Fig. 5).
 Repeat radiographs at 1 week must be ordered with any suspected radial-sided wrist pain.
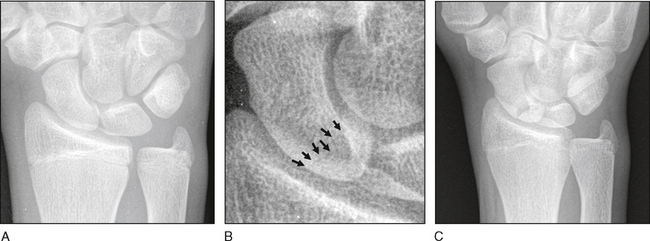
Repeat radiographs at 1 week must be ordered with any suspected radial-sided wrist pain.• Figure 2A and 2B are initial radiographs in an 18-year-old male that were read as negative by radiology. Small arrows in Figure 2B show a fracture line in the proximal pole that was missed. Repeat radiographs should have been scheduled but were not done.
• Follow-up at 4 months for the same patient (Fig. 2C) shows obvious nonunion with cyst formation. Splint use might have prevented this complication.
 CT scan or magnetic resonance imaging (MRI) will reliably rule out most fractures at initial presentation.
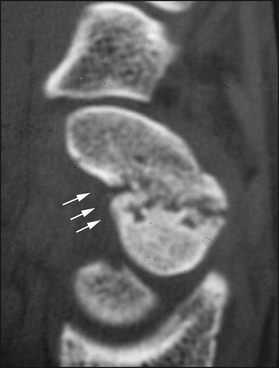
CT scan or magnetic resonance imaging (MRI) will reliably rule out most fractures at initial presentation.• Figure 3 shows a CT scan of a scaphoid nonunion. There is a loss of volar scaphoid bone stock secondary to cyst formation (arrows). Sclerosis is seen at the fracture ends.
• Obvious increase in the intrascaphoid angle is easily seen on a sagittal CT scan (Fig. 4, angle). As for the delayed union shown in Figure 1, this is a structural problem necessitating a large graft. The sclerotic ends must be removed in order to facilitate invagination of a graft to allow reconstitution of scaphoid length.
• The MRI in Figure 5 shows a waist fracture of the scaphoid. Signal changes on this coronal view show obvious vascularity loss (arrowhead). Change in vascularity of the proximal pole secondary to the fracture and the distal blood supply result in an avascular proximal pole.
♦ Use of a vascularized graft in waist fractures is controversial. The avascular proximal pole will heal to the distal scaphoid if solid internal fixation with a screw orthogonal to the fracture line is accomplished.
 Bone scan may be used if more than 48 hours have passed since injury, and is a sensitive but not specific test.
Bone scan may be used if more than 48 hours have passed since injury, and is a sensitive but not specific test.Surgical Anatomy
Portals/Exposures
 Volar approaches are used for larger defects, humpback deformities, combined volar ligament repairs, and fractures distal or at the waist.
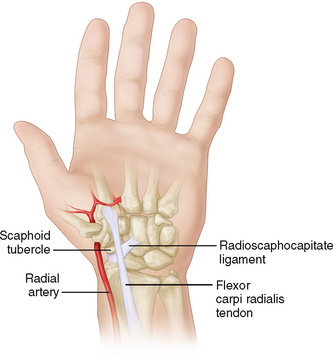
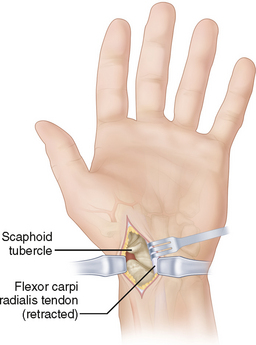
Volar approaches are used for larger defects, humpback deformities, combined volar ligament repairs, and fractures distal or at the waist.• A 3-cm incision is centered over the scaphoid tubercle, extending from the distal aspect of the FCR tendon and then curving toward the base of the thenar mass (Fig. 8).
• The FCR tendon sheath is incised, the FCR tendon is retracted ulnarly, and the dorsal sheath is then incised.
• A longitudinal arthrotomy is made in the radiocarpal joint, curving transversely to open the STT joint.
 Dorsal approaches are used for proximal fractures and dorsal revascularization procedures.
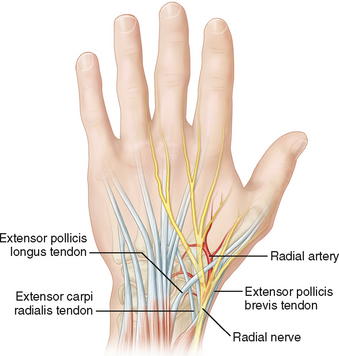
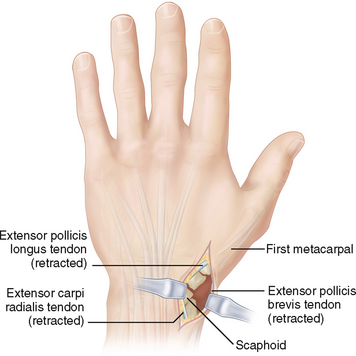
Dorsal approaches are used for proximal fractures and dorsal revascularization procedures.• A 3-cm curvilinear incision is centered over the anatomical snuff-box, extending from the base of the first metacarpal to 2 cm proximal to the snuff-box (Fig. 9).
• The EPL and EPB tendons are identified. The fascia between the two tendons is incised and the tendons are retracted.
 Percutaneous fluoroscopy-guided volar and dorsal approaches have been described for fractures in the same location that do not need bone grafts and are easily anatomically reducible without an open reduction being required.
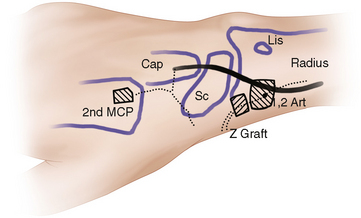
Percutaneous fluoroscopy-guided volar and dorsal approaches have been described for fractures in the same location that do not need bone grafts and are easily anatomically reducible without an open reduction being required. Combined volar-dorsal approaches may be used for vascularized grafting of humpback deformities (see Fig. 17) or percutaneous fixation of proximal fractures when a distal screw is desirable.
Combined volar-dorsal approaches may be used for vascularized grafting of humpback deformities (see Fig. 17) or percutaneous fixation of proximal fractures when a distal screw is desirable.• Kirschner wires can be used for segmental, comminuted fractures where compression would cause malunion.
• Small modular hand screws can be used in combination with other compression devices for more complicated fractures. However, they may not be strong enough when used alone with intercalary grafting. In Figure 10, broken hardware is evident after use of small screws to fix a large intercalary graft. Slow healing associated with this large graft probably resulted in fixation failure. A more robust screw should be used, especially if bone healing is expected at both ends of a large graft.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree