PROCEDURE 14 Distal Radius Fractures
Open Reduction and Internal Fixation
• Although volar fixation has become increasingly popular, reports of the complications of volar plates are beginning to appear in the literature
• Specific equipment and reduction choices must be made available within the capabilities of the operating surgeon to allow for customization of fixation to fracture type.
Indications
INTRA-ARTICULAR FRACTURES
• A wide array of fixation option and approaches are available such that almost all distal radius fractures can be treated with open reduction and internal fixation (ORIF). Whether this is always necessary or preferable and can be reliably accomplished with good functional outcome is still open to debate until appropriately powered, well-designed studies are completed.
• In terms of volar locking plates, many systems exists with various design features such as multiple rows of distal fixation, availability of locking screw versus locking smooth peg option, and different direction and number of distal locking screws. However, to date, no one volar locking plate has been shown to be consistently superior to other volar locking plate designs.
 Type B fractures
Type B fractures• Dorsal
♦ If closed reduction and percutaneous pinning cannot be attained, a volar fixed-angle locking plate can be used.
♦ Volar treatment of dorsal lip fractures requires secure purchase into the distal fragment and use of distally inclined locking screws to provide subchondral support of the dorsal articular surface.
 Type C fractures
Type C fractures• Lunate fossa
♦ A volar fixed-angle locking plate or polyaxial locking plate is used to provide adequate subchondral support to each of the common intra-articular fracture fragments. If comminution necessitates dorsal reduction, then a fragment-specific plate is used as well.
• Lunate fossa split and displaced
♦ A volar fixed-angle locking plate or polyaxial locking plate is used to provide adequate subchondral support to each of the common intra-articular fracture fragments.
• Comminuted (type C2/C3)
♦ An extended volar fixed-angle locking plate is used, with or without a dorsal plate(s) in a fragment-specific manner.
Examination/Imaging
 All displaced intra-articular fractures should be imaged with computed tomography (CT) scanning in order to determine specific fragment position and displacement.
All displaced intra-articular fractures should be imaged with computed tomography (CT) scanning in order to determine specific fragment position and displacement. Intraoperative images must include anteroposterior (AP) (or posteroanterior) and lateral views as well as a 30° styloid view to ensure that screws placed subchondrally are not in the lunate fossa or scaphoid fossa.
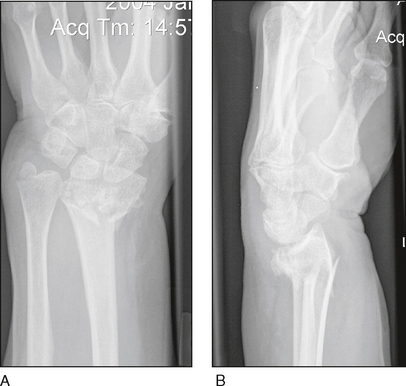
Intraoperative images must include anteroposterior (AP) (or posteroanterior) and lateral views as well as a 30° styloid view to ensure that screws placed subchondrally are not in the lunate fossa or scaphoid fossa.• Figure 1A shows an AP radiograph of a displaced distal radius fracture. An associated styloid fracture may or may not convey instability. An intraoperative stress test of the distal ulna may indicate if fixation of the styloid area is needed. Although this AP image is consistent with a typical extra-articular fracture known as Colles’ fracture, the lateral view shows comminution of the dorsal cortex extending to the joint line (see Fig. 1B). This is a bad prognostic sign for redisplacement if not treated with stable fixation.
• In the lateral view (see Fig. 1B), dorsal tilt (and shortening) is obvious. Carpal instability pattern (CIA) is secondary to the distal radius angulation. Dorsal comminution is obvious. This amount of dorsal tilt and comminution denotes an unstable pattern, leading to a high rate of redisplacement with cast treatment alone.
 Multiple oblique lateral projections in varying degrees of pronation and supination may help visualize dorsal penetration of volar locking screws.
Multiple oblique lateral projections in varying degrees of pronation and supination may help visualize dorsal penetration of volar locking screws.Surgical Anatomy
 Volar surgical anatomy
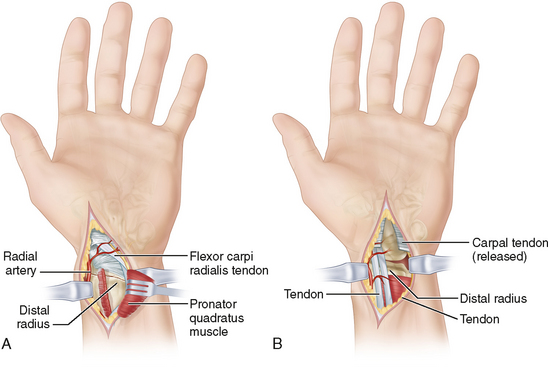
Volar surgical anatomy• A longitudinal incision is made over the distal aspect of the flexor carpi radialis (FCR) tendon. The volar aspect of the FCR sheath is incised and the FCR tendon is retracted ulnarly. The bed of the sheath is then incised longitudinally.
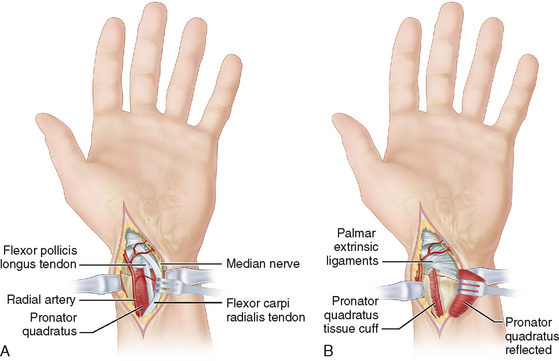
• The flexor pollicis longus (FPL) tendon lies just beneath the FCR sheath. Retraction of the FPL tendon ulnarly will reveal the deep layer of the palmar approach and hence the pronator quadratus (PQ) (Fig. 2A).
• The PQ is released sharply from the radius, leaving a small cuff of tissue radially. It is reflected back as an ulnar-based flap. Care must be taken not to detach the palmar extrinsic radiocarpal ligaments (Fig. 2B).
• The use of the FCR for the palmar approach keeps the radial artery safely out of the surgical plane just radial to the dissection (see Fig. 2).
• The palmar cutaneous branch of the median nerve is only at risk if the dissection strays to the ulnar side of the FCR (see Fig. 2).
• The approach allows for exposure of the entire volar distal radius and can be used for most fractures.
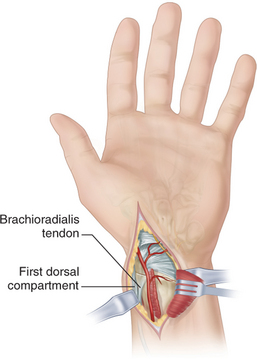
• Occasionally, particularly for fractures, treated in delayed fashion, dissection can be carried out radial to or below the radial artery, and a brachioradialis tenotomy can then be performed. The brachioradialis tenotomy will release one of the main deforming vectors on the fracture. Care must be taken to avoid injury to the first dorsal compartment during this radial dissection (Fig. 3).
 Dorsal surgical anatomy
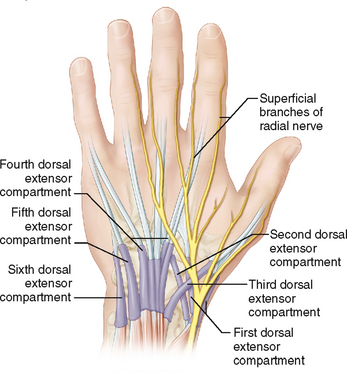
Dorsal surgical anatomy• A longitudinal incision is made just ulnar to Lister’s tubercle. The incision extends 2 cm distal and 3 cm proximal to Lister’s tubercle.
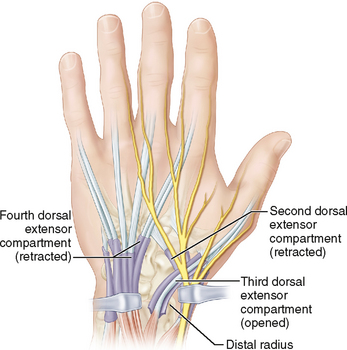
• The third extensor compartment and its content, the extensor pollicis longus (EPL), are identified beneath the extensor retinaculum just ulnar to Lister’s tubercle. Sharp dissection is used to release the EPL tendon in its entirety from the third compartment. Blunt dissection beneath the subcutaneous tissue of the radial-sided flap will avoid inadvertent injury to the dorsal branches of the superficial radial nerve (Fig. 4).
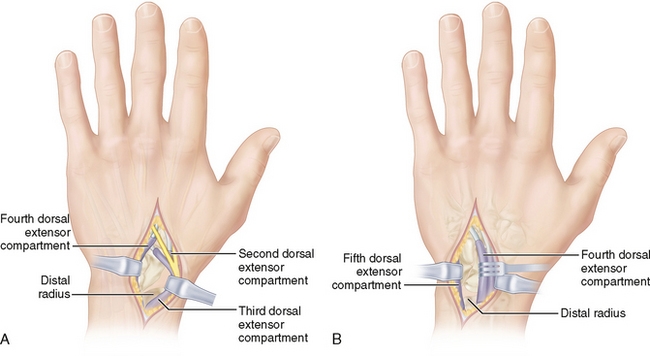
• A plane of dissection is established subperiosteally on the radius beneath the second and fourth extensor compartments to expose the entire dorsal aspect of the distal radius. The plane of dissection distally is established beneath the second and fourth compartments but superficial to the dorsal joint capsule.
• A transverse arthrotomy can be performed just distal to the dorsal rim of the radius to allow for accurate intra-articular reduction under direct visualization (Fig. 5).
Positioning
• Finger traps applied to the index and middle fingers, with 4.5 kg of longitudinal traction applied through a rope and pulley system (see Fig. 6), can facilitate reduction of the fracture and decrease the need for an assistant.
 The patient is positioned supine with the involved extremity draped free and centered on a radiolucent hand table (Fig. 6). A weight system with sterile rope is seen projecting from the end of the hand table in Figure 6; this aids in some complex fractures.
The patient is positioned supine with the involved extremity draped free and centered on a radiolucent hand table (Fig. 6). A weight system with sterile rope is seen projecting from the end of the hand table in Figure 6; this aids in some complex fractures. The table is set up to allow frequent radiographic evaluation. A mobile C-arm is used for every case.
The table is set up to allow frequent radiographic evaluation. A mobile C-arm is used for every case. A tourniquet is placed around the upper arm. One or two towels rolled and held in place with a plastic sticky drape are useful to position the wrist and hand on.
A tourniquet is placed around the upper arm. One or two towels rolled and held in place with a plastic sticky drape are useful to position the wrist and hand on.Portals/Exposures
 Volar FCR approach (Fig. 7A)
Volar FCR approach (Fig. 7A)• The volar and dorsal sheaths of the FCR tendon are incised. The radial artery is retracted toward the radial side. The FCR tendon is retracted ulnarly, thereby protecting the palmar cutaneous branch of the median nerve and the median nerve proper.
 Universal volar carpal tunnel approach (Fig. 7B)
Universal volar carpal tunnel approach (Fig. 7B)• This approach allows for simultaneous release of the carpal tunnel as well as excellent exposure of the ulnar side of the radius.
 Dorsal 3-4 approach (Fig. 8A)
Dorsal 3-4 approach (Fig. 8A)• This is the standard dorsal approach. It is performed through the third dorsal extensor (EPL) compartment. Then the interval between the second and fourth extensor compartments is used to expose the entire distal radius.
• The dorsal ligaments may be released in order to visualize the radiocarpal joint and verify the intra-articular reduction and congruity.
Procedure: Volar Fixed-Angle Locking Plate for Extra-Articular Fractures
STEP 1: CLOSED REDUCTION MANEUVER OF AGEE
 Longitudinal traction is first used to restore length and to assess the benefit of ligamentotaxis for the restoration of articular stepoff. This procedure is used for type A fractures such as that shown in Figure 9A and 9B.
Longitudinal traction is first used to restore length and to assess the benefit of ligamentotaxis for the restoration of articular stepoff. This procedure is used for type A fractures such as that shown in Figure 9A and 9B. Next, the hand is translated palmarly relative to the forearm to restore sagittal tilt and to assess the integrity of the volar lip of the radius.
Next, the hand is translated palmarly relative to the forearm to restore sagittal tilt and to assess the integrity of the volar lip of the radius. Finally, pronation of the hand relative to the forearm is performed in order to correct the supination deformity.
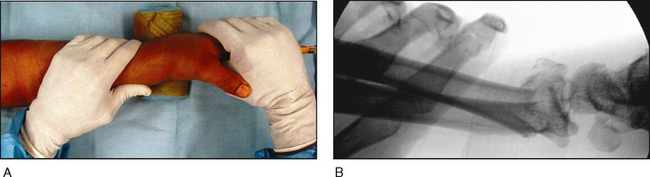
Finally, pronation of the hand relative to the forearm is performed in order to correct the supination deformity. Figure 10 shows the clinical (Fig. 10A) and radiographic (Fig. 10B) outcome of the Agee reduction maneuver.
Figure 10 shows the clinical (Fig. 10A) and radiographic (Fig. 10B) outcome of the Agee reduction maneuver.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree