PROCEDURE 13 Distal Radius Fractures
Indications
• If the goals of reduction cannot be obtained using external fixation (with or without augmentation), then the surgeon must be equipped to convert to an open procedure. This occurs in up to 10% of distal radius fractures.
 Spanning external fixation
Spanning external fixation• This technique can be used for most fractures of the distal radius that have failed an attempt at closed reduction, excluding volar displaced fracture patterns (Smith’s) and volar or dorsal shear patterns (Barton’s).
 Nonspanning external fixation
Nonspanning external fixation• This technique can be used for unstable extra-articular or minimally displaced articular distal radius fractures that have failed an attempt at closed reduction.
• It can also be used for severe intra-articular fractures where there is space for the distal pins after reduction of the intra-articular component.
• Nonspanning external fixation can be combined with distal radial osteotomy for the treatment of distal radius malunion.
Examination/Imaging
• Some authors prefer to avoid external fixation in patients with osteoporosis, while others advocate its use considering that all stabilization techniques are severely compromised in this population.
PHYSICAL EXAMINATION
 Treatment should be directed according to patient’s functional status, occupational requirements, hand dominance, pertinent medical history, and expectations.
Treatment should be directed according to patient’s functional status, occupational requirements, hand dominance, pertinent medical history, and expectations. Examination should focus on identifying other systemic or upper extremity injuries. After diagnosing, prioritizing, and treating systemic injuries, the limb needs to be assessed.
Examination should focus on identifying other systemic or upper extremity injuries. After diagnosing, prioritizing, and treating systemic injuries, the limb needs to be assessed.• It is essential to examine the forearm and elbow as well as the carpus. Galeazzi, Monteggia, and Essex-Lopresti lesions are often missed in the forearm, while carpal ligament injuries are often missed in the hand (Fig. 1).
• The limb must be inspected for open wounds. They are generally low grade and occur on the volar surface of the wrist or occasionally on the ulnar side of the wrist when associated with an ulnar styloid fracture).
• A careful neurologic examination must rule out neurologic insult. This most commonly occurs in the median nerve and may require an urgent decompression if a severe or progressive neurologic deficit is found.
• Most distal radius fractures considered for surgery should have failed an attempted closed reduction. Exceptions include open fractures, polytrauma, ipsilateral upper extremity injuries, and associated neurologic insult requiring surgery.
• Many treatment options exist for the distal radius fracture. Most can be used in isolation or in conjunction with external fixation. The general principle is to do what works well and is reproducible in your hands.
 A second reduction can be attempted, but the results are usually similar to the first attempt. It should only be attempted when at least one or more parameters have been changed to significantly increase the chances of success. Finger traps, deeper sedation, or more experienced physician and assistants may all increase chances of successful reduction.
A second reduction can be attempted, but the results are usually similar to the first attempt. It should only be attempted when at least one or more parameters have been changed to significantly increase the chances of success. Finger traps, deeper sedation, or more experienced physician and assistants may all increase chances of successful reduction.
 A second reduction can be attempted, but the results are usually similar to the first attempt. It should only be attempted when at least one or more parameters have been changed to significantly increase the chances of success. Finger traps, deeper sedation, or more experienced physician and assistants may all increase chances of successful reduction.
A second reduction can be attempted, but the results are usually similar to the first attempt. It should only be attempted when at least one or more parameters have been changed to significantly increase the chances of success. Finger traps, deeper sedation, or more experienced physician and assistants may all increase chances of successful reduction.IMAGING STUDIES
 Anteroposterior (AP), lateral, and oblique films should be obtained for initial assessment. The patient should be splinted for comfort prior to transport to the diagnostic imaging department.
Anteroposterior (AP), lateral, and oblique films should be obtained for initial assessment. The patient should be splinted for comfort prior to transport to the diagnostic imaging department. Repeating these films postreduction usually provides more information about the specific fracture fragments. Postreduction films should be obtained even if the decision to go to the operating room has already been made, such as for open fracture.
Repeating these films postreduction usually provides more information about the specific fracture fragments. Postreduction films should be obtained even if the decision to go to the operating room has already been made, such as for open fracture.• Radiographic parameters for acceptable reduction must be assessed preoperatively and repeatedly during surgery.
• Acceptable and normal values differ; these numbers should be intimately well known to the treating surgeon.
 Contralateral films can be obtained to assess the patient’s normal anatomy. This may be useful in assessing anatomic variants or judging radial length. This is not routinely done.
Contralateral films can be obtained to assess the patient’s normal anatomy. This may be useful in assessing anatomic variants or judging radial length. This is not routinely done. Traction films can add value in identifying specific fracture fragments. These are easily obtained in the operating room utilizing the image intensifier.
Traction films can add value in identifying specific fracture fragments. These are easily obtained in the operating room utilizing the image intensifier.• Figure 2 shows traction views of a 47-year-old female with an injury to her dominant arm; these were taken in the operating room prior to deciding on a definitive treatment plan. The fracture was deemed too comminuted for open fixation and therefore was treated with a spanning fixator in combination with a mini-open dorsal incision and supplementary Kirschner wires (K-wires). This example demonstrates the value of these views in understanding the fracture pattern.
 Computed tomography is occasionally indicated for distal radius fractures. If utilized, it provides the most information after a reduction maneuver is performed. It should be reserved for use when the surgeon is trying to determine the size, position and orientation of fracture fragments or fragment orientation.
Computed tomography is occasionally indicated for distal radius fractures. If utilized, it provides the most information after a reduction maneuver is performed. It should be reserved for use when the surgeon is trying to determine the size, position and orientation of fracture fragments or fragment orientation.Surgical Anatomy
 The bony anatomy of the distal radius must be intimately understood. If distal radial pins are used, this is paramount.
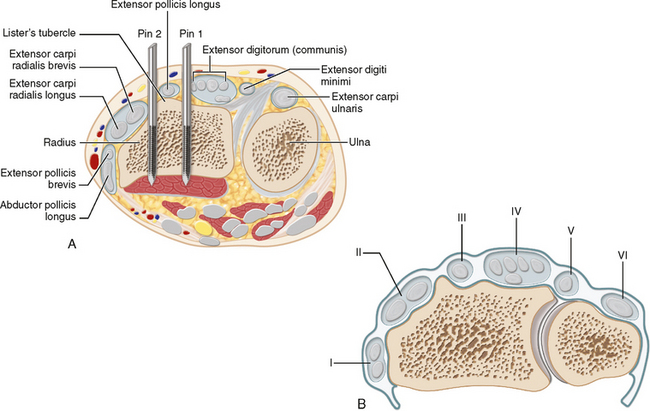
The bony anatomy of the distal radius must be intimately understood. If distal radial pins are used, this is paramount. The articular surface is a triangle with its base at the lunate facet and its apex the radial styloid. It slopes in an ulnar and volar direction (Fig. 3A).
The articular surface is a triangle with its base at the lunate facet and its apex the radial styloid. It slopes in an ulnar and volar direction (Fig. 3A). Lister’s tubercle sits dorsally and acts as a fulcrum for the EPL tendon, which passes on its ulnar side. This acts as a landmark to identify and protect the EPL for pin placement or mini-open procedures.
Lister’s tubercle sits dorsally and acts as a fulcrum for the EPL tendon, which passes on its ulnar side. This acts as a landmark to identify and protect the EPL for pin placement or mini-open procedures. The superficial branch of the radial nerve and its branches are at risk during proximal and distal fixator pin placement as well as during percutaneous K-wire placement from the radial styloid. Painful neuromata can cause significant morbidity postoperatively.
The superficial branch of the radial nerve and its branches are at risk during proximal and distal fixator pin placement as well as during percutaneous K-wire placement from the radial styloid. Painful neuromata can cause significant morbidity postoperatively. The dorsal-radial anatomy of the radius in the middle third must be well known for proximal fixator pin placement.
The dorsal-radial anatomy of the radius in the middle third must be well known for proximal fixator pin placement.• From radial to ulnar, the bone is covered by the flat tendons and musculotendinous junctions of the brachioradialis, extensor carpi radialis longus and brevis, and crossing abductor pollicis longus muscles.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree