PROCEDURE 10 Radial Head Arthroplasty
Introduction
 Most comminuted radial head fractures have been shown to occur in conjunction with other associated injuries around the elbow or wrist (Davidson et al., 1993; Itamura et al., 2005).
Most comminuted radial head fractures have been shown to occur in conjunction with other associated injuries around the elbow or wrist (Davidson et al., 1993; Itamura et al., 2005). This combination of injuries often makes the elbow more unstable; the radial head becomes an important elbow stabilizer in this scenario. Therefore, nonoperative treatment or a simple radial head resection for a comminuted radial head fracture is an uncommon treatment choice in this scenario.
This combination of injuries often makes the elbow more unstable; the radial head becomes an important elbow stabilizer in this scenario. Therefore, nonoperative treatment or a simple radial head resection for a comminuted radial head fracture is an uncommon treatment choice in this scenario. Open reduction and internal fixation or radial head arthroplasty remain the treatment choices for displaced and comminuted fractures.
Open reduction and internal fixation or radial head arthroplasty remain the treatment choices for displaced and comminuted fractures. Displaced, comminuted (Mason type 3) radial head fractures are better treated by arthroplasty than marginal fixation, even in the hands of experienced surgeons (Ring et al., 2002).
Displaced, comminuted (Mason type 3) radial head fractures are better treated by arthroplasty than marginal fixation, even in the hands of experienced surgeons (Ring et al., 2002).Indications
 The indications for radial head arthroplasty include a comminuted, unreconstructible radial head fracture with:
The indications for radial head arthroplasty include a comminuted, unreconstructible radial head fracture with:• Associated fracture of the of the coronoid (terrible triad injury) (Pugh et al., 2004) (Fig. 2A and 2B)
Examination/Imaging
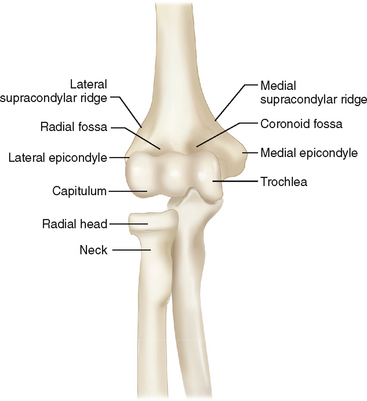
 Locations where the patient is tender—medial epicondyle, lateral epicondyle, radial head, interosseous membrane, distal radioulnar joint—are noted.
Locations where the patient is tender—medial epicondyle, lateral epicondyle, radial head, interosseous membrane, distal radioulnar joint—are noted. Stable range of motion (ROM) is documented in supination, neutral, and pronation. ROM/stability testing may be most accurate after administration of a general anesthetic.
Stable range of motion (ROM) is documented in supination, neutral, and pronation. ROM/stability testing may be most accurate after administration of a general anesthetic. Preoperative neurovascular status is documented thoroughly, with special attention to the posterior interosseous nerve.
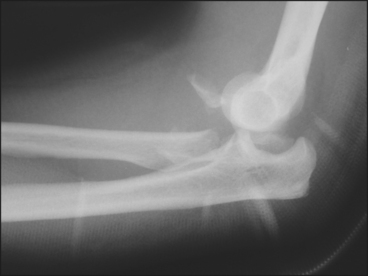
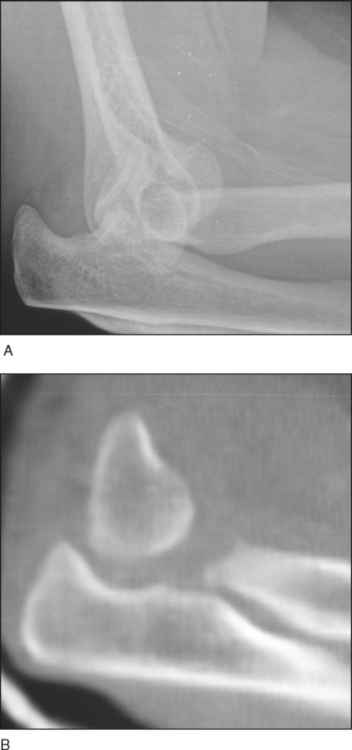
Preoperative neurovascular status is documented thoroughly, with special attention to the posterior interosseous nerve. Radiographic imaging includes high-quality anteroposterior (AP)/lateral radiographs of the elbow (Fig. 4A and 4B).
Radiographic imaging includes high-quality anteroposterior (AP)/lateral radiographs of the elbow (Fig. 4A and 4B). Preoperative fluoroscopy (after general anesthetic), including AP/lateral and moving fluoroscopic examination, can be helpful.
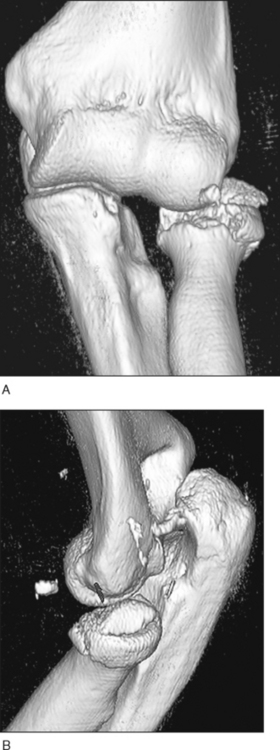
Preoperative fluoroscopy (after general anesthetic), including AP/lateral and moving fluoroscopic examination, can be helpful. Computed tomography can be helpful (but is not mandatory) preoperatively to understand and plan the surgery; usually two- or three-dimensional reconstuctions are the most informative (Fig. 5A and 5B).
Computed tomography can be helpful (but is not mandatory) preoperatively to understand and plan the surgery; usually two- or three-dimensional reconstuctions are the most informative (Fig. 5A and 5B).Surgical Anatomy
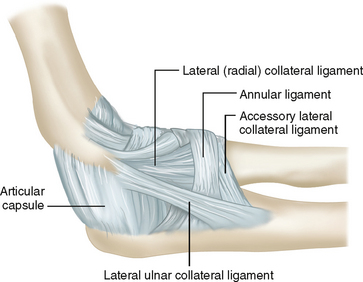
 Neurovascular structures
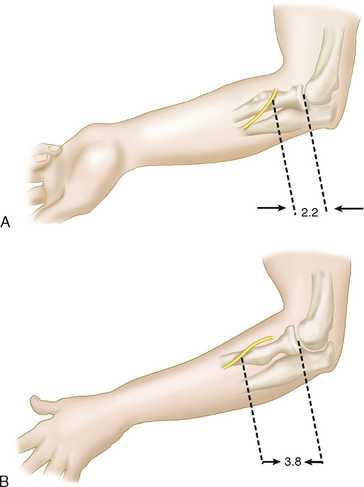
Neurovascular structures• The posterior interosseous nerve is in close proximity to the radial neck (Diliberti et al., 2000) (Fig. 9A and 9B).
Positioning
• Using a popliteal post allows the arm to hang freely, but taping of pillows and then sterile rolls allows the same arm position and easier intraoperative fluoroscopic examination.
• Since most dislocations are posterior, in the lateral decubitus position, gravity helps to reduce the elbow (Fig. 11).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree