Non-Inflammatory Joint and Soft Tissue Disorders
1Atlanta Veterans Affairs Medical Center, Atlanta, GA, USA
2Rheumatology and Internal Medicine, Chen Medical Centers, Miami, FL, USA
3Emory University School of Medicine, Atlanta, GA, USA
Introduction
Rheumatologists often manage non-inflammatory arthritides and associated soft tissue disorders, including osteoarthritis, carpal tunnel syndrome, and gout. The diagnosis of these conditions as well as recent innovations in treatment will be reviewed here.
Carpal Tunnel Syndrome
Epidemiology
- One of the most common and frequently diagnosed entrapment neuropathies
- Accounts for up to 90% of entrapment neuropathies
- Prevalence in the US population up to 5% of the general population
- Estimated lifetime risk of 10%
- Females affected more frequently than men
- Peak age range 40–60 years
- Estimated lifetime risk of 10%
- Risk factors include prolonged wrist flexion or extension, repeated use of flexor muscles, and exposure to vibration
- Systemic medical conditions i.e. diabetes, hypothyroidism, obesity, pregnancy, vitamin toxicity or deficiency can predispose
- Many cases remain idiopathic
- Systemic medical conditions i.e. diabetes, hypothyroidism, obesity, pregnancy, vitamin toxicity or deficiency can predispose
- Accounts for up to 90% of entrapment neuropathies
Pathology
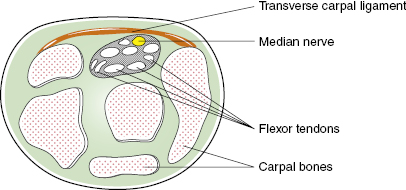
- Median nerve entrapment is caused by chronic pressure at the level of the carpal tunnel
- Compression of the median nerve is secondary to surrounding structures: carpal bones, flexor tendons, and the fibrous transverse carpal ligament leading to median nerve dysfunction
- Carpal tunnel anatomy (Figure 1.1)
- Superiorly: transverse carpal ligament
- Posteriorly: carpal bones
- Nine flexor tendons: (four) flexor digitorum profundus, (four) flexor digitorum superficialis, flexor pollicis
- Median nerve
- Superiorly: transverse carpal ligament
- Carpal tunnel anatomy (Figure 1.1)
- Repetitive compressive injury to the median nerve leads to demyelination
- Blood flow may also be interrupted, altering the blood–nerve barrier
Clinical Presentation
- Symptoms may include tingling and numbness, in the distribution of the median nerve (first three fingers and radial aspect of the fourth finger); pain involving the entire hand, decreased grip strength, and reduced dexterity
- Symptoms occasionally worse at night (awakenings with paresthetica nocturna: sensation of tingling, burning or numb hand possibly secondary to flexion of wrist at night)
- Patients with carpal tunnel syndrome (CTS) occasionally report subjective swelling of the hands and/or wrists
- Atrophy of the thenar eminence occurs in later stages (this finding is associated with poor response to surgical decompression)
Diagnosis
- Combination of the clinical history, examination, provocative tests, electrodiagnostic studies
- Phalen’s test is positive when flexion at the wrist for 60 seconds causes pain and/or paresthesias in median nerve distribution
- Sensitivity ranges from 67–83%
- Specificity ranges from 40–98%
- Sensitivity ranges from 67–83%
- Tinel’s test is positive when tapping over the volar surface of the wrist (course of median nerve) causes pain and/or paresthesias in the distribution of the median nerve
- Sensitivity ranges from 48–73%
- Specificity reported as high as 100%
- Sensitivity ranges from 48–73%
- Electrodiagnostic studies lack standardized diagnostic criteria currently, making them inadequate as a universally recognized gold standard
- Nerve conduction studies provide objective information regarding the median nerve across the carpal tunnel
- Findings include prolonged motor and sensory latencies of median nerve
- Reduction in median nerve compound motor or sensory action potential amplitude
- Reductions in sensory and motor conduction velocities
- Rules out other polyneuropathies included in the differential diagnosis
- Findings include prolonged motor and sensory latencies of median nerve
- Nerve conduction studies provide objective information regarding the median nerve across the carpal tunnel
- Ultrasonography may reveal flattening of the median nerve within the tunnel and bowing of the flexor retinaculum
- Cross-sectional area of the median nerve is the most predictive of CTS; it has also been used in the classification of the severity of CTS
- Magnetic resonance imaging assists in the determination of the severity of nerve compression; it is also helpful in observing anatomical structures that may be contributing to symptoms, i.e. ganglion cysts, bony deformities
- Swelling of the median nerve and increased signal intensity on T2- weighted images assist in diagnosing CTS
- Phalen’s test is positive when flexion at the wrist for 60 seconds causes pain and/or paresthesias in median nerve distribution
Treatment
- Mild to moderate symptoms
- Oral anti-inflammatories
- Oral corticosteroids may be effective in reducing edema and tenosynovitis associated with CTS
- Carpal bone mobilization and hand splints are often first-line treatment options
- Corticosteroid injection along the proximal wrist crease just ulnar to the palmaris longus tendon provides clinical improvement, however benefit beyond 1 month was not shown in a systematic review
- Ultrasound therapy
- Oral anti-inflammatories
- Moderate to severe symptoms
- Acupuncture therapy has been reported to improve median nerve function
- Carpal tunnel release (CTR)
- Surgical procedure to increase space in the carpal tunnel and reduce pressure on the median nerve, via division of the transverse carpal ligament
- Good to excellent long-term outcomes following CTR in up to 90% of reported cases
- Surgical treatment has been reported to demonstrate better long-term response when compared to splinting
- Surgical procedure to increase space in the carpal tunnel and reduce pressure on the median nerve, via division of the transverse carpal ligament
- Acupuncture therapy has been reported to improve median nerve function
Differential Diagnosis
- Cervical radiculopathy
- Proximal median neuropathy
- Thoracic outlet syndrome
- Central nervous system (CNS) disorders
Osteoarthritis (OA)
Epidemiology
- Most common arthritis
- A leading cause of chronic pain and disability in older adults
Commonly Involved Joints
- Hand – most commonly involved in OA – distal interphalangeals (DIPs), proximal interphalangeals (PIPs), first carpometacarpal (CMC)
- Feet – first metatarsophalangeal (MTP), subtalar joint
- Knee
- Hip
- Spine
- Rarely affects elbow, wrist, ankle – look for history of trauma, congenital abnormality, systemic or crystalline disease
- Feet – first metatarsophalangeal (MTP), subtalar joint
Definition
- OA can be defined pathologically, radiographically, or clinically
- Radiographic OA has long been considered the reference standard for epidemiology
- Not all subjects with radiographic OA are symptomatic and not all with symptoms have radiographic OA
Risk Factors
- Age – the strongest risk factor, most commonly age >40 years
- Females
- Obesity – the strongest modifiable risk factor
- Previous injury
- Family history (genetic predisposition)
- Joint malalignment (mechanical factors)
Pathogenesis
- Caused by an interplay of multiple factors – joint integrity, genetics, local inflammation, mechanical forces, cellular and biochemical processes
- Abnormal remodeling of joint tissues is driven by a host of inflammatory mediators within the joint
- OA pathogenesis is now thought of as an active response to injury rather than a degenerative process
- Degradation of matrix and articular cartilage
- Chondrocytes become “activated” and increase production of matrix proteins and matrix-degrading enzymes during inadequate repair response
- Aggrecanases, collagenases, serine and cysteine proteinases, matrix metalloproteinase (MMP)-3, MMP-13, ADAMTS-5 are all reported to play a role
- Chondrocytes become “activated” and increase production of matrix proteins and matrix-degrading enzymes during inadequate repair response
- Thickening of the subchondral bone
- Bone remodeling may be initiated at sites of local bone damage resulting from excessive repetitive loading
- Formation of osteophytes
- At joint margins and entheseal sites – new bone is added by endochondral ossification, leading to osteophyte formation
- Variable degrees of inflammation of the synovium
- Synovial infiltrates have been identified in many OA patients, though lower in grade than in rheumatoid arthritis (RA)
- Prevalence of synovitis increases with advancing age
- Interleukin (IL)-1 beta and tumor necrosis factor (TNF) alpha suppress matrix synthesis and promote cartilage catabolism, IL-17 induces chemokine production by synovial fibroblasts and chondrocytes
- Synovial infiltrates have been identified in many OA patients, though lower in grade than in rheumatoid arthritis (RA)
- Degeneration of ligaments, menisci in the knee, and hypertrophy of the joint capsule, as any meniscal or ligamentous injury predisposes to the development of OA
- Degradation of matrix and articular cartilage
Symptoms
- Hand
- Pain on usage
- Mild morning or inactivity stiffness, usually lasting <30 minutes
- Characteristic sites – DIPs, PIPs, base of the thumb
- Pain on usage
- Knee and hip
- Usage-related pain
- Often worse toward the end of the day
- Pain relieved, usually incompletely, with rest
- Mild morning or inactivity stiffness (gelling)
- Advanced OA – may have rest or night pain
- OA symptoms are often episodic or variable in severity and slow to change
- Usage-related pain
Physical Examination
- Hand
- Heberden’s (DIPs) and Bouchard’s (PIPs) nodes
- Squared appearance to the first CMC is classic
- Heberden’s (DIPs) and Bouchard’s (PIPs) nodes
- Feet
- First MTP involvement may result in hallux valgus or hallux rigidus
- Knees
- Tenderness to palpation of joint
- Crepitus
- Joint effusion
- Synovial fluid in OA typically exhibits
- Normal viscosity
- Mild pleocytosis (WBC <2000/mm3)
- Normal viscosity
- Synovial fluid in OA typically exhibits
- Osteophytes – may have palpable bony enlargements at periphery of joint
- Restricted movement and range of motion
- Tenderness to palpation of joint
- Hip
- Hip pain worsened with internal or external rotation
- Anterior and inguinal pain generally indicative of true hip joint involvement
- Check both hips, as ∼20% have bilateral OA
- Full exam should also include evaluation for referred pain sources
- Trochanteric bursitis
- Lumbosacral spine
- Knee pathology
- Trochanteric bursitis
- Hip pain worsened with internal or external rotation
Osteoarthritis Treatment
Non-Pharmacologic Treatments
- Instruction on joint protection techniques
- Thermal modalities – paraffin wax treatments, heat packs, and heating pads
- Strong recommendation for weight loss in patients with hip or knee OA
- Exercise – cardiovascular and/or resistance land-based exercise, aquatic exercise, and manual therapy (physical/occupational therapy) in combination with supervised exercise have all been helpful
- Participation in self-management programs and psychosocial interventions (diet, exercise instruction) can offer significant benefit
- Tai chi programs have been reported to be beneficial in small studies
- Assistive devices, orthotics, and splinting as needed:
- Splints for trapeziometacarpal joint OA
- Medially wedged insoles for lateral compartment knee OA
- Laterally wedged subtalar strapped insoles for medial compartment knee OA
- Medially directed patellar taping for knee OA
- Splints for trapeziometacarpal joint OA
Pharmacologic Therapy
- Acetaminophen
- Topical capsaicin – efficacy is controversial, but some advocate for its use as adjunctive treatment
- Topical non-steroidal anti-inflammatory drugs (NSAIDs), e.g. topical diclofenac, is a safe option especially if age >75 years
- Oral NSAIDs, including non-selective and selective (cyclo-oxygenase (COX)-2 inhibitors) (Table 1.1)
- Monitor for gastrointestinal (GI) and cardiac adverse effects (GI bleeding, abdominal pain, MI, worsening CHF)
- Avoid in chronic kidney disease
- COX-2 selective inhibitors are associated with increased cardiovascular risk and should be avoided in patients with cardiovascular risk factors
- Tramadol can also play a role in pain relief, especially in patients for whom NSAIDs or acetaminophen are contraindicated
- Intra-articular injection of long-acting corticosteroid can be effective for painful flares of OA, especially in trapeziometacarpal joint OA and knee OA
- Topical non-steroidal anti-inflammatory drugs (NSAIDs), e.g. topical diclofenac, is a safe option especially if age >75 years
| Clinical scenario | Recommended regimen |
|---|---|
| History of GI bleed, but none within the past year | Non-selective NSAID or COX-2 inhibitor + proton-pump inhibitor |
| History of GI bleed within the past year | COX-2 inhibitor + proton-pump inhibitor |
| Patient taking low-dose aspirin for cardioprotection | Non-selective NSAID other than ibuprofen* + proton-pump inhibitor |
*The FDA warns against ibuprofen and low-dose aspirin used in combination, due to a pharmacodynamic interaction causing a decreased cardiprotective effect
Table 1.1 Use of NSAIDs in high-risk populations.
Intra-Articular Viscosupplementation
- Multiple brands available (Table 1.2)
- Currently only FDA-approved for knee osteoarthritis
- Few head-to-head comparisons and generally small studies
- Currently only FDA-approved for knee osteoarthritis
- Mechanism
- Hyaluronic acid (HA) is a constitutive component of the matrix cartilage
- Plays a key role in maintenance of joint homeostasis
- Biologically active component secreted by chondrocytes that protects cartilage from degradation by interacting with MMPs and pain mediators
- In OA, concentration and molecular weight of HA is reduced
- Plays a key role in maintenance of joint homeostasis
- Exact mechanism not understood
- Proposed mechanism
- Biomechanical – improves synovial fluid viscoelasticity, increases joint lubrication, coats articular cartilage surface
- Analgesic – reduces pain eliciting nerve activity, reduces prostaglandin- or bradykinin-induced pain
- Anti-inflammatory – reduces levels of inflammatory mediators, decreases leukocyte chemotaxis
- Antioxidant
- Chondroprotective – stimulation of endogenous HA and extra matrix component synthesis, protects against chondrocyte apoptosis, inhibits cartilage degradation
- Biomechanical – improves synovial fluid viscoelasticity, increases joint lubrication, coats articular cartilage surface
- Hyaluronic acid (HA) is a constitutive component of the matrix cartilage
- Side effects
- Generally well tolerated, most side effects related to injection site reactions
- Rare pseudosepsis reactions, especially with high molecular weight HA
- Patients present with acute joint swelling, pain, and warmth
- Care must be taken to distinguish this syndrome from true septic joint
- Patients present with acute joint swelling, pain, and warmth
- Generally well tolerated, most side effects related to injection site reactions
- Clinical use
- Used in knee OA patients who fail non-pharmacologic treatments, acetaminophen, NSAIDs, and intra-articular steroids
- Studies have shown improvement in pain scores with viscosupplementation, however:
- Appropriate patient selection is not well defined
- Many studies do not control for concomitant pharmacologic therapy
- Double-blind, placebo-controlled trials report a large placebo effect
- Appropriate patient selection is not well defined
- Campbell et al. in 2007 reviewed six systematic reviews on viscosupplementation
- Three reviews showed viscosupplementation more effective than placebo
- Three reviews suggested no benefit
- Three reviews showed viscosupplementation more effective than placebo
- Rutjes et al. in 2012 systematic review and meta-analysis concluded that viscosupplementation is associated with a small and clinically irrelevant benefit and an increased risk for serious adverse events
- Viscosupplementation is not recommended for OA of the hip due to lack of data
- Used in knee OA patients who fail non-pharmacologic treatments, acetaminophen, NSAIDs, and intra-articular steroids
| Product | Dosing | Molecular weight (in M Daltons) |
|---|---|---|
| Hyalgan (sodium hyaluronate) | Once weekly for 3–5 weeks | 0.5–0.73 |
| Supartz (sodium hyaluronate) | Once weekly for 3–5 weeks | 0.6–1.1 |
| Orthovisc (high molecular weight hyaluronan) | Once weekly for 3–4 weeks | 1.0–2.9 |
| Euflexxa (1% sodium hyaluronate) | Once weekly for 3 weeks | 2.4–3.6 |
| Synvisc (hylan G-F 20) | Once weekly for 3 weeks | 6 |
| Synvisc-One (hylan G-F 20) | Once | 6 |
Table 1.2 Comparison of viscosupplementation products.
Glucosamine and Chondroitin Sulfate
- Both are labeled as supplements in the United States and are therefore do not need to be approved by the FDA before they are marketed; therefore variations in dosage among the marketed supplements exist, making comparisons difficult
- The GAIT trial for knee OA demonstrated that response to glucosamine and chondroitin alone or in combination were not different from placebo
- A small subgroup analysis of patients with moderate-to-severe knee OA did show statistically significant improvement with combination therapy
- 2-year follow up did not demonstrate clinically significant differences between the treatment groups
- A small subgroup analysis of patients with moderate-to-severe knee OA did show statistically significant improvement with combination therapy
- Other studies have shown efficacy with these agents but were criticized for flaws, including failure to adhere to intention to treat, small numbers of patients, potential bias related to sponsorship of the study, and inadequate masking of the study agent
- As a result, recommendations from leading organizations differ:
- American College of Rheumatology (ACR) 2012 statement recommends against the use of glucosamine and chondroitin
- European League against Rheumatism (EULAR) recommendations include glucosamine and chondroitin as viable treatment option for knee OA
- OARSI (Osteoarthritis Research Society International) recommends a trial for 6 months, followed by reassessment and discontinuation if ineffective at that time
- American College of Rheumatology (ACR) 2012 statement recommends against the use of glucosamine and chondroitin
Surgery for Osteoarthritis
- Joint replacement for the knee and hip should be considered in patients with radiographic evidence of OA along with chronic pain and disability that is refractory to treatment with non-pharmacologic and pharmacologic interventions
- Surgical intervention should be performed before the development of significant deformities, contractures, functional loss, or muscle atrophy for optimal result
- Surgical intervention should be performed before the development of significant deformities, contractures, functional loss, or muscle atrophy for optimal result







