Shoulder Stiffness
A major function of the shoulder is to position the hand in space. When the shoulder is stiff, the hand becomes less functional because its access to the space around it is restricted. That is why stiffness of the shoulder is so disabling: it affects not only the shoulder but also the hand.
Prior to the advent of shoulder arthroscopy, surgical treatment of the stiff shoulder was seldom attempted. Open releases were so painful for patients that vigorous stretching after release was out of the question, and the shoulder would usually stiffen again after open release. Manipulation under anesthesia was the mainstay of treatment, but some shoulders had such thick capsules and dense adhesions that they could not be manipulated, and fracture of the humerus remained a very real possibility during manipulation. The ability to arthroscopically treat stiffness has greatly enhanced our ability to surgically improve shoulder dysfunction.
Stiffness in the nonarthritic shoulder can have two components:
TYPES OF STIFFNESS (NONARTHRITIC)
Most nonarthritic stiff shoulders fall into one of three categories:
Adhesive capsulitis usually has only intra-articular restriction due to an inflammatory process affecting the joint capsule, without any subacromial or subdeltoid adhesions.
Postoperative stiffness after rotator cuff repair typically has both intra-articular restriction due to capsular thickening and shortening, as well as subacromial/subdeltoid adhesions. However, postoperative stiffness after labral repair (intra-articular arthroscopic surgery) demonstrates capsular thickening causing intra-articular restriction, but no subacromial adhesions.
Posttraumatic stiffness after fracture of the proximal humerus is most common after surgical treatment of three-part and four-part fractures. In such cases, the source of the stiffness is both intra- and extra-articular, as in other types of postoperative stiffness. Malunion of proximal humerus fractures can cause loss of motion that is not true stiffness. For example, displaced greater tuberosity fractures can cause bony subacromial impingement that blocks overhead motion to varying degrees. Furthermore, varus malunion of humeral neck fractures causes rotational medialization of the greater tuberosity, resulting in shortening of the supraspinatus and infraspinatus muscle-tendon unit in addition to shortening of its moment arm. These biomechanical derangements contribute to loss of motion. Posttraumatic stiffness after glenoid fracture is usually due either to intra-articular adhesions or to posttraumatic arthritis.
ADHESIVE CAPSULITIS
The natural history of untreated adhesive capsulitis passes through freezing, frozen, and thawing stages. Some authors treat adhesive capsulitis differently at different stages.
In contradistinction to stage-specific treatment, we have a standard treatment protocol regardless of the stage of adhesive capsulitis. Our mainstay of treatment is to inject the stiff shoulder three consecutive times at monthly intervals. The injections consist of a mixture of Xylocaine and DepoMedrol and are given into both the intra-articular space and the subacromial space. The patient is placed on a self-administered stretching program that emphasizes restoration of elevation, external rotation, and internal rotation.
If, after 3 months of the above regimen, patients still have significant stiffness, we offer them the choice of continued stretching (but without any further injections), or arthroscopic capsular release and lysis of adhesions.
For patients that choose stretching alone, the duration of the stiffness is usually quite prolonged, often in excess of a year, and it may never fully resolve.
Patients that elect to have arthroscopic capsular release and lysis of adhesions have rapid and dramatic improvements in pain relief as well as range of motion.
In performing the surgery, we first release the rotator interval (including the superior glenohumeral ligament) with a 3-mm electrocautery probe (OPES System; Arthrex, Inc., Naples, FL), while viewing from a posterior portal (Fig. 21.1). Then, we switch the scope to the anterior portal and release the posterior capsule with a pencil-tip cautery (from 11 o’clock down to 7 o’clock in a right shoulder) (Fig. 21.2). Then, we release the axillary pouch, staying at least 5 mm away from the labrum in order to protect the axillary nerve (Fig. 21.3). Next, with the pencil-tip cautery still in the posterior portal, we release the anterior capsule all the way up to the midglenoid notch (Fig. 21.4). Since our posterior working portal has an angle of approach parallel to the glenoid face, it is much easier to release the anterior capsule through this portal than through an anterior portal. The superior capsule is not released, as it does not restrict the primary motions of elevation, external rotation, and internal rotation.
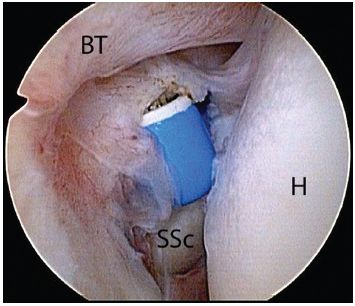
Figure 21.1 Right shoulder, posterior viewing portal demonstrating release of the rotator interval with an electrocautery. This is the first step of a glenohumeral release for stiffness and is performed from the superior border of the subscapularis tendon (SSc) to and including the superior glenohumeral ligament. BT, biceps tendon; H, humerus.
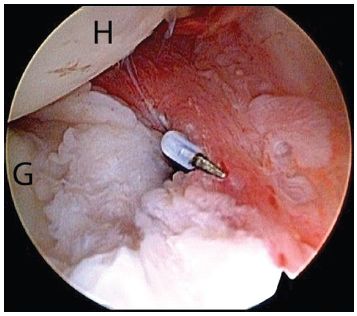
Figure 21.2 Right shoulder, anterosuperolateral viewing portal, demonstrating release of the posterior capsule with a pencil-tip electrocautery. Performing the posterior release prior to the inferior and anterior capsular release provides freedom of movement for the electrocautery device. G, glenoid; H, humerus.
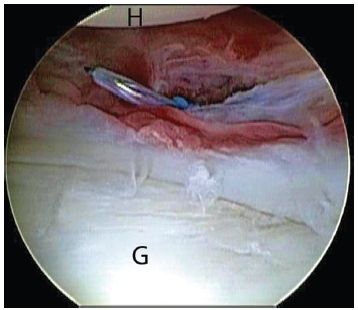
Figure 21.3 Right shoulder, anterosuperolateral viewing portal, demonstrates inferior capsular release with a pencil-tip electrocautery. Note that the electrocautery is at least 5 mm lateral to the labrum in order to avoid iatrogenic injury of the axillary nerve. G, glenoid; H, humerus.
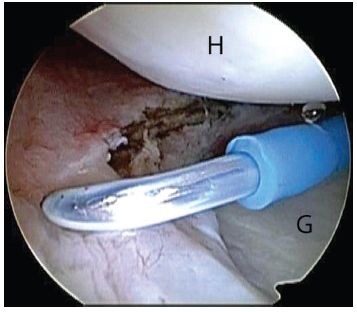
Figure 21.4 Right shoulder, anterosuperolateral viewing portal, demonstrates anterior capsular release performed with a pencil-tip electrocautery introduced through the posterior portal. The posterior portal provides an angle of approach parallel to the glenoid, making it an ideal working portal for the anterior capsular release. G, glenoid; H, humerus.
After capsular release, we take the arm out of traction and manipulate it through a full range of motion while manually stabilizing the scapula. Even with complete capsular release, manipulation is necessary to stretch the muscles which have become shortened and stiff (thixotrophy) because the adhesive capsulitis has restricted their excursion over a prolonged period. Then, the arm is put back into traction and we look into the glenohumeral joint to confirm the adequacy of the capsular release (Fig. 21.5). Once that is done, we place our arthroscope in the subacromial space. In adhesive capsulitis, the subacromial space is usually normal, in which case we either do nothing or we do an arthroscopic subacromial decompression (if the patient has a type 2 or 3 acromion).
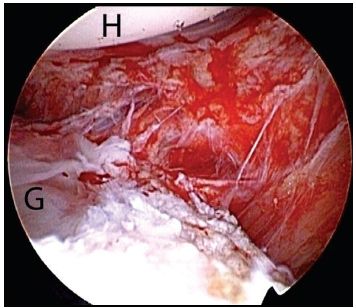
Figure 21.5 Right shoulder, posterior viewing portal. Following capsular release and manipulation under anesthesia, inspection of the axillary recess demonstrates a complete release with visualization of muscle fibers.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








