Pain Management and ROM Desensitization
Imagine three clinical scenarios in which patients present with different knee conditions. The first patient presents with a knee sprain which happened 1 week ago. It is painful, swollen and stiff and on examination has only a limited range of movement (ROM). Another patient had a knee joint fracture. It is now 6 weeks later and the plaster has just been removed. The knee is painful, swollen, has restricted ROM and is very stiff. Finally, another patient had knee surgery 1 year ago. On examination the passive knee ranges have mostly recovered but pain and stiffness are still limiting the patient’s functional ranges.
The clinical examples above represent three conditions in which pain, stiffness and ROM losses are shared symptoms. However, the ROM management will be different for each of these presentations. These scenarios raise several questions about ROM rehabilitation in the presence of pain:
 In the presence of pain, when is stretching/ROM challenge safe or useful?
In the presence of pain, when is stretching/ROM challenge safe or useful?
 When is pain a signal to stop stretching?
When is pain a signal to stop stretching?
 How soon after injury should ROM challenges commence?
How soon after injury should ROM challenges commence?
 Can movement be stiff and painful without inflammation, damage or shortening?
Can movement be stiff and painful without inflammation, damage or shortening?
 What can help to promote desensitization?
What can help to promote desensitization?
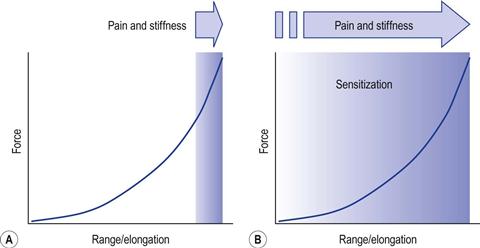
ROM Sensitization
Sensitization is a neurological process in which the central nervous system can change, distort or amplify the experience of pain in a manner that no longer reflects the noxious stimuli from the periphery.1 ROM sensitization is the limitation in ROM owing to an increase in the subjective experience of stiffness and pain. It is a common phenomenon in acute and chronic musculoskeletal conditions.2 Of particular focus here is ROM sensitization in which pain and stiffness are experienced in functional ranges, in the absence of current tissue damage, inflammation or tissue shortening (Fig. 9.1). This phenomenon will be termed here persistent ROM sensitization.
Under normal circumstances sensitization is a positive protective response to injury. Following injury, the site of damage, as well as its surrounding area, will become hypersensitive to touch, movement or temperature. This sensitivity serves as a warning system to protect the weakened tissues from further damage.3
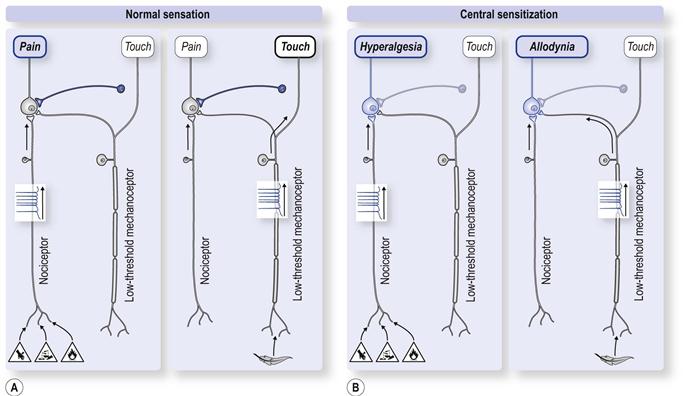
Sensitization is brought about by increased excitability of nociceptors in the periphery and central neurons that convey the nociceptive information. Peripherally, inflammatory by-products lower the nociceptors’ threshold, resulting in their increased excitability.4–8 Centrally, within the spinal cord and brain, sensitization is associated with complex biological and functional reorganization of sensory transmission and motor and autonomic responses. The outcome is facilitation and amplification of nociceptive signals throughout the nervous system.9–16
Sensitization tends to spread in the spinal cord to influence the receptive field of neurons that are not directly related to the site of injury. This spread can even affect the receptive fields of spinal neurons on the non-affected side.7,8 This means that pain sensitivity can be experienced further away from the site of injury as well as on the opposite limb. For example, in some patients with osteoarthritis of the hip there is increased pain perception and skin sensitivity at locations distant to the joint and even on the non-affected side.17
The consequence of sensitization is an elevated pain experience which is disproportionate to underlying tissue strain or damage (Fig. 9.2). Such hypersensitivity means that previously normal functional ranges are experienced as painful, and end-ranges which were uncomfortable become intolerably painful.
Persistent sensitization
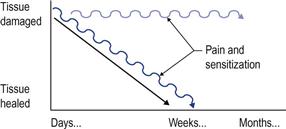
Under normal circumstances pain and sensitization tend to diminish as the individual recovers from their injury. However, for some individuals persistent central sensitization can be maintained long after tissue healing has taken place (Fig. 9.3). It can arise spontaneously, even without an obvious event of injury. Once central sensitization has taken place it does not seem to be dependent any longer on nociception from the damaged tissues.11 Indeed, in many chronic pain conditions there is an absence of “fresh” tissue damage or inflammation.1,18 Consequently, persistent sensitization may lead the patient (and the therapist) to the erroneous belief that the painful area is damaged and inflamed.
Persistent pain sensitization is a feature of many chronic musculoskeletal conditions.1 It can be demonstrated in injury/post-surgical conditions,19 chronic low back and neck pain, trapezius myalgia, whiplash conditions, painful jaw and post-immobilization.1,20–25 Sensitization also plays a role in the various tendinopathies such as tennis elbow and supraspinatous, Achilles and patellar tendinopathies.26–31 In arthritis, both joint nociceptors and related spinal nociceptive neurons show pronounced sensitization for mechanical stimulation.32
ROM sensitization has also been demonstrated in patients with chronic low back pain.33 Athough they experience pain and stiffness in forward bending their flexion ROM is no different from asymptomatic individuals.34–37 This suggests that the range limitation was due to reduced tolerance to stretching rather than physical shortening of the muscles.33 A similar example of ROM sensitization can also be observed in non-traumatic pain conditions such as chronic trapezius myalgia and chronic neck pain.22–25 In these conditions, the patient may experience substantial loss of neck rotation. (I have seen patients who could no longer drive because they were unable to turn their head during reversing.) Yet, such restrictions are not evident when the patient is lying relaxed on the table. Often there is full pain-free neck rotation when the therapist passively moves the neck.
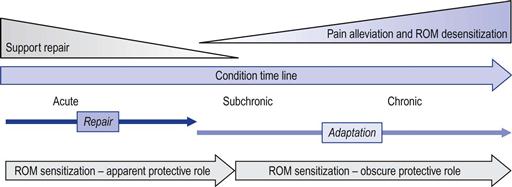
Central sensitization suggests that the experience of stiffness/pain during active movement or even manual stretching may be due solely to stretch sensitivity. It also implies that in some conditions ROM recovery can come about solely by desensitization (Fig. 9.4).
ROM Desensitization
The causes underlying the transition from acute to chronic sensitization are not fully understood. Factors associated with persistent sensitization include greater degree and longer duration of injury and genetic and psychosocial factors, to name but a few.19,38 This means that preventing or removing the cause of sensitization can be clinically elusive. The central nature of sensitization makes it even more elusive for physical therapies since there is nothing to “fix” peripherally in the tissues. All this suggests that to promote desensitization we need to focus on central process, somehow engaging the potential adaptive capacity of the nociceptive systems.
Before we set out to promote desensitization we have to establish in which conditions it will be beneficial.
When is ROM desensitization beneficial?
Whether ROM desensitization is beneficial depends on the role of pain within the patient’s condition. An important consideration is whether pain/sensitization serves a protective function, which is partly related to the duration of the patient’s condition, i.e. whether the condition is acute or persistent (Fig. 9.5).
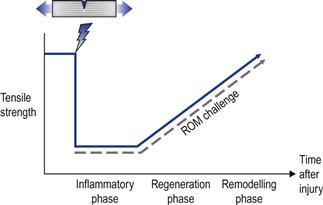
Acute condition – In acute conditions pain and sensitization are likely to be part of a protective strategy. In these conditions the subjective experience of stiffness may be due to localized swelling and sensitization. Improvement in pain and ROM sensitization are often spontaneous and related to the rate of tissue healing.39 Therefore, desensitization is not a therapeutic priority and the focus should be on assisting tissue repair. During that period the patient should be advised to remain active and ROM challenges should be within tolerable pain ranges. Furthermore, acute injuries are associated with tearing/damage of fibres and reduced tensile strength rather than structural shortening of tissues (Fig. 9.6). Therefore, end-range challenges may be unnecessary and unsafe in recently acquired injuries.
This raises the question of how long a condition is considered to be acute and when should the ROM challenges be introduced. Generally, tissue inflammation and regeneration are most marked within the first 2 weeks of injury. This duration may depend on the magnitude of damage and the type of tissue injured. A safety margin of 3–6 weeks is a useful time scale to consider a condition as acute.40 Indeed, in many injuries or post-operative conditions the repair processes will resolve within this time frame.
However, pain relief, rather than optimized tissue healing, is often the patient’s priority (most patients are not aware that inflammation is a positive aspect of repair). Some transient pain relief could be obtained by helping to minimize oedema and inflammatory by-products. Both of these therapeutic goals (healing and pain relief) can be achieved by the use of rhythmic movement (active or passive) and external intermittent compression within pain-free ranges (for full exploration of this topic see Lederman41).42,43 Stretching is unlikely to have a positive influence on these processes.41
So, in acute conditions, ROM recovery can come about primarily by repair processes (Fig. 9.7).
Chronic conditions – ROM desensitization can be beneficial in persistent musculoskeletal conditions. Here there is no obvious protective function for pain and sensitization (since there is an absence of tissue damage/inflammation). However, this clinical reasoning can be a bit more complicated; in asymptomatic, pain-free individuals it is common to find tissue damage without inflammation. For example, partial or full rotator cuff tears can be found in 34% of asymptomatic individuals.44 Similarly, in the spine, the prevalence of tissue damage in asymptomatic individuals can be fairly high: 27% disc protrusion, 54% disc degeneration and 28% annular tears.45 This means that tissue damage without pain is a fairly common occurrence. Another consideration is that pain does not always reflect the magnitude of tissue damage.46 For example, non-perforated rotator cuff tears can be more painful than full-thickness tears.47,48 In the spine, the degree of disc displacement, nerve root enhancement or nerve compression does not correlate with the magnitude of pain or disability.49 It means that in more chronic conditions the pain experience is (often) disproportionate or even unrelated to the underlying tissue damage.
This brings us back to the original question: whether ROM challenges would be safe for chronic conditions in which “old” tissue damage is accompanied by pain/sensitization. In the spinal and shoulder conditions described above physical activities/exercise are considered to be both safe and beneficial for improvement/recovery.50–60 From this it can be loosely concluded that, in chronic conditions in which there is pain and potential underlying “old damage”, ROM challenges are both safe and likely to be beneficial.
This leaves us with the question of how physical therapy can facilitate ROM desensitization.
Factors supporting ROM desensitization
Neural inhibitory mechanisms are inherent in all brain functions, including in the transmission of nociception and in desensitization processes.61 Physical therapies often aim to exploit these inhibitory mechanisms in order to control/alleviate pain.
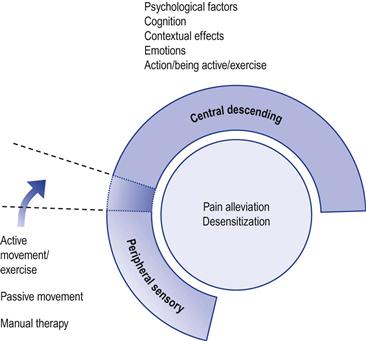
The modulation of nociception/pain can be largely by psychological/cognitive/emotional processes and partly by the physical sensory stimulation components of the treatment (Fig. 9.8). Although these mechanisms can be explored individually, in practice they are inseparable. It is difficult to specifically target one inhibitory system to the exclusion of another. Furthermore, the inhibition associated with desensitization is not exclusive to a particular aspect of the treatment, pathway or brain centre.62–64 Pain alleviation and desensitization should be considered as whole-person responses to the entire therapeutic encounter – psychological and physical.65
Psychological dimension
Therapies that target psychological factors are known to have a potent influence on the experience of pain and sensitization.62,66 The main psychological factors which may help mediate desensitization can be divided into three broad areas: emotional, cognitive and contextual factors.
Emotional factors
Sensitization and the experience of pain can be heightened by negative mood changes, such as depression, distress, anxiety and fear, whereas improvements in psychological well-being are often associated with alleviation of pain.67–73 When patients with lower back pain experience negative moods they tend to report an increase in pain levels and decreased pain tolerance, with positive moods having the opposite effect.74 This suggests that therapeutic interventions that help to improve psychological well-being may also have a positive impact on the pain experience.
There is a link between physical activities and a positive change in various psychological factors.75 Even (the humble) walking can have a positive influence on psychological factors such as depression,76 but also on chronic back pain.77–79 One way to exploit the links between physical activity, psychological well-being and pain is to encourage the patient to return to physical activities, particularly those that they enjoy.80
Cognitive–behavioural factors
The patient’s experience of pain and degrees of sensitization can be influenced by anxieties associated with their condition. Anxieties are often expressed as fears about movement, with the patient making inexact and disproportionate links between physical activities and the potential for greater pain and recurrence of injury (catastrophizing). When such anxieties were present, they were shown to have a negative influence on the experience of pain.37,80–86 For example, patients who have a higher catastrophizing score before surgery tend to experience more pain following surgery.82,87 Conversely, a decrease in pain catastrophizing can bring about a reduction in pain intensity and disability.88,89
These anxieties/fears can be alleviated by providing positive messages that reduce catastrophizing, empower the patient and promote self-efficacy in pain control.89 It is useful to provide information about the nature of sensitization, highlighting the disparity between tissue damage and pain and the potential to modulate the pain experience through various cognitive and behavioural means (Ch. 11).89,90 A patient with a chronic lower back condition who presents with ROM stiffness/discomfort can be informed that the area may be sensitive but not necessarily damaged, that discomfort experienced during or after movement in certain ranges does not mean that the spine has been re-damaged, and so on. These messages can be delivered explicitly and cognitively by verbal communication, but equally by “unspoken” messages that are conveyed implicitly by positive physical experiences (see reassurance, Ch. 11). This could explain why outcomes are similar for physical and cognitive–behavioural therapies in the treatment of chronic low back pain.35,91–94 It has been proposed that the improvements in both groups are mediated by alleviating the anxieties associated with pain.
Pain experiences can also be alleviated by diverting attention away from the area of pain.95–100 This can be done by drawing attention to another part of the body or to a particular mental or non-painful physical task.101 The immediate application of this clinically is to provide movement strategies that emphasize an external focus of attention. This can be towards an external goal or outcome of a task rather than focusing on the painful area. For example, patients with chronic low back pain can be instructed to perform reaching movements, at end-range, while focusing on the target rather than on the discomfort in the back (“forget the back therapy”).
Within the cognitive–behavioural dimension, relaxation techniques also have an important role in helping to control acute and chronic pain conditions.102–109 Relaxation techniques can help distract attention from pain, support an internal locus of control and improve self-efficacy in managing pain.107,108 Simple relaxation techniques, such as progressive muscle relaxation, have been found to be effective in managing chronic pain.107,108,110
Contextual effects
Contextual effects are the environmental factors which influence the patient’s perception of the treatment. These factors can have a profound lasting effect on the patient’s experience of pain.111–115 Often, these factors are not directly associated with the physical aspect of the treatment but associated with the therapeutic relationship,116 the patient’s expectations, previous therapeutic experiences, treatment credibility and the patient’s preference for a particular treatment.35,92,94,111–113,117–119 When these contextual factors are positive they provide the individual with internal narratives that engage them psychologically, behaviourally and physiologically in their recovery.114
Contextual effects can have a significant influence on neurophysiological processes including sensitization/desensitization.120 For example, the individual’s expectation of pain, or, conversely, of pain relief, can determine the magnitude of spinal sensitization.121 This was demonstrated in a study in which hypersensitivity to mechanical stimulation was induced by heating the skin of the forearm.121 The area of sensitization was smaller in subjects who received a placebo analgesic in the form of a sham magnet (a metal plate shaped like a magnet applied to the sensitive area). Brain and spinal imaging during such placebo analgesia has demonstrated that the subject’s report of reduced pain coincides with decreased activity in the brain pain areas with a concurrent inhibition of nociceptive input within the spinal cord.115,120 There is some evidence that contextual effects on pain are more prominent in treatments that contain physical events, such as manual therapy, than in interventions where medication or psychological approaches are used.122
Physical components
Active movement
Active movement challenges can also play a role in ROM desensitization. Several studies have explored the effects of exercise on induced pain in healthy individuals.123 Transient desensitization has been demonstrated during and after different forms of exercise. In dynamic, aerobic exercise desensitization is more likely to occur when the exercise is performed for more than 10 minutes and at above 70% of maximal aerobic capacity.124–126 For isometric exercise it seems that less effort and duration is required for desensitization to take place.63,127,128 It can be observed at an intensity as low as 25% of full contraction force and within a period of time as brief as 1 minute.129,130
Reduced hypersensitivity to activity has also been demonstrated in patients with chronic musculoskeletal conditions. In tennis elbow, active wrist movement combined with superimposed elbow joint mobilization demonstrated an immediate reduction in sensitization.26–28 Similarly, in patients with chronic neck pain, 3 minutes of specific neck exercises, performed in non-painful ranges, was shown to reduce local hypersensitivity and improve cervical pain-free ranges.131 Overall, these studies demonstrate that active forms of ROM challenges could be useful for inducing desensitization. This could be achieved both by rhythmic, cyclical movement and by static isometric-like activities. These challenges should be applied within the pain-free ranges of movement.
These principles can be applied clinically within the framework of a functional approach. For example, a patient with chronic low back pain can be instructed to perform a repetitive reaching movement, towards a target marked by the therapist’s hand. The procedure starts by exploring the patient’s pain-free range by moving the target hand to different positions. Once a comfortable sphere of movement is established the patient repeats the reaching movement towards these positions. After several reaching cycles the therapist surreptitiously moves the target hand further away. If there is no pain at the new position the patient is instructed to repeat the movement to this range, and so on (see accompanying Video).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree