Chapter 7 Nonthrust Procedures
Mobilization, Traction, and Soft Tissue Techniques
The chiropractic profession did not develop most of the techniques and procedures discussed in this chapter. Therefore, they should not be considered unique to the chiropractic profession. Moreover, a small percentage of chiropractic professionals do not use them because of the exclusiveness of thrust techniques. However, they are important forms of manual therapy that can be used alone or in combination with thrust procedures. Procedures characterized by a high-velocity thrust (adjustment) may indeed have effects that are different than and, in certain clinical situations, superior to nonthrust procedures.1,2
Nevertheless, both procedures share common physical attributes and overlapping potential positive clinical effects. Grieve3 contends that all mobilizations and manipulations are actually soft tissue techniques, because it is in the soft tissue that the lesions treated and the effects produced are found.
Chiropractors commonly encounter circumstances in which thrust manipulation is contraindicated or the primary neuromusculoskeletal (NMS) disorder is not the product of joint dysfunction or a pathologic condition. In such circumstances, it benefits both the doctor and the patient if the chiropractor is skilled in alternative nonthrust manual procedures. Indeed, various and numerous forms of manual therapy exist within the profession of chiropractic.4 Examples of circumstances in which nonthrust procedures might be more appropriate include the treatment of the older adults or patients with osteoporotic or extremely acute conditions, treatment of patients in the later stages of pregnancy, or treatment of patients with a diagnosis of myofascial pain syndrome (trigger point).
Nonthrust procedures are also viable options in circumstances in which the doctor is unable to produce a thrusting force that is capable of producing joint cavitation. If the doctor’s size, strength, or ability to develop the needed speed and amplitude is inadequate to produce the necessary force, some other type of technique application may provide an effective alternative. This is suitable only in the circumstance in which both thrust and nonthrust procedures are assumed to have the same physical effects. All manual therapies are not equivalent simply because a wide variety of methods exist.5 Most of the procedures described in this chapter were developed empirically. Typically they are associated with a particular innovator or profession, but invariably development, refinement, and modification by subsequent innovators has led to an environment of multiple definitions, descriptions, and variations of the same procedure. The intention of this chapter is not to present a comprehensive discussion of the variations and nuances of each procedure, but to offer a fair representation of techniques and an overview of each method presented. Ideally, the descriptions of the procedures contained within this chapter will broaden your awareness of nonthrust manual procedures and stimulate further critical evaluation of those procedures that pique your interest.
Joint mobilization
Definition
Joint mobilization may be defined as a passive therapeutic movement up to but not exceeding the anatomic end range of joint movement. A nonthrust maneuver is not commonly applied beyond a joint’s elastic barrier. Movement beyond the elastic barrier takes the joint into the paraphysiologic joint space and is typically associated with an audible pop or click. Therefore mobilization is less commonly associated with an audible crack than manipulation. Grieve3 considers spinal mobilization a more gentle, persuasive pressure performed within the available accessory range or at the end of the accessory range. However, mobilization can be applied over a wide range and can thus involve a series of movements (stages or grades). Mobilization is a coaxing, repetitive, rhythmic movement of a joint that can be resisted by the patient. Inherent within a nonthrust manipulation is a patient feedback mechanism. Because the motion is relatively slow, controlled, and gentle, the patient can report the effect of the technique during the application.
Primary goal
The primary goal of mobilization is to restore optimal range of motion (ROM), quality of movement, and comfort to the joint being addressed. Indirect benefit is thought to accrue because of improved function within each part of the kinetic chain in need of treatment. For example, compensatory mechanical stress on adjacent structures may be reduced when a previously painful or restricted part of the chain is returned to normal function. Such return to comfortable, maximal ROM usually serves as a passive treatment end point.6 Mobilization can be performed in a physiologic direction (rotation, flexion, extension, or lateral flexion) or in a nonphysiologic direction (e.g., longitudinal traction or posterior-to-anterior [P-A] gliding). Furthermore, various types of mobilization can be used to restore segmental motion and perhaps reduce pain in the spine and extremities. Graded oscillation, progressive stretch, and continuous stretch mobilization form the basis for most types of mobilization techniques.
Various types
Graded oscillation technique is a form of mobilization whereby alternate pressure (on and off) is delivered at different parts of the available range.7 The amplitude of the oscillation may also vary according to the purpose of the technique. Oscillatory technique is graded on a 1-to-4 scale based on the amplitude of the motion and part of the range being reached (Box 7-1). The vibratory nature of the graded oscillation technique is thought to activate sensory mechanoreceptors that may help reduce pain and improve proprioceptive function. Box 7-2 lists generalized procedural steps for the application of graded oscillatory mobilization.
BOX 7-1 Amplitude Grades for Oscillatory Technique
| Grade I | A small-amplitude movement near the starting position of the range |
| Grade II | A larger-amplitude movement that carries well into the range, occupying any part of the range that is free of stiffness or muscle spasm |
| Grade III | A large-amplitude movement that moves into stiffness or muscle spasm |
| Grade IV | A small-amplitude movement that stretches into stiffness or muscle spasm |
BOX 7-2 Generalized Graded Oscillatory Mobilization Procedure
Progressive stretch mobilization involves a series of successive short-amplitude, spring-type pressures or a series of short-amplitude stretch movements.8 The pressure or stretch is imparted at progressive increments of the range. Progressive stretch is graded on a 1-to-4 scale, as is graded oscillation. The major indication for the use of progressive stretch mobilization is mechanical or soft tissue restriction or both.
In addition, special attention should be given to the traction component of mobilization. Where anatomic relationships allow traction to accompany mobilization, traction should be used as an integral part of the treatment program. In many cases of pain-induced failure of a mobilization technique, that is, when angular or even translational force vectors produce increased pain, pure traction techniques may still be useful. This fact reinforces the concept that traction is one of the least invasive mobilization methods.9
Selected examples
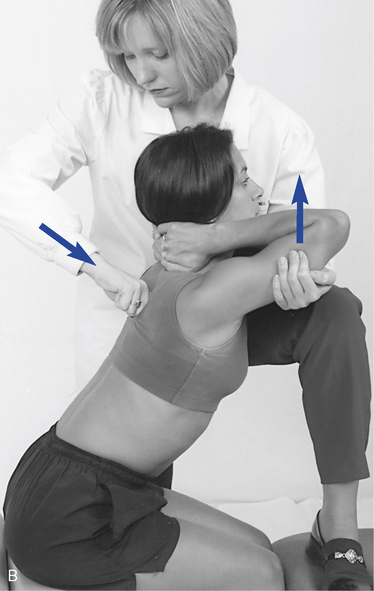
Progressive Stretch Thoracic Extension (Figure 7-3)
The patient lies in the prone position with the hands interlaced behind the neck and the elbows together (Figure 7-3, A). The clinician stands on the side of the table and grasps the patient’s arms from underneath with the cephalic hand. The caudal hand is used to establish a broad contact over the spine below the section to be mobilized. The clinician simultaneously and progressively raises the arms to the patient’s tolerance while applying stabilizing pressure over the spine. This procedure may also be done in the seated position (Figure 7-3, B). There is powerful leverage produced in both positions, and caution must be used to prevent injury.
Manual traction-distraction
Definition
The term traction refers to the process of pulling one body in relationship to another, which results in separation of the two bodies. Traction is passive translational movement of a joint, which occurs at right angles to the plane of the joint, resulting in separation of the joint surface. Kaltenborn10 graded manual traction by the three effects it produces. With the first effect, there is no appreciable joint separation because only enough traction force is applied to nullify the compressive forces acting on the joint. The compressive forces are the result of muscle tension, cohesive forces between articular surfaces, and atmospheric pressure. The second effect produces a tightening in the tissue surrounding the joint that is described as “taking up the slack.” The third grade of traction requires more traction force to produce a stretching effect into the tissues crossing the joint. The principal aim of treatment is restoration of normal painless ROM (Box 7-3).
BOX 7-3 Treatment Aims of Manual Traction
Traction produces measurable separation of vertebral bodies and centripetal forces exerted by the tension applied to surrounding soft tissues. However, traction has other effects as well. Grieve11 identifies some other effects that are the result of both sustained and rhythmic traction (Box 7-4).
Manual traction is not a unique and separate form of treatment but is simply one form of passive mobilization.12 Traction can be varied in many ways; almost any form of passive handling may be used, with some form of oscillation or as a static hold. Therefore, a longitudinal movement may be performed as an oscillatory mobilization, as a slow rhythmic stretch, or as a static traction. Traction may be manual or mechanical, static or rhythmic, or fast or slow; the force applied may be strong or gentle, and it may be applied symmetrically or asymmetrically. These variations must be explored to determine which combination is most suitable for the patient’s needs or the clinician’s abilities. The effects of traction are not necessarily localized, but may be made more specific by careful positioning.
For traction to achieve maximal success in a minimal amount of time, the patient must be positioned accurately, a minimal effective force must be used, and each patient’s treatment must be based on his or her signs and symptoms rather than the diagnosis. The potential theoretic effects of traction on the spine include stretching of the muscles and ligaments, improving glide of the dural root sleeves, freeing fixation of articular facets, changing hydrostatic pressure in the discs and repositioning nuclear fragments, and improving the blood supply to the spine and its surrounding structures.13
Specific procedures
Manual Lumbar Flexion-Distraction (Cox Method)
Flexion-distraction is a mechanically assisted form of joint mobilization or distraction, blending osteopathic and chiropractic principles into one technique. Flexion-distraction has been advanced in the chiropractic profession largely by the work of chiropractor James Cox. Much of Cox’s initial work in developing his technique of flexion-distraction was based on the work of the osteopath J.V. McManis. Moreover, the design of the early Cox table was a direct emulation of the McManis table of the early 1900s. This manual table provided an advantage to both the patient and the clinician, allowing a multiple-plane approach to distraction, including flexion-extension, lateral flexion, and rotation. The McManis table incorporated many of the features that appear on contemporary tables, including split headpieces, multiple sections adjustable for patient comfort, and positioning for various adjustive maneuvers.14
A number of lumbar disorders have been presented as conditions suitable for treatment with lumbar flexion-distraction. They include lumbar disc protrusion, spondylolisthesis, facet syndrome, subluxation, and scoliotic curves of a nonsurgical nature.15 The theoretic benefits that have been associated with this form of spinal manipulation are presented in Box 7-5.
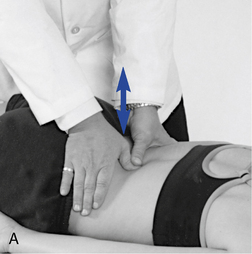
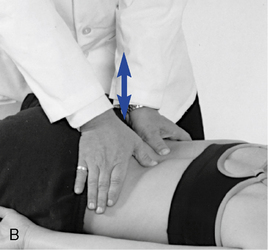
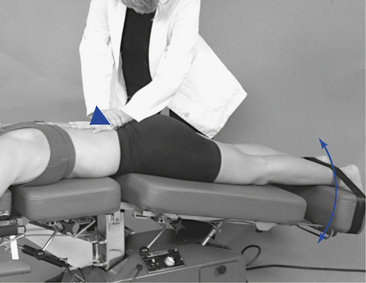
The Cox method uses a process of analysis that incorporates physical examination, orthopedic and neurologic testing, and imaging as indicated to establish the presence of a disc lesion, facet syndrome, or any other condition affecting the low back. Cox distraction therapy typically consists of three 20-second flexion-distraction sessions. Once the patient is properly positioned on the table and the tolerance of the patient to flexion is determined, the sessions can begin. The hand is placed over the spinous process of the superior vertebra of the motion segment to be distracted (e.g., to distract the L5–S1 segment, contact is on the L5 spinous process). The contact hand is slightly cupped, creating an indentation between the thenar and hypothenar eminence to receive the prominence of the spinous process without placing undue pressure and causing subsequent discomfort to the patient.16 The patient is encouraged to relax, and the clinician depresses the handle at the foot of the table. If there is no handle, the clinician depresses the foot of the table (pelvic section) by hand. The handle is an improvement over placing the hand on the caudal section of the table because it provides increased leverage and a better stance position for the clinician (Figure 7-7).
The pelvic section is then depressed until the clinician’s hand detects that the musculature has reached a point of tautness and all tissue and joint play have been removed from the area under treatment. This point is maintained, and an additional 2 to 3 inches of table depression is achieved manually. The caudal section is then allowed to return to neutral, followed by another downward movement to the previous point over a 20-second period. This process creates a “pumping action” and is repeated three times, with a break of a few seconds between each 20-second session (Box 7-6).
BOX 7-6 Essential Steps of Flexion-Distraction Treatment
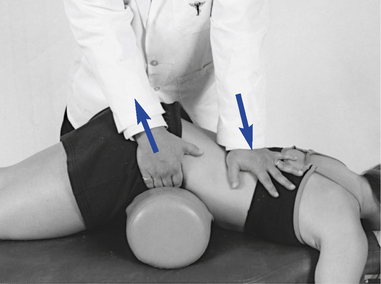
Motorized Lumbar Distraction (Leader Method)
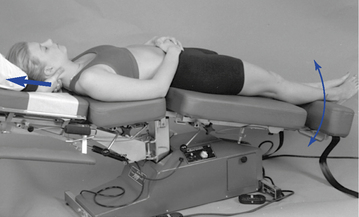
A motorized traction table, such as the Leader table, can be used to assist in the production of lumbar traction (Figure 7-8). Traction to the lumbar spine is applied in the prone position while the pelvic section of the table produces continuous passive motion in the long axis of the spine. The clinician can apply a stabilizing pressure, using both hands over the spinous process of the segment to be distracted to produce a counterpressure against the distractive force produced by the table.
Manual Cervical Traction
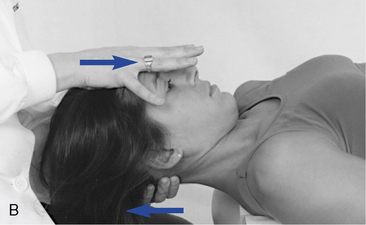
Cervical traction can be applied manually or with mechanical assistance. Manual cervical traction is generally accomplished with the patient in the supine position. The clinician sits or stands at the head end of the table and establishes contacts with the fingers of both hands on the posterior aspect of the cervical spine. Contacts taken over the C5–C6 segment (Figure 7-9, A) will allow the neck to extend slightly to provide more distractive separation and stretch to the anterior structures (the disc and longus coli muscles). Contacts taken under the base of the occiput (see Figure 7-9, B) will allow the neck to flex slightly to provide more distractive separation and stretch to the posterior structures (facets and paraspinal muscles). A towel may be substituted for hand contacts (see Figure 7-9, C).
Motorized Cervical Traction
A motorized traction table, such as the Leader table, can be used to assist in the production of cervical traction (Figure 7-10). Traction to the cervical spine is usually applied in the prone position while the pelvic section of the table produces continuous passive motion in the long axis of the spine. The clinician can apply a stabilizing pressure at the base of the occiput or anywhere in the cervical spine to produce a counterpressure against the distractive force produced by the table’s moving pelvic piece (Box 7-7).
BOX 7-7 Motorized Cervical Traction
Mckenzie method
The McKenzie method is most commonly associated with the promotion and application of lumbar extension exercises for the treatment of low back pain (LBP). Consequently, it is often viewed incorrectly as only a treatment method. The McKenzie method is both an evaluation and treatment approach to the management of painful spinal conditions. It is based on a structured and focused assessment of the effects of repeated movements and sustained postures on a patient’s symptoms and spinal biomechanics. The information gained about the patient’s symptomatic and mechanical responses to loading allows the clinician to determine which specific movements, positions, and activities to either pursue or avoid in the treatment plan. This information is specific to a particular patient at a specific point in time and provides reproducible objective and subjective criteria on which to base clinical decisions. It has been shown to reliably differentiate discogenic from nondiscogenic pain, and a competent from incompetent annulus.17 In comparison with magnetic resonance imaging, it demonstrates superior ability in distinguishing painful from nonpainful discs.17
Treatment principles
The McKenzie approach to treatment is based on the application of mechanical forces and the patient’s symptomatic and mechanical responses to those forces. The central premise is that those movements that decrease or “centralize” the patient’s pain are the movements that should be applied in the treatment of the disorder. Centralization refers to the process of peripheral symptom resolution. With centralization, a patient’s spine pain may persist or temporarily increase. Centralization has been shown to predict a beneficial clinical outcome.18 Increasing symptoms most distal to the spine are known as peripheralization and have been shown to correlate with a loss of competence of the disc annulus18 and predict a poor response to McKenzie treatment procedures. In the McKenzie treatment approach, there is a significant amount of self-applied therapy. The patient learns to appreciate the role of prophylactic procedures from the beginning of treatment and how to interpret which exercises, postures, or activities are beneficial or not. A primary consideration is that all applied procedures should be done in such away that the patient is able to self-treat more effectively. McKenzie19 suggests that clinician-applied forms of spinal manipulative therapy should not be performed on the entire population with back and neck pain, but rather on the minority of patients who have not been able to adequately resolve their symptoms through self-treatment.
Three syndromes: postural, dysfunctional, and derangement
Information obtained through the McKenzie evaluation allows for the classification of mechanical pain into one of three syndromes: postural, dysfunctional, or derangement. Each of the syndromes is considered a unique and separate disorder; however, they often coexist within the same individual. They are distinguished from one another by location of symptoms, presence or absence of acute spinal deformity, and effects of repeated movements and sustained end range positions altering pain patterns.20
The derangement syndrome is a product of anatomic disruption or displacement of the intervertebral segment. Pain may occur immediately with injury or develop over time and is often felt in the midrange of movement. The derangements are divided into one anterior and six posterior categories. Their history and repeated movement examination (Box 7-8) differentiate the three syndromes. Because the three identified syndromes of mechanical pain are separate entities, they each require a different approach to treatment.
BOX 7-8 Characteristics of McKenzie Syndromes
Dysfunctional Syndrome
Treatment of the dysfunction syndrome is directed at remodeling of adaptively shortened structures by stretching maneuvers. The most common pattern of the dysfunction syndrome is loss of spinal extension, except in the upper to middle cervical spine, where flexion is most likely to be limited.21 To achieve the required tissue response, end-range stretching procedures should be performed in a slow, repeated movement in sets of 10 to 15 every 2 hours throughout the day. The presence of significant degenerative changes or stretch irritation to neural structures may make the repetitive rate difficult to tolerate. The involved spinal region and the specific loss of movement pattern determine the movement chosen for treatment. In this case, correction of posture alone is not likely to enhance the lengthening of shortened structures. However, postural dysfunction, if present, must still be addressed because chronic poor posture often leads to tissue shortening and dysfunction. Moreover, when progress is slow or nonexistent, the use of manual procedures or other external forces is introduced. This can include the use of rhythmic end-range mobilizations designed to assist in the phenomenon of creep to lengthen soft tissue. However, these are used to augment, not replace, the exercise program. The repeated movements used in evaluation and treatment of the dysfunction syndrome include flexion, extension, and side-gliding in both the seated and lying positions (Figure 7-12). The treatment exercises will reproduce the patient’s pain, but the increased pain should not persist for prolonged periods after treatment.
Derangement Syndrome
For treatment of the derangement syndrome, a conceptual model of disc pathomechanics must be considered. The model is based on the premise that certain movements can be applied to reduce internal disc derangements and bulging intervertebral discs (IVDs). Movements that are successful in reducing disc protrusion are accompanied by a reduction in the patient’s most distal symptoms (centralization) as the conflict between the protruding disc and associated spinal nerve root is reduced. As symptoms centralize, it is also common for the patient’s repeated ROM to increase with exercise. Using this approach, the suspected derangement patient is directed through a series of movements to ascertain which movements or positions will be most effective in reducing the segmental derangement. The evaluation results in the patient being classified into one of seven derangement categories. The first six derangements are variations of posterior disc disruptions, often requiring extension reductions. In certain instances, coronal plane movements, such as side-gliding (Figure 7-13), or even rotational movements will be required for reduction. The seventh derangement is an anterior disc derangement, requiring a flexion reduction (Figure 7-14).
To complement the use of extension (or flexion) reduction exercises, avoidance of stressful static and dynamic flexion (or extension) postures and activities must be reinforced. These activities often cause peripheralization of the patient’s symptoms, as well as painfully reduced ROMs. Recovery of function is considered complete when full normal repeated weight-bearing flexion produces no more than the expected strain at the end range of all movements.21
Cranial manipulation
Cranial manipulation developed along parallel lines in both the osteopathic and chiropractic professions beginning in the mid- 1930s. Misperceptions and misunderstandings have led to controversy over cranial manipulation. Much of the controversy comes from those who look at the cranium as a fused structure and therefore believe that manipulation has no basis. Cranial manipulation was begun in the chiropractic profession by Cottam and in the osteopathic profession by Sutherland. Both Cottam and Sutherland hypothesized that the cranial bones moved and formed the basis for most cranial techniques. The concept of cranial bone motion, and the therapeutic application of forces on the cranium, is by no means universally accepted. However, the previously held belief that the cranial bones fuse in relatively early life has been shown to be faulty.22 23 24 Although the process of ossification starts in the mid-20s, sutures may remain open throughout life, and some motion flexibility may last into old age.25 The cranial bones are connected and held together by connective tissue called the sutural ligament or membrane, which remains nonossified. Nerve fibers accompany the collagenous connective tissue, although their exact function has not been established.
Practitioners incorporating cranial manipulation purport to be able to palpate a rhythmic (8 to 14 oscillations per minute) cranial movement.26 27 28 However, there have been no interrater reliability studies published. Sutherland called the rhythmic movement within the dural system the primary respiratory mechanism. The pulsations within the dural tube are thought to aid in the circulation of CSF. CSF bathes and nourishes the central nervous system. The potential effects of cranial dysfunction are listed in Box 7-9.
Although the mechanism of cranial movement remains unknown, there is agreement that sutural asymmetry, jamming of the sutures, and pain and muscle tightness can be palpated.25 The evaluation for cranial dysfunction includes observation for skull asymmetries; palpation of skull contours and the sutures themselves to identify widening, narrowing, or tenderness; and determination of the rate, rhythm, and amplitude of the craniosacral mechanism. The goal of cranial manipulation is to improve sutural motion, reduce membranous tension, improve circulation, and increase the vitality of the primary respiratory mechanism. Direct and indirect manipulative procedures have been described for the treatment of cranial dysfunction. Mild forces are used in conjunction with the patient’s breathing pattern.
Soft tissue manipulation
Humans have been performing therapeutic procedures to the soft tissues for as long as humans have been able to touch one another. STM techniques are defined as those physical methods applied to muscles, ligaments, tendons, fascia, and other connective tissues with the goal of therapeutically affecting the body.29 A common source of pain and disability is soft tissue injury with its resultant fibrosis and loss of elasticity and strength. Soft tissue injury and fibrosis may result from acute or repetitive trauma to muscular, tendinous, myofascial, or ligamentous tissue.30 31 32 Although all manual techniques have some effect on the soft tissues, the justification for a separate STM classification is to draw attention to the prime importance of including techniques that have the specific purpose of improving the vascularity and extensibility of the soft tissues.11 One of the signs of joint dysfunction and subluxation is the presence of muscle hypertonicity. Localized increased paraspinal muscle tone can be detected with palpation. Janda33 recognizes five different types of increased muscle tone: limbic dysfunction, segmental spasm, reflex spasm, trigger points, and muscle tightness. Liebenson34 has discussed the treatment of these five types using active muscle contraction and relaxation procedures. Reflex muscle spasm or splinting follows trauma or injury to any of the pain-sensitive structures of the spine. The pain-sensitive spinal tissues include the zygapophyseal joints, posterior ligaments, paravertebral muscles, dura mater, anterior and posterior longitudinal ligaments, and IVD.35 Mechanical deformation or chemical irritation of any of these tissues will cause restricted motion by way of muscle spasm. Treatment directed at the tissue source of pain will reduce the reflex muscle spasm and increase the ROM; however, if the muscle spasm has been present for some time, it may require direct treatment as well.
Visceral disease can also cause reflex muscle splinting. The diagnosis of a viscerosomatic reflex is based on a history of visceral disease or current visceral disease symptomatology and objective palpation findings.36 Objective palpation findings include two or more adjacent spinal segments that show evidence of fixation located within a specific autonomic reflex area; a deep paraspinal muscle splinting reaction; resistance to segmental joint motion; and skin and subcutaneous tissue changes consistent with the acuteness or chronicity of the reflex.36
Effects of soft tissue manipulation
Blood Flow and Temperature Effects
STM has been purported to produce an increase in blood flow and cutaneous temperature. Deep stroking and kneading of the soft tissues in the extremities of normal patients, patients with rheumatoid arthritis, and patients with spasmodic paralysis create a consistent and clinically significant increase in blood flow and cutaneous temperature.37 These findings are supported by other studies.38 39 40 However, it must be emphasized that the clinical procedure being tested in all of these reports was a deep or heavy massage application. Therefore, conclusions on the effects of light-force stimulation of the body wall cannot be drawn from these data.
Massage can induce a fall in blood viscosity, hematocrit count, and plasma viscosity. Ernst, Matrai, and Magyarosy41 found massage to equal pharmacologic agents used to treat blood flow problems. The proposed mechanism may be hemodilation resulting from either an increase in blood plasma volume or reactive hyperemia. Therefore, the effect of massage and circulation appears to be an increased perfusion of blood with plasma fluid, allowing for improved blood flow.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree