5
Nondegenerative Disk Diseases
| Developmental Disturbances | 33 | Involvement of the Intervertebral Disks | |
| Inflammatory and Infectious Disorders | 36 | in Systemic Illness | 37 |
| Tumors | 37 |
 Developmental Disturbances
Developmental Disturbances
Notochord Remnants
The regression of the embryonic notochord can be inhibited at any stage of development, giving rise to a wide variety of structural anomalies of the motion segments. A notochord that persists almost in its entirety appears as a cylinder of soft tissue that passes through the entire length of the vertebral body and widens out in the disk space as a fusiform, intervertebral notochordal swelling. This exceedingly rare anomaly has been described to date only by Schmorl (1932) and Schmorl and Junghanns (1968). A lesser degree of persistence of notochordal tissue produces concave indentations in the dorsal third of the upper and lower end plates, with abnormal thinning of the cortical bone. These are sites where the notochordal canal, which previously traversed the vertebral body, has not closed normally. The overlying cartilaginous end plates, too, are always somewhat thinner than usual. At these sites, disk material may protrude into the spongiosa of the vertebral body, forming so-called Schmorl’s nodes (Schmorl 1932), which are relatively common and are often found incidentally on spinal radiographs. Schmorl’s nodes are an asymptomatic, clinically insignificant finding that should notbe mistaken for spondylitis or vertebral body fractures. Characteristic features of notochord remnants are their location in the posterior third of the upper and lower end plates of the vertebral body and their presence in multiple motion segments (Fig. 5.1).
Developmental Disturbances of the Vertebral Bodies and Intervertebral Disks in Childhood
Persistence of notochord remnants should not be confused with impaired ossification of cartilage at the interface of the vertebral body and intervertebral disk. The latter condition is due to a developmental disturbance during childhood affecting both the vertebral bodies and the intervertebral disks and is mainly seen in their anterior portions. Its cause is not fully understood.
 The high oncotic and hydrostatic pressure of intervertebral disk tissue in children and adolescents can cause it to burst through the cartilaginous and bony end plates at sites of least resistance. The disk tissue destroys growth zones and protrudes into the spongiosa of the vertebral body.
The high oncotic and hydrostatic pressure of intervertebral disk tissue in children and adolescents can cause it to burst through the cartilaginous and bony end plates at sites of least resistance. The disk tissue destroys growth zones and protrudes into the spongiosa of the vertebral body.

Fig. 5.1 Lateral plain radiograph of the lumbar spine in an asymptomatic 20-year-old man. Notochordal regression anomaly with arch-like impressions in the posterior third of the upper and lower end plates.
The severity of the deformity caused by protrusion of the intervertebral disks into the vertebral bodies depends on the size of the protrusions and the stage of development at which they arise. Each region of the spine is affected in its own characteristic way, because the different regions are exposed to different mechanical stresses.
Involvement of the thoracic spine produces the characteristic picture of adolescent kyphosis (Scheuermann disease). The growth of the vertebral bodies is impaired, so that they remain of lesser height ventrally than dorsally; Schmorl’s cartilaginous nodes are seen, and the contours or the upper and lower end plates are irregular. At the same time, the anterior portions of the intervertebral disks are narrowed.
 The abnormal development of the intervertebral disks in Scheuermann disease is a secondary manifestation. It is caused by increased pressure on the disk tissue lying in the anterior portion of the disk space, i.e., in the inner aspect of the kyphosis.
The abnormal development of the intervertebral disks in Scheuermann disease is a secondary manifestation. It is caused by increased pressure on the disk tissue lying in the anterior portion of the disk space, i.e., in the inner aspect of the kyphosis.
As mentioned on page 24 above, an asymmetrical stress on the intervertebral disk causes shifting of fluid and molecules within the disk. In Scheuermann disease, water and dissolved metabolic substrates move from the anterior portion of the disk (on the concave side of the kyphosis) to its posterior portion (on the convex side). With persistent asymmetrical compression, the cells of the anterior portion of the disk receive an inadequate supply of the substrates needed for the generation of disk tissue. As a result, the interstitial, appositional growth of the disk is deficient in this area. Thus, in Scheuermann disease, just as in structural scoliosis, the abnormally shaped intervertebral disks account for a large proportion of the fixed axial deviation of the spine in the sagittal plane.
In the thoracic region, the anterior portions of the intervertebral disks are continually under high mechanical stress and therefore begin to manifest degenerative changes relatively early. The disks age rapidly; they prematurely become partially immobilized in an abnormal posture while the normally loose disk tissue is replaced with fibrous tissue. Particularly in the early stage of adolescent kyphosis, when the spine is still adequately mobile, the goal of treatment should be to optimize the metabolic functioning of disk tissue through a regular alternation of mechanical stress (compression) and relaxation.
In the thoracolumbar junction and the lumbar spine, the developmental structural anomalies occurring at the interfaces of the disks and vertebral bodies differ from those seen in the thoracic spine, because these different regions are subject to different mechanical stresses. The lumbar changes are often referred to as the “lumbar type of Scheuermann disease,” though Scheuermann himself, in 1921, described only changes of the mid- and lower thoracic spine.
Disk herniations into the spongiosa of the vertebral body tend to be larger in the lumbar than in the thoracic spine and to impair the growth of the motion segment in such a way as to cause a considerable degree of deformity. Peripheral portions of the vertebral body may become separated from its main portion by disk tissue, and deep invaginations into the vertebral body may arise (Fig. 5.2).

Fig. 5.2 Juvenile developmental disorder of the lumbar spine in a 12-year-old boy, with deformation of an intervertebral disk and of the adjacent vertebral body end plates. The clinical presentation was consistent with paravertebral muscular insufficiency.
The radiological diagnosis is usually readily apparent from the simultaneous involvement of multiple segments and the reactive growth that is seen in the adjacent vertebral bodies, often in the form of bony protrusions toward the disk space corresponding to invaginations in the opposite end plate (Fig. 5.3).

Fig. 5.3 Juvenile developmental disorder of the lumbar intervertebral disks and vertebrae in an active, asymptomatic female athlete, aged 25.
This type of developmental disturbance has both endogenous and exogenous causes. The cartilaginous end plates of the vertebral bodies contain circumscribed areas of diminished resistance while still in their primordial stage. The very high expansile pressure of the disk tissue, in combination with hydrostatic pressure, damages the growth zone of the vertebral body. Defects arise and are then filled by the expanding disk tissue.
The release of mechanical stress in the axial direction at this site in the disk results in greater than normal bone growth in the ossification layer of the next vertebral body. Its bony end plate therefore develops a bump, or protrusion, pointing in the direction of the disk space. These changes can only arise during development. The importance of mechanical stress on the disk as a cause of these juvenile developmental anomalies is also implied by the fact that they arise in the same regions of the spine that most often sustain compression fractures in accidents involving sudden axial stress.
Though the radiological findings may be quite impressive, one must take care not to ascribe undue importance to them or to cause needless anxiety by communicating them to the patient. The observed deformities often contrast markedly with the patient’s complaints of pain, which are usually localized to other areas of the spine and are most commonly due to the ordinary disk-related disturbances of the lumbar and lower cervical motion segments. In fact, symptoms arising from the deformed disk segments are notably rare. The disk tissue has little tendency to become displaced, because it is anchored to its surroundings by the cartilaginous nodules within the bony spongiosa and by the protrusions of the end plates into the disks.
Although juvenile developmental anomalies of this type generally produce no symptoms in the segments directly affected, they do impair the biomechanical quality of the neighboring intervertebral disks and related structures. Even while the spine is still in its developing phase, these structures cannot withstand the expansile pressure of the disk tissue. It is thus not surprising that disk-related complaints are more common in individuals with this kind of anomaly, as reported decades ago by Alajouanine and Thurel (1949), Kuhlendahl (1953), Hanraets (1959), Brocher (1973), and Idelberger (1984). Mau (1974) found that evidence of dysostotic weakness of the metaphyses was more common in patients with disk herniation than in normal controls. The multisegmentally distributed juvenile developmental anomalies usually cause deviations of the spinal axes in the sagittal and frontal planes; therefore, as a secondary effect, the disks in the adjoining areas of the spine are subject to abnormal and excessive mechanical stress. This is why affected individuals are more than usually subject to intervertebral disk disease.
Congenital Anomalies
The juvenile developmental anomalies discussed above arise during the growth phase, partly under the influence of gravity. In contrast, certain other anomalies of the intervertebral disk are already present at birth. The disk between two vertebrae may be congenitally absent – a “block vertebra.” Incomplete block vertebrae with a markedly attenuated, hypoplastic disk sometimes present difficulties in differential diagnosis; in particular, spondylitis must be ruled out. The diagnosis of a congenital anomaly is supported by the lack of clinical evidence of inflammation; by the concave anterior border of the block vertebra, whose overall size is abnormal compared to the neighboring ones; and by the sharp demarcation of the disk remnants from the vertebral bodies. Congenital anomalies of the disks are not usually accompanied by any areas of bony sclerosis or bony defects in the vicinity of the end plates, but the laminae and spinous processes are often fused. The motion segments corresponding to the block vertebrae do not give rise to any symptoms, even when their neural foramina are markedly narrowed or occluded with bone. This painless block state is analogous to the desired result of spinal fusion procedures. The congenital fusion of two adjacent vertebrae can, however, produce painful functional disturbances of the motion segments above and below, which are subject to increased mechanical stress. This is particularly true when the vertebrae are fused in an abnormal position.
Partial anterior block formation over multiple segments is not a congenital anomaly but, rather, a result of Scheuermann disease or of severe senile kyphosis of the thoracic spine.
 Inflammatory and Infectious Disorders
Inflammatory and Infectious Disorders
Bacterial Infection of the Intervertebral Disk
Bacterial infection is a relatively rare but nonetheless important cause of intervertebral disk disease. It is easily overlooked, particularly in its early stages, because degenerative diseases are much more common.
Bacterial infection of the disk can be caused by specific pathogens (e.g., the tubercle bacillus) or by nonspecific ones (staphylococci, streptococci, E. coli, and others). Nonspecific infections arise most commonly in the lumbar motion segments. Infection with Gramnegative organisms (E. coli, Bacillus proteus) has recently become more common. Isolated discitis without primary involvement of the vertebral body is caused by direct entry of the pathogenic organism into the disk, usually as a complication of a medical procedure such as discotomy or disk puncture. Hematogenous discitis is theoretically possible only when there are blood vessels within the intervertebral disk, i.e., only in infants and in old people with advanced degenerative disk disease.
Schmorl (1932) found very few cases of primary hematogenous disk infection in his extensive clinical series. In one such case, for example, an abscess developed in the nucleus pulposus of a vascularized second lumbar disk in a patient with tonsillitis complicated by bacterial sepsis.
Most of the “primary disk infections” in adults that have been reported in the literature are, in fact, more likely to have been secondary to vertebral body infection in the vicinity of the end plates (a condition that often cannot be seen on plain radiographs and can only be diagnosed by tomography). Bacterial infection of the disk itself is radiographically characterized by narrowing of the disk space and by subchondral end plate defects with a surrounding sclerotic zone. Unlike Schmorl’s nodes, the sclerotic zones around foci of infection are not sharply demarcated; rather, they extend far into the vertebral spongiosa, without any clear border. The vertebral body end plates above and below the infected disk also appear to be unfocused, with blurred contours. Bacterial infection of the disk can spread cranially and caudally beneath the anterior longitudinal ligament and give rise to an extensive, spindle-shaped abscess. Disks at neighboring levels can also be secondarily infected in this way. Paravertebral abscesses in the lumbar region can spread along the psoas sheath, causing a widening of the psoas shadow in a plain radiograph.
Disk infection is difficult to diagnose in its early stages because plain radiographs often show no change beyond a mild narrowing of the disk space. Scintigraphy may reveal increased local activity, but the main diagnostic criteria are clinical: a history of recent infection elsewhere in the body (tonsillitis/pharyngitis, furuncle, abscess), fever, and localized back pain on manual pressure or shaking of the spine. Laboratory testing, CT, and plain tomograms confirm the diagnosis. Later on in the course of disk infection, one may see bony bridges traversing the disk space, a characteristic finding. The radiological distinction between specific and nonspecific intervertebral disk infections is usually only one of degree. Nonspecific infection more commonly takes a fulminant course and shows a more marked bony reaction, with the formation of wide bony bridges and sclerotic areas (Fig. 5.4).
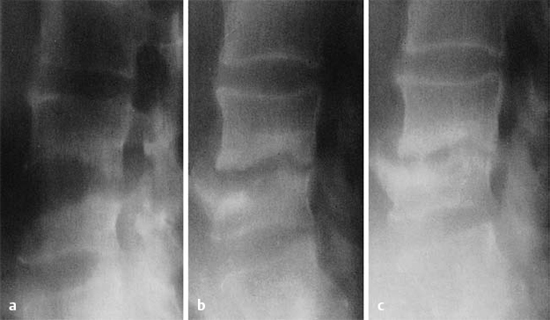
Fig. 5.4a–c Nonspecific spondylitis at L4/L5 in a 62-year-old man. At first, there is spondylodiscitis with loss of vertebral body bone opacity (a); within a few months, the bone consolidates and develops large spondylotic processes (b, c).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





