Fig. 5.1
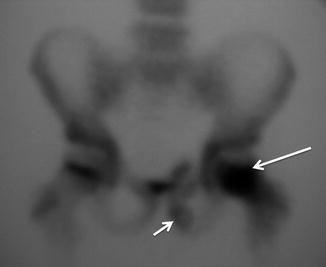
Fig. 5.2
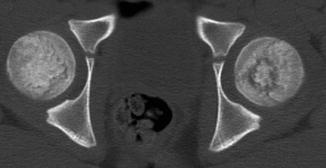
Fig. 5.3
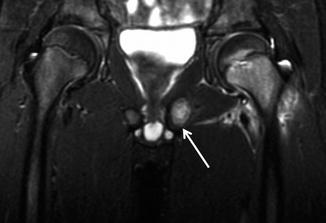
Fig. 5.4
A 9-year-old child complaining of left hip pain (restricting his soccer activities) for 3 weeks. Four weeks previously, he had suffered an abdominal superficial injury requiring subcutaneous sutures. At admission, the patient presented with intermittent fever. He had an abnormal gait and was reluctant to weight bear. A plain pelvic radiograph in the emergency room was suggestive of a left ischial bone tumor. CT, bone scintigraphy, and MRI examinations were requested.
Comments
Acute hematogenous osteomyelitis usually occurs during skeletal growth while the physis is open. Early detection is essential to start appropriate therapy before bone devitalization.
Plain x-ray manifestations may not be demonstrable for at least 10 days after onset of symptoms. The infection’s evolution can show soft-tissue swelling with adjacent muscle plane obliteration, subperiosteal calcification, and bony trabecular resorption.
Bone scintigraphy is a highly sensitive procedure for diagnosing osteomyelitis. It gives a sensitive indication of altered osteoblastic activity; however, local disturbances in vascular perfusion, clearance rate, permeability, and chemical binding also affect imaging.
CT should be used as a third-line technique for visualizing bony destruction/sequestration and gas in the bone. MRI is a highly sensitive technique as a disease indicator since pathologic findings appear much earlier. The diagnosis of osteomyelitis on MRI is given by physeal bone marrow abnormalities. Active osteomyelitis appears as a low signal on T1-weighted images and a high signal on T2-weighted images, fat suppression, or STIR sequences. MR imaging is unique in being able to detect the presence of osteomyelitis and also in determining its extent.
Understanding each technique’s limitations is important in order to avoid delays in the diagnosis and management of osteomyelitis and to prevent possible complications.
The differential diagnosis of pelvic osteomyelitis in children should include septic arthritis, Legg-Calve-Perthes disease, toxic synovitis, and, less commonly, collagen vascular diseases, neoplasms involving bone, or retroperitoneal abscess.
Radiological Findings
Plain pelvic radiography (Fig. 5.1) does not reveal pathologic findings suggestive of bone infection in the left femur. Incidentally a left swollen ischiopubic synchondrosis (arrow) was noted, which was initially thought to be responsible for the patient’s symptoms. A bone scintigraphy scan (Fig. 5.2) shows increased uptake within the left femoral head (large arrow) and slight uptake on the left ischiopubic synchondrosis (short arrow).
CT imaging (Fig. 5.3) shows a round annular area in the left femoral head corresponding to the focal site of infection.
Coronal STIR MR imaging (Fig. 5.4) reveals femoral bone marrow high-intensity signal especially within the physis, with edema on the surrounding soft tissues. Note the ischiopubic synchondrosis hypertrophy (arrow).
Case 5.2: Adventitial Cystic Disease of the Radial Artery

Fig. 5.5
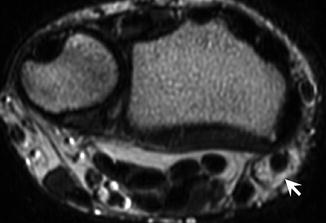
Fig. 5.6
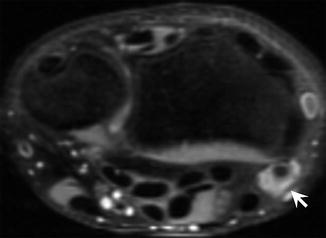
Fig. 5.7
A 17-year-old hockey player presented with recurrent pain in anatomical snuffbox after trauma 6 months ago.
Comments
Arterial adventitial cystic disease is an uncommon type of non-atherosclerotic peripheral vessel disease of unknown etiology. Several theories about their pathogenesis have been proposed such as repetitive trauma, embryological origin, direct communication with the herniated synovial structures of the adjacent joint and connective tissue disease. It affects most commonly the popliteal artery (85 % of cases), typically in young to middle-aged men without significant vascular risk factors, with a male-to-female ratio of 15:1. However, involvement of other arteries like axillary, brachial, radial, ulnar, external iliac, and common femoral has also been reported. Rarely, it can also affect the veins.
Clinically this condition results in intermittent claudication due to peripheral vascular insufficiency caused by compression of the arterial lumen by a cystic collection of mucinous material in the adventitial layer of the artery.
Magnetic resonance imaging (MRI) with magnetic resonance angiography (MRA) is very helpful in the diagnosis, as it provides excellent anatomical detail with cysts appearing as hyperintense structure on T2WI images, and luminal compromise can also be assessed.
It is an important treatable cause of vascular disease with multiple therapeutic options, which include restore arterial flow, resection of the affected artery and interposition grafting, percutaneous aspiration of cystic contents under ultrasound, or CT guidance and resectional adventitial cystotomy.
Radiological Findings
Post-contrast coronal MIP (maximal intensity projection) image from upper extremity contrast-enhanced MR angiography (Fig. 5.5) demonstrates focal narrowing of the radial artery (long arrow). The remaining vasculature is normal.
Case 5 3: Transient Lateral Patellar Dislocation
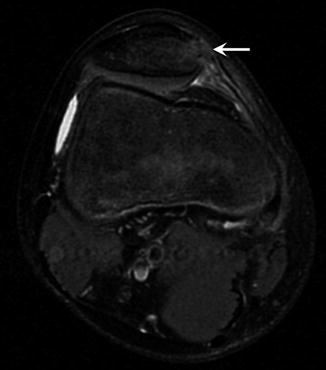
Fig. 5.8
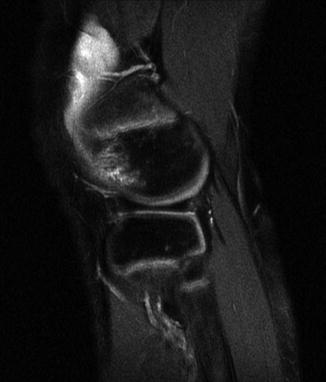
Fig. 5.9

Fig. 5.10

Fig. 5.11
A 13-year-old soccer player suffered a painful partial patellar dislocation while running backwards and twisting to kick the ball. The patellar subluxation reduced spontaneously. On examination, there was no ACL (anterior cruciate ligament) instability, although knee pain was persistent after the traumatic event.
Comments
Acute lateral patellar dislocation (LPD) occurs often in children during sporting activities and is commonly transient with spontaneous reduction. It accounts for approximately 9–16 % of acute knee trauma in young athletes presenting with hemarthrosis. The mechanism of injury usually involves a twisting motion: fixed foot and internal rotation on a flexed knee with valgus stress. Spontaneous relocations occur in the majority of patients. Between 50 and 75 % of diagnosis go unsuspected after clinical exam and initial plain radiology evaluation. Differentiation from other knee injuries is often difficult as extensive tenderness, hemarthrosis, and pain are often present.
Radiographs may show hemarthrosis, and a minority of patients will have a patellar chip fracture. Concomitant injuries, including medial patellofemoral ligament injuries, are common, occurring in up to 90 % of patients.
Magnetic resonance (MR) imaging findings may include typical contusion patterns in the patellar inferomedial pole and the anterolateral aspect of the femur’s nonarticular portion (kissing sign) with injury to the medial patellar soft-tissue restraints. Up to one third of patients will also show concomitant injury to the major knee ligaments or menisci. These are frequently associated with osteochondral fractures, which may be an indication for surgery.
Trauma alone rarely causes patellar dislocations in patients without predisposing anatomical factors for patellar instability, such as trochlear dysplasia, dominant lateral patellar facet, high riding patella and tibial tuberosity lateralization. Trochlear dysplasia is found in up to 85 % of patients with LPD.
Nonsurgical management is generally recommended for first-time dislocations, with brace immobilization in extension for 3–6 weeks. Following initial conservative management, recurrent instability occurs in 15–50 % cases. Chronic instability and recurrent patellofemoral dislocations may cause cartilage damage with bone soft-tissue restraint abnormalities and eventual arthritic changes. Surgery may be indicated when associated injuries or abnormal patellofemoral relationships are identified.
Radiological Findings
Axial (Fig. 5.8) and sagittal (Fig. 5.9) proton density-weighted images with fat suppression reveal focal bone marrow edema involving the patellar medial aspect (arrow) and the lateral femoral condyle’s lateral aspect. A medial patellar retinaculum high signal is visible without tearing. Note the trochlear dysplasia and the minimal joint effusion. Coronal T1- (Fig. 5.10) and coronal T2-GE-weighted (Fig. 5.11) MRI demonstrate focal bone marrow edema involving the medial femoral condyle with a hyperintense signal along the superficial aspect of the medial collateral ligament (MCL) (sprain grade I).
Case 5.4: Normal Knee Ossification Variants

Fig. 5.12

Fig. 5.13

Fig. 5.14

Fig. 5.15
A 7-year-old boy injured himself (internal varus mechanism) during a soccer match. He presented with bilateral knee pain (occasionally locking and more pronounced on the right) with questionable meniscal positive test. Two days later, he was asymptomatic. A magnetic resonance imaging exam was performed to exclude osteochondritis dissecans.
Comments
Marginal ossification center irregularities in the distal femoral epiphyses are extremely common in children during normal skeletal maturation, showing a high rate of bilaterality. There are four different knee ossification variants: puzzle piece (completely filled by bone), partial puzzle piece (partially filled by bone), spiculated configuration with an irregular subchondral bone plate, and extra ossification centers within the non-ossified physeal cartilage that remain separated from the condyle’s ossified part. These variants may occur in the posterior aspect of the maturing femoral condyle. A subchondral bone plate focal defect results if the variant is embedded within the epiphysis’ already ossified part.
Often the irregularities take a form roentgenographically indistinguishable from osteochondritis dissecans (OCD). OCD is an acquired, potentially reversible subchondral bone disorder that can secondarily affect the overlying articular cartilage and, in some cases, may lead to cartilage separation and fragmentation. The typical symptoms are pain, swelling, stiffness, locking, and clicking. Accessory ossification centers, on the other hand, do not cause any clinical symptoms and do not require treatment.
Magnetic resonance imaging provides several helpful key points distinguishing normal ossification variants from stage I OCD. Features of normal variants are infero-central defect location in the posterior femoral condyles with intact overlying articular cartilage, the presence of accessory ossification centers, lesion angle measurement <105º, spiculations, residual physeal cartilage, and lack of joint effusion and bone marrow edema. Osteochondritis dissecans MRI features have been discussed in Chap. 4 (Case 4.6).
Radiological Findings
Right knee sagittal T1-weighted MRI (Fig. 5.12) demonstrates an OCD-like lesion (arrow) in the femoral condyle’s posterolateral aspect. A corresponding sagittal fat-suppressed T2 (Fig. 5.13) view shows a normal overlying articular cartilage and lack of bone marrow edema.
A left knee coronal T2-weighted sequence (Fig. 5.14) shows a posterolateral femoral condyle irregularity (arrow). Sagittal fat-suppressed fast spin-echo T2-weighted MR image (Fig. 5.15) demonstrates the normal knee maturation anatomy: heterogeneous signal intensity (SI) of non-ossified posterior femoral condyle (long arrow), hyperintense signal of organized articular cartilage (short arrow), and relative hypointense signal in the less organized hyaline cartilage of the non-ossified epiphysis.
Case 5.5: Lateral Discoid Meniscus with Incidental Fibrous Cortical Defect

Fig. 5.16

Fig. 5.17

Fig. 5.18
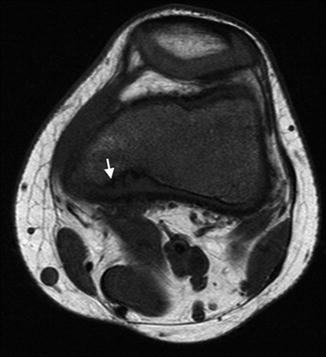
Fig. 5.19
An 8-year-old girl basketball player presented with chronic knee pain more intense while playing, with the sensation of blocking occasionally. No traumatic history was reported. At physical examination, a lateral meniscal tear was suspected.
Comments
A discoid lateral meniscus (DLM) is a common variant of normal meniscal morphology, which is usually C shaped. The enlarged body of the meniscus extends medially toward the intercondylar notch and covers the articular surface of the tibial plateau, considering three types of DLM in arthroscopy: complete, incomplete (50–80 % of coverage), and the Wrisberg variant (complete or incomplete with no capsular attachments). Their prevalence is between 0.4 and 17 % depending on the authors. It occurs on the lateral side of the knee in about 1–3 % of the population and even less commonly on the medial side of the knee. It is bilateral in up to 20 % of cases.
Magnetic resonance imaging (MRI) provides a precise identification of the lesion. According to Silverman et al., criteria for adult knees are the presence of three or more 5-mm thick contiguous sagittal images showing continuity of the anterior, and posterior horns of the meniscus are suggestive for a discoid lateral meniscus. In children, particularly those younger than 10 years should be used a ratio of lateral tibiofemoral joint space coverage. If the meniscus occupies greater than 50 % of the lateral tibiofemoral joint space, a discoid lateral meniscus should be considered. Unlike adults, children frequently present symptoms: projection on bending the knee, pain, and reduction in the range of movement. The discoid meniscus is more susceptible than normal to mechanical forces due to its thickness, hypermobility, poor vascularization, and a weak attachment of the posterior area to the capsule.
Surgical treatment is necessary in symptomatic cases, with satisfactory results following arthroscopic partial resection.
Radiological Findings
Sagittal fat-suppressed T2-weighted image and coronal STIR image (Figs. 5.16 and 5.17) show an abnormally large and thick lateral meniscus (arrow) with internal increased signal due to mucinous degeneration. The abnormal signal does not reach the articular surface (Fig. 5.17). Coronal STIR (Fig. 5.17) also demonstrates the body of the lateral meniscus extending into the intercondylar notch, consistent with complete discoid meniscus. Note the normal shape and size of the medial meniscus. Incidental fibrous cortical defect is seen on the medial condyle with hyperintense signal (arrow) on sagittal fat-suppressed T2-weighted image (Fig. 5.18) and hypointense on axial T1-weighted image (Fig. 5.19) outlined by a thin rim of sclerosis (arrow). Fibrous cortical defect and non-ossifying fibroma are discussed in length within Case 5.7.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








