Large and Massive Rotator Cuff Tears
BIOMECHANICS OF LARGE AND MASSIVE ROTATOR CUFF TEARS
The goal of arthroscopic rotator cuff repair is to anatomically repair the rotator cuff with a biomechanically sound construct while respecting the biology of the tissues. While historically these principles have largely been adhered to, in some instances heroic measures have been undertaken to “close the defect.” These have included large tendon transfers (e.g., subscapularis tendon transfer, latissimus dorsi transfer), allograft or autograft transplantations (e.g., fascia lata), and aggressive slides and elevations (e.g., supraspinatus slide). Although in rare cases these procedures may provide some benefit, in many instances a biomechanically sound repair without complete closure of the defect may suffice, that is, a partial rotator cuff repair.
The major function of the rotator cuff is to compress and depress the humeral head into the glenoid to provide a stable fulcrum of glenohumeral motion. For this to occur, the rotator cuff must be balanced in the transverse (axial) and sagittal planes (Fig. 7.1). With a stable fulcrum of glenohumeral motion, the major muscle movers of the shoulder (i.e., deltoid, pectoralis major, latissimus dorsi) can exert their moments about the shoulder, providing global functional motion.
With a significant rotator cuff tear, the transverse and/or sagittal plane force couples are no longer balanced, resulting in an unstable fulcrum of motion and painful dysfunction of the shoulder (Fig. 7.2). However, not all rotator cuff tears will result in an unstable fulcrum of motion with pain and disability. In fact, many tears, particularly those in the avascular crescent region of the rotator cuff (i.e., supraspinatus tendon and anterior half of the infraspinatus tendon), may be minimally symptomatic with relatively preserved strength. This is due to the ability of the torn rotator cuff to transmit a distributed load to the humeral head by utilizing the cable region of the rotator cuff, an anatomic thickening of the rotator cuff.
The rotator cable is an anatomic thickening of collagen fibers within the rotator cuff, seen best arthroscopically (Fig. 7.3) and is formed anatomically by an extension of the coracohumeral ligament. This cable extends from a bifurcated insertion on both sides of the long head of the biceps tendon and continues posteriorly to the inferior margin of the infraspinatus (Fig. 7.4). Enclosed within the arc of the rotator cable is the classical crescent region of the rotator cuff, the area where the majority of rotator cuff tears begin. When a rotator cuff tear occurs in this region, the muscle may still exert its force on the humeral head through the rotator cable in much the same way that a suspension bridge exerts its force through a distributed load from its cable to its columns (Fig. 7.5). Because of this preserved function, most tears that are contained within the rotator cable region will still have a stable fulcrum of motion, preserved clinical motion, and minimal strength deficit on manual muscle testing.
In contrast, tears that extend through the rotator cable attachments usually will result in an unstable fulcrum, loss of motion, and significant strength deficit. This clinical picture generally conforms anatomically to tears extending anteriorly into the upper half of the subscapularis tendon or posterior tears that extend through the inferior half of the infraspinatus tendon. This has led to the conventional wisdom that, although single-tendon tears may have preserved function or even be asymptomatic, tears extending into a second tendon are usually poorly tolerated.
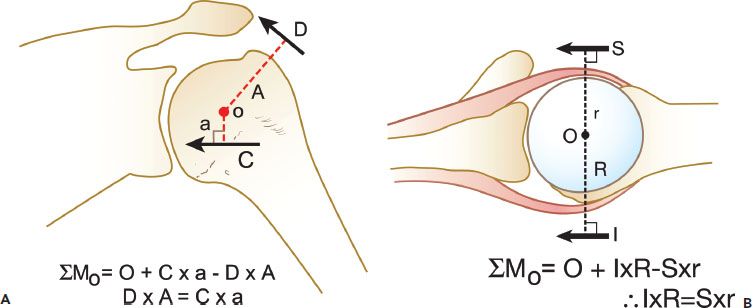
Figure 7.1 Balanced force couples are required to maintain the normal glenohumeral relationship. A: In the coronal plane, the combined inferior rotator cuff force (C) is balanced against the deltoid (D). B: In the transverse plane, the subscapularis (S) is balanced against the infraspinatus and teres minor (I). O, center of rotation; A, moment arm of the deltoid; a, moment arm of the inferior rotator cuff; r, moment arm of the subscapularis; R, moment arm of the infraspinatus and teres minor.
The consequence of the cable-crescent architecture in patients with massive rotator cuff tears is that, if a complete repair is not possible, a partial repair focusing on reattachment of the subscapularis and infraspinatus tendons can provide significant clinical improvement due to restoration of the cable attachment, preservation of rotator cuff function, restoration of balanced force couples, and reestablishment of a stable fulcrum of motion. This principle respects the natural anatomy and biomechanical function of the rotator cuff and precludes the natural tendency to simply “close the defect” using the heroic measures as described above.
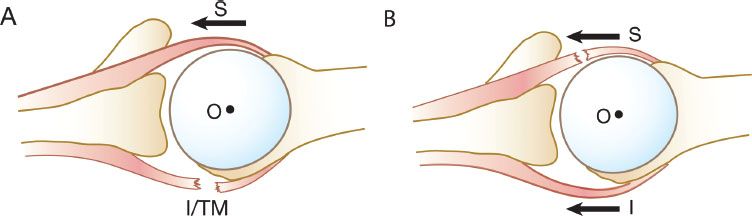
Figure 7.2 A: The transverse plane force couple is disrupted because of a massive rotator cuff tear involving the posterior rotator cuff (infraspinatus and teres minor). B: An alternative pattern of disruption of the transverse plane force couple. The transverse plane force couple is disrupted by a massive tear involving the anterior rotator cuff (i.e., subscapularis). I, infraspinatus; TM, teres minor; O, center of rotation; S, subscapularis.
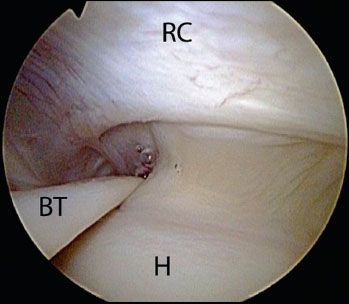
Figure 7.3 Arthroscopic view of a right shoulder demonstrating a cablelike thickening of the capsule surrounding a thinner crescent of tissue that inserts into the greater tuberosity of the humerus. BT, biceps tendon; H, humerus; RC, rotator cuff.
TEAR PATTERNS
Clearly, if a complete rotator cuff repair is possible, this is more desirable than a partial rotator cuff repair. Furthermore, a complete rotator cuff repair that respects the natural mobility of the tear will inherently result in a low-tension, anatomic repair. For this reason, it is critical to exhaustively evaluate the medial-to-lateral and anterior-to-posterior mobility of the tear margins. That is to say, if a tear may be repaired from a medial-to-lateral direction (i.e., crescent-shaped tear) or by an anterior-to-posterior margin convergence technique (i.e., U-shaped, or reverse-L-shaped tears), then it should be performed. A complete anatomic rotator cuff repair will result in restoration of the cable region with resultant improvement in function.
In severe chronic cases, particularly cases in which the margins of the rotator cuff are scarred to the internal deltoid fascia (e.g., massive adhesed immobile rotator cuff tears), there may be no mobility from a medial-to-lateral and an anterior-to-posterior direction. This precludes repair by direct tendon to bone repair or by margin convergence. These cases represent approximately 10% of massive rotator cuff tears and repair in such cases may be attempted using interval slide techniques.
ADVANCED RELEASES FOR THE ROTATOR CUFF
In clinical practice, rotator cuff tears may present with a wide spectrum of size and mobility. Although a tear may be massive in size, the necessity for complex releases is purely dependent on its inherent mobility. Many massive rotator cuff tears may be reparable without releases after proper evaluation of their natural mobility. This natural mobility defines its tear pattern and therefore its repair pattern. In contrast, some small rotator cuff tears may require releases particularly in the presence of concurrent disorders (e.g., adhesive capsulitis or revision surgery). When a tear can be anatomically reduced to the footprint, advanced releases are not required and can unnecessarily increase the complexity of the procedure.
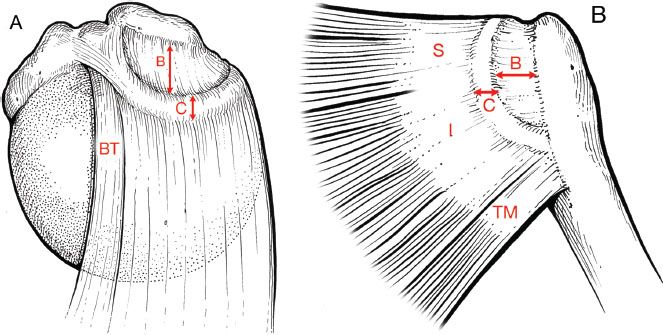
Figure 7.4 Superior (A) and posterior (B) projections of the rotator cable and crescent. The rotator cable extends from the biceps to the inferior margin of infraspinatus, spanning a crescent-shaped area of tendon composed of the supraspinatus and half of the infraspinatus insertions. The cable inserts into the humerus posteriorly at the lower margin of the infraspinatus. C, width of rotator cable; B, mediolateral dimension of rotator crescent; S, supraspinatus; I, infraspinatus; TM, teres minor; BT, biceps tendon.
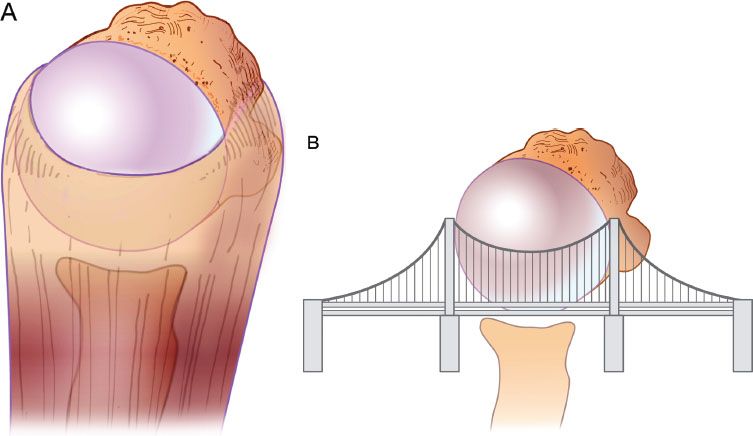
Figure 7.5 A rotator cuff tear (A) can be modeled after a suspension bridge. B: The free margin corresponds to the cable, and the anterior and posterior attachments of the tear correspond to the supports at each end of the cable’s span. A preserved rotator cable can exert a compressive force sufficient to stabilize the humeral head in the setting of a large rotator cuff tear.
Rotator cuff releases may be divided into bursal-sided releases, articular-sided releases (i.e., capsular releases), and interval slides (see “Bonus Videos,” Disc 2). Releases associated with the subscapularis tendon are covered in Chapter 6.
ARTICULAR-SIDED RELEASES—THE CAPSULAR RELEASE
When a rotator cuff tear will not quite reach the bone bed, or is reducible to the bone bed only with significant tension, a capsular release may provide sufficient mobility for tension-free repair to bone. In most scenarios, capsular release is most beneficial in crescent-type tears where the direction of repair is generally from a medial-to-lateral direction. Capsular release generally provides 1 to 1.5 cm of additional mobility.
When performing a capsular release for increasing mobility of the tear margins, one must be cognizant of the proximity of the suprascapular nerve. The suprascapular nerve lies approximately 1.5 to 2.0 cm medial to the glenoid rim and therefore any releases should not be performed more than 1 to 1.5 cm medial to the glenoid rim. By applying traction to the margins of the rotator cuff tear, the rotator cuff and capsule can be lateralized and therefore increase the margin of safety when performing a capsular release.
When performing a capsular release, it is easiest to view through a lateral portal. One or two traction sutures are placed along the margin of the rotator cuff tear using a Scorpion (Arthrex, Inc., Naples, FL) suture passer. The traction stitches are retrieved through lateral stab incisions that are created close to the edge of the acromion. In this fashion when traction is applied, it draws the tendon laterally and superiorly to improve access to the medial capsule. In some cases, a switching stick or grasper may be used to “lift” the rotator cuff away from the glenoid labrum to further maximize visualization.
Using a combination of an elevator and pencil-tip electrocautery, the medial capsule underneath the margin of the rotator cuff and just above the glenoid labrum is carefully incised. It is important to incise the capsule completely until the muscular fibers of the rotator cuff are exposed to ensure maximum tendon excursion. The rotator cuff margin can then be reassessed for mobility. If sufficient mobility is obtained for tendon repair to bone, rotator cuff repair may proceed. However, if inadequate mobility is obtained, then one may proceed with interval slides.
INTERVAL SLIDES
The need for interval slides is based upon the mobility of the rotator cuff tendon margins. Many U-shaped and L-shaped tears, despite their size, have adequate mobility and may be repaired using the principles of margin convergence. Understanding and elucidating tear patterns is one of the most important principles of successful performance of routine arthroscopic rotator cuff repair.
When a tear has been determined to be irreparable despite standard capsular release, proceeding with interval slides to improve mobility should be considered. The decision is based upon patient age, patient symptoms (i.e., pain vs. weakness), tissue quality, and initial tear mobility. Young patients, with a primary complaint of weakness, who have adequate tissue quality and moderate tear mobility, should be strongly considered for interval slides. In contrast, older patients (e.g., age >70), with a primary complaint of pain, who have poor tissue quality, and minimal to no medial-to-lateral mobility may be candidates for a partial repair or for debridement alone. This is particularly relevant when a prolonged rehabilitation program may be poorly tolerated or in patients with >75% fatty atrophy on MRI.
Two slides are relevant to repairs of the posterosuperior rotator cuff: the anterior interval slide and the posterior interval slide. The anterior interval slide is a release of the anterior leading edge of the supraspinatus from the rotator interval and can improve mobility of the rotator cuff by approximately 2 cm. This same release can be accomplished without dividing the tissue adjacent to the anterior leading edge of the subscapularis. This is done by using an elevator to lyse the underlying soft tissue attachments to the coracoid base. This is called an anterior interval slide in-continuity, and we prefer this method when an anterior interval slide is indicated. In contrast, the posterior interval slide is a release of the posterior edge of the supraspinatus from the infraspinatus and can also increase mobility by a further 2 to 4 cm.
When only one release is performed, this is commonly referred to as a single-interval slide, whereas when both releases are performed, this is referred to as a double-interval slide. Although classically the anterior interval slide is performed prior to the posterior interval slide, choosing which slide to perform first and whether a single or a double-interval slide is necessary is based upon the tear mobility. In general, the releases are performed first in the location with the most severe restriction of mobility. If sufficient mobility may be obtained with a single release, this may be advantageous since the residual flaps of rotator cuff are larger and more robust than if a second release is performed. A second release is performed only if insufficient mobility is obtained with the initial release.
If the tendon mobility is equally restricted anteriorly and posteriorly, then the arthroscopist may perform either release first. However, in general, the authors have noted that the posterior interval slide provides more mobility than the anterior interval slide, and importantly improves mobility of both the supraspinatus and infraspinatus. Many times, only a posterior interval slide is required and will provide sufficient mobility for repair of both the supraspinatus and infraspinatus. Furthermore, maintaining the continuity of the leading edge of the supraspinatus to the rotator interval facilitates repair of the anterior rotator cuff.
The keys to expedient and effective use of interval slides are exposing the critical landmarks, utilizing the correct angle of approach, and employing traction stitches appropriately. Standard anterior, posterior, and lateral subacromial portals will have already been established. A posterolateral viewing portal is also created. A complete subacromial bursectomy should be performed. Formal subacromial decompression with release or excision of the coracoacromial ligament is not performed to avoid the risk of iatrogenic anterosuperior escape.
THE BONY LANDMARKS
In doing interval slides, the two key bony landmarks are the scapular spine and the base of the coracoid. The scapular spine is easiest to identify while viewing through the lateral portal. Using a combination of a shaver and cautery through the posterior portal, the undersurface of the acromion is debrided. As the exposure is continued posteriorly and medially, the scapular spine may be identified as a keel-shaped structure, posterior to the acromioclavicular joint (Fig. 7.6). In cases of massive rotator cuff tears, the scapular spine is actually easier to identify than in cases with an intact cuff where the bulk of the rotator cuff muscle may obscure medial visualization. Exposure of the scapular spine should proceed inferiorly toward the glenoid. Exposure should be carefully performed due to risk of injury to the suprascapular nerve, and should stop upon reaching the tendinous bridge of tissue connecting the infraspinatus and supraspinatus. Exposure of the scapular spine is vital to performing posterior interval slides since this keel-shaped structure delineates the interval between the supraspinatus and infraspinatus tendons.
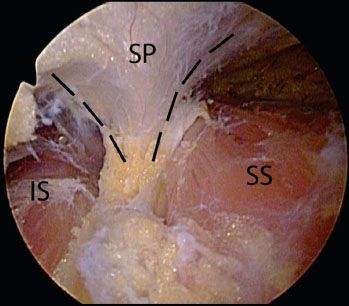
Figure 7.6 Arthroscopic view of the scapular spine in a right shoulder viewed from a lateral portal. The scapular spine (outlined by dashed black lines) defines the margin between the supraspinatus (right) and the infraspinatus (left). IS, infraspinatus; SP, scapular spine; SS, supraspinatus.
The second key bony landmark is the coracoid base. It is easiest to identify this landmark while viewing through the lateral portal. Using an accessory lateral portal, a switching stick or similar instrument is used to palpate the coracoid base. The coracoid base can be palpated as a bony prominence just anteromedial to the biceps root. Although one may choose to formally expose the coracoid base, this is usually not required and only its location needs to be identified. The coracoid base is critical to discern the location and direction of the anterior interval slide.
TRACTION STITCHES
Once the bony landmarks have been identified, tractions stitches are placed through the supraspinatus and infraspinatus tendons. Generally speaking, one stitch is placed at the anterior leading edge of the infraspinatus tendon and another stitch is placed in the midpoint to posterior leading edge of the supraspinatus tendon. Traction stitches are critical and should be used routinely. Differential tensioning of the traction stitches can help align the interval to the arthroscopic scissor during release and can spread apart the interval during release to maximize visualization.
While viewing through a posterolateral portal, an antegrade suture-passing instrument is introduced through the lateral portal (e.g., Scorpion) and a #2 FiberWire (Arthrex, Inc., Naples, FL) stitch is placed through the supraspinatus tendon. The supraspinatus traction stitch is then retrieved through an anterior portal. A second traction stitch is similarly placed through the infraspinatus tendon (Fig. 7.7). As an alternative to an antegrade pass, a retrograde suture-passing instrument (e.g., Penetrator; Arthrex, Naples, FL) can be used. The Penetrator is preloaded with a traction stitch (usually of a different color (e.g., #2 TigerWire; Arthrex, Inc., Naples, FL). The Penetrator is first used to pass a suture loop through the infraspinatus tendon. The Penetrator is then carefully retracted back out of the infraspinatus tendon leaving the suture loop in situ. The suture loop can then be retrieved by the Penetrator, completing passage and retrieval of the traction stitch.
POSTERIOR INTERVAL SLIDE
It is easiest to perform the posterior interval slide while viewing through a lateral or posterolateral subacromial portal. The traction stitches are retrieved through corresponding portals to spread the posterior interval apart—the supraspinatus traction stitch through an anterior or anterolateral portal and the infraspinatus traction stitch through a posterior or posterolateral portal (Fig. 7.8).
A spinal needle is used to identify the correct angle of approach in line with the posterior interval and toward the spine of the scapula. An arthroscopic scissor is then introduced through the accessory portal and begins the posterior interval slide along the lateral margin of the rotator cuff tendon directing the incision toward the base of the scapular spine. By using a combination of straight or curved arthroscopic scissors, the release is continued toward the base of the scapular spine (Fig. 7.9A). Instead of an accessory working portal, one may view through a posterolateral portal and use the scissors through a lateral portal, or vice versa. When performing the slide, it is critical to place traction on both the anterior supraspinatus tendon stitch and the posterior infraspinatus tendon stitch to spread the tissues apart as the release progresses, facilitating release and maximizing visualization of the apex of the release. Furthermore, differential tensioning of the traction stitches can help position the interval in line with the arthroscopic scissors.
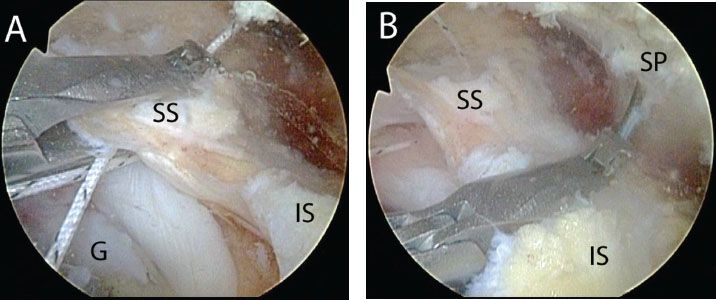
Figure 7.7 Arthroscopic view of a left shoulder viewed from a lateral portal demonstrating (A) placement of a traction stitch in the supraspinatus, and (B) placement of a traction stitch in the infraspinatus. G, glenoid; IS, infraspinatus tendon; SP, scapular spine; SS, supraspinatus tendon.
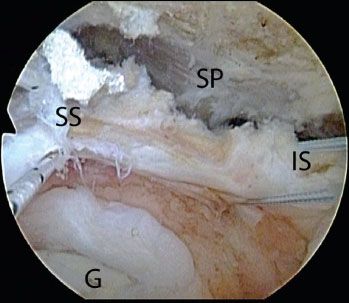
Figure 7.8 Arthroscopic view of a left shoulder viewed from a lateral portal showing traction sutures placed in preparation for a posterior interval slide. G, glenoid; IS, infraspinatus tendon; SP, scapular spine; SS, supraspinatus tendon.
When performing the release, it is important to incise the tissue full thickness as it can sometimes appear as though there are two separate layers. Failure to do so will result in an incomplete release and insufficient mobility. The release is continued toward the scapular spine until the fat pad lateral to the bony spine is encountered. This fat pad heralds the proximity of the suprascapular nerve (Fig. 7.9B). Once the posterior interval release is completed, care is taken to ensure that the capsular release underlying the infraspinatus and supraspinatus is also complete and connected to the posterior interval release.
The supraspinatus and infraspinatus tendons are then assessed for mobility (Fig. 7.10A–C). Usually with an isolated posterior interval slide, mobility of the infraspinatus tendon is sufficient for tendon repair to bone. If there is also sufficient mobility for supraspinatus tendon repair to bone, then an anterior interval slide is avoided to maintain the anterosuperior rotator cuff as a single sleeve facilitating repair (Fig. 7.10D). In more severe cases, however, where mobility is insufficient, an anterior interval slide may be required for mobilization of the supraspinatus tendon as well. After repair of the tendon to bone, the separation between the supraspinatus and infraspinatus is closed with margin convergence sutures (Fig. 7.10E).
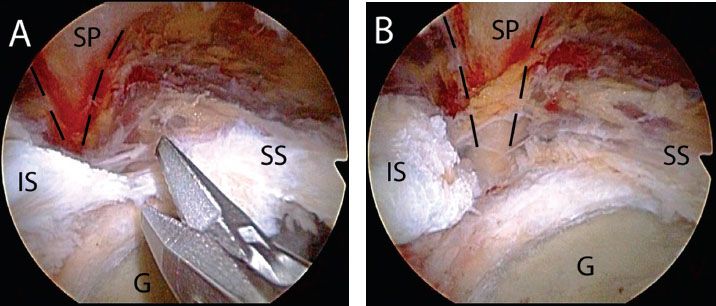
Figure 7.9 A: Arthroscopic view of a right shoulder viewed from a posterolateral portal demonstrating a posterior interval slide performed with arthroscopic scissors. B: The interval slide is completed when the supraspinatus and infraspinatus are completely separated and the perineural fatty tissue at the base of the scapular spine (outlined by dashed black lines) is visualized. G, glenoid; IS, infraspinatus tendon; SP, scapular spine; SS, supraspinatus tendon.
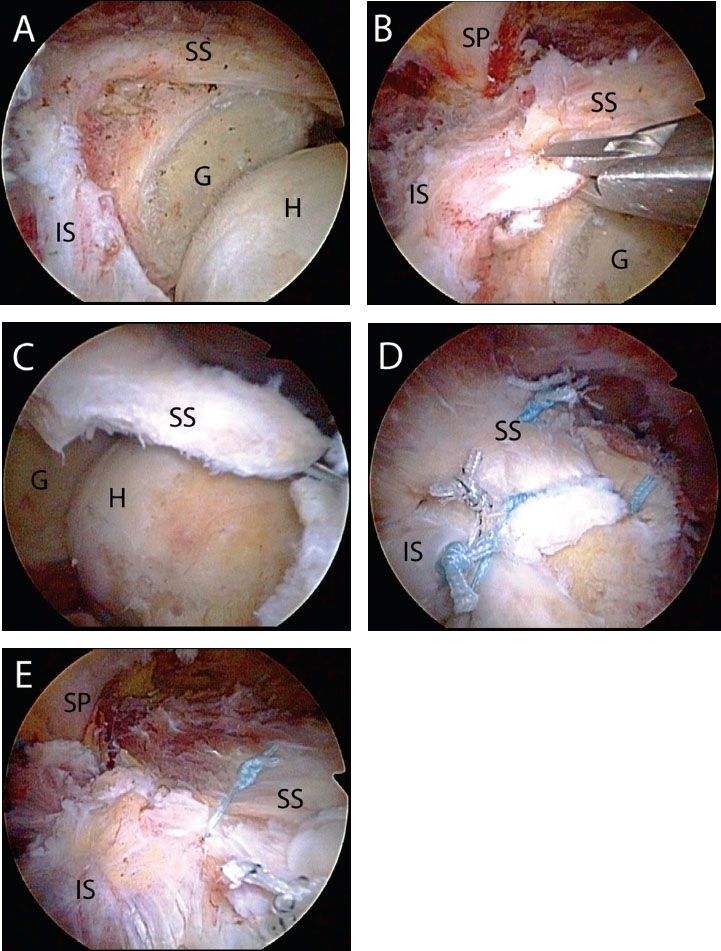
Figure 7.10 The power of the posterior interval slide. A: Right shoulder viewed with a 70° arthroscope from a posterior portal demonstrates a massive rotator cuff tear retracted medially beyond the glenoid rim. B: Initial assessment shows limited mobility. C: Following a posterior interval slide (Fig. 7.9), the mobility of the supraspinatus is dramatically increased and can now reach the greater tuberosity bone bed. D: Final repair shows the rotator cuff secured to the greater tuberosity. E: The separation created by the posterior interval slide has been closed with margin convergence sutures. G, glenoid; H, humerus; IS, infraspinatus tendon; SP, scapular spine; SS, supraspinatus tendon.
ANTERIOR INTERVAL SLIDE
When performing the anterior interval slide, it is easiest to perform the release while viewing through a lateral or posterolateral subacromial portal. The anterior supraspinatus traction stitch is retrieved through the posterior portal to again assist in visualizing the tear apex and positioning the anterior interval. A traction stitch through the rotator interval or subscapularis tendon is not required since these tissues are either intact or have been previously repaired.
The release is performed along the leading edge of the supraspinatus tendon toward the coracoid base, separating the tendon from the rotator interval and subscapularis (Fig. 7.11). The location of the coracoid is again confirmed by palpation using a switching stitch and a spinal needle is used to locate the correct angle of approach in line with the anterior interval. In many instances, the same two lateral portals may be utilized (that were used during the posterior interval slide) and the arthroscope is simply switched to the more posterior lateral portal and the arthroscopic scissors are used through the more anterior lateral portal. However, we do not hesitate to establish another portal if required.
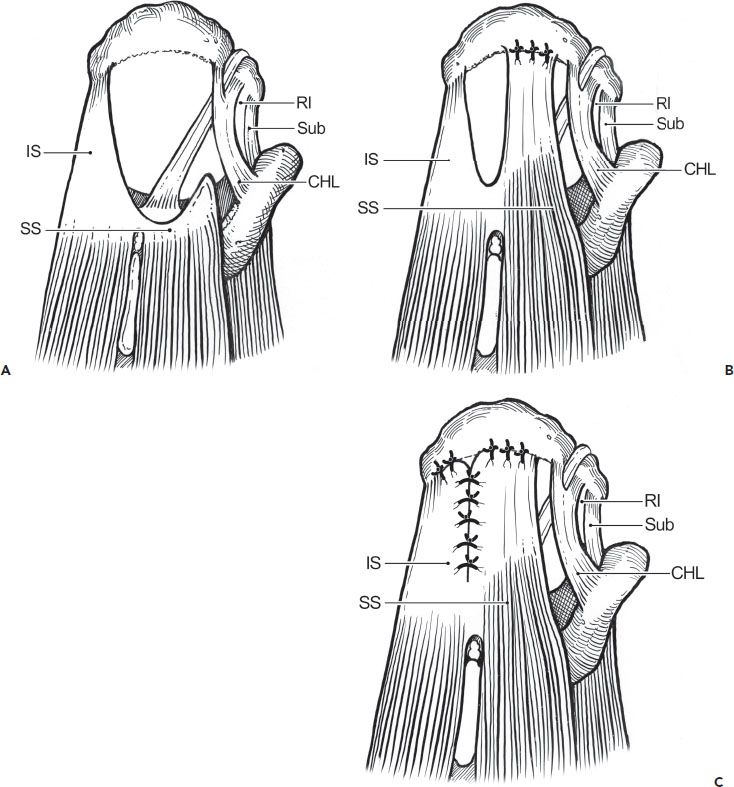
Figure 7.11 Anterior interval slide for repair of a massive contracted immobile longitudinal rotator cuff tear. A: An anterior interval slide is performed by incising the interval between the supraspinatus tendon and rotator interval. This incision releases the posterior portion of the coracohumeral ligament. B: The improved mobility from the release allows repair of the supraspinatus tendon to a lateral bone bed. C: The posterior leaf of the tear, consisting of the infraspinatus and teres minor tendons, is then advanced superiorly and laterally and the residual longitudinal defect is closed by side-to-side sutures. CHL, coracohumeral ligament; IS, infraspinatus; RI, rotator interval; SS, supraipnatus; Sub, subscapularis.
Similar to the posterior interval slide, the anterior interval slide is begun at the margin of the rotator cuff tendon and proceeds toward the bony landmark—in this case, the base of the coracoid. The traction stitch is used posteriorly to distract and improve visualization of the apex and position the anterior interval in line with the arthroscopic scissors. The release is completed when the fat pad medial to the coracoid base is encountered and the coracoid is palpated. Care is taken to ensure that the slide is performed lateral to the coracoid base to avoid injury to the suprascapular nerve.
This anterior interval slide can also be performed without incising the interval tissue (see next section on Anterior Interval Slide in Continuity). This is currently our preferred technique, as it avoids the floppiness of a supraspinatus tendon that has been released on both sides. The one situation in which we will perform a traditional anterior interval slide is when, after a posterior interval slide and an anterior interval slide in continuity, the anterolateral margin of the supraspinatus tendon does not quite reach the bone bed and it is felt that with additional mobility a complete repair will be possible. Once the slide is complete, the capsule underlying the supraspinatus tendon is reevaluated to ensure a complete release has been performed. The supraspinatus tendon is then evaluated for its mobility and reparability.
THE ANTERIOR INTERVAL SLIDE IN CONTINUITY
In patients with combined tears of the subscapularis tendon and supraspinatus tendon (+/− infraspinatus tendon), an interval slide in continuity is preferable to the complete anterior interval slide. By releasing the soft tissues at the base of the coracoid, the coracohumeral ligament is released. It is this ligament that restricts the excursion of a medially retracted supraspinatus tendon. In contrast to a standard anterior interval slide, the interval slide in continuity maintains the connection laterally between the subscapularis and supraspinatus tendon, which simplifies repair of the anterosuperior rotator cuff (Fig. 7.12)
In patients with combined tears of the subscapularis tendon and the supraspinatus tendon, it is important to first address the anterior structures (i.e., subscapularis, biceps, coracoid) prior to proceeding with supraspinatus tendon repair (see Chapter 6, “Subscapularis Tendon Tears” for a complete discussion). It may be necessary to tag and release the long head of the biceps tendon prior to performing the interval slide in continuity.
To perform the interval slide in continuity, it is easiest to view through a posterior glenohumeral portal. An anterosuperolateral portal is established, the comma sign is identified, and a traction stitch is placed in the superolateral corner of the subscapularis tendon if the subscapularis is torn and retracted; if the subscapularis is not torn the following steps are still performed with the only differences being that a traction stitch is not necessary and a posterior release of the subscapularis is not required (Fig. 7.13). The subscapularis tendon is then placed under traction, drawing the subscapularis tendon and rotator interval out from behind the glenoid neck. Starting just above the upper subscapularis tendon border, the rotator interval is then excised using a combination of a shaver and electrocautery (Fig. 7.14A, B). As the dissection proceeds, the hard bony prominence of the coracoid tip can be felt through the rotator interval.
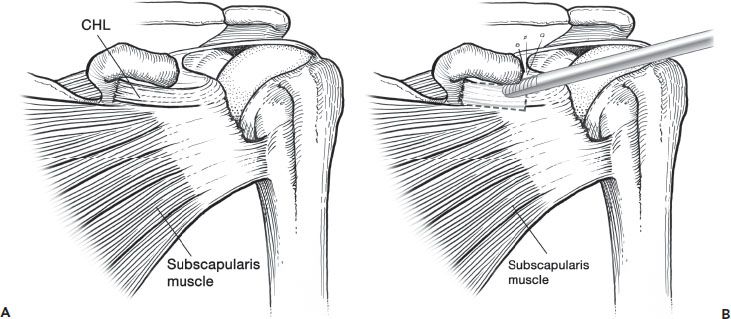
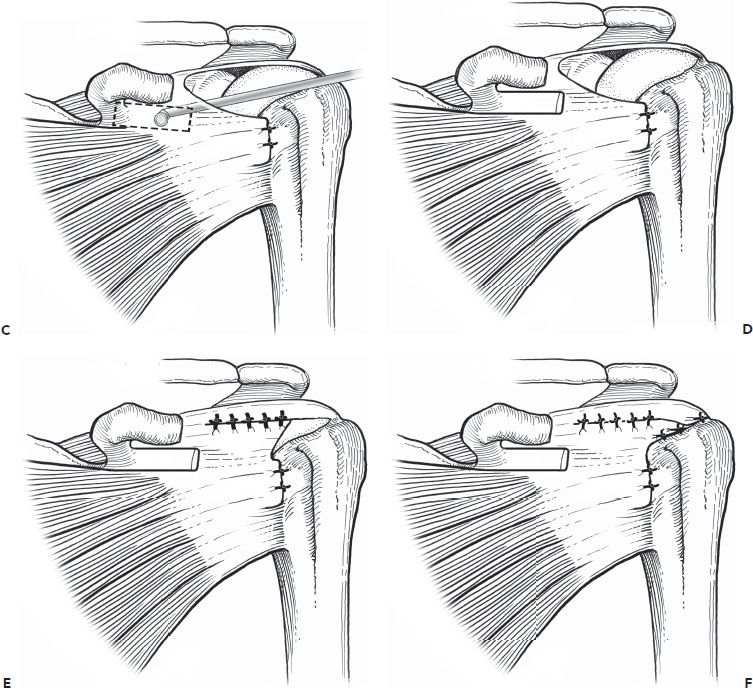
Figure 7.12 Anterior interval slide in continuity. A: An anterosuperior rotator cuff tear involving 50% of the subscapularis tendon and a massive tear of the supraspinatus and infraspinatus tendons. B: A coracoplasty is performed. The dotted box outlines the proposed area for resection of a portion of the rotator interval for the interval slide in continuity. C: An interval slide in continuity is performed by first exposing the posterolateral aspect of the coracoid all the way to the coracoid neck, releasing any adhesions between the subscapularis tendon and the inferolateral coracoid. Then, the medial rotator interval tissue is excised, creating a “window” through the rotator interval, partially releasing and excising the coracohumeral ligament. Care is taken to ensure that the lateral margin of the rotator interval remains intact, maintaining the continuity between the subscapularis and the supraspinatus tendons. Then, soft tissues are debrided and released from the posterolateral base of the coracoid while viewing through the “window” with a 70° arthroscope. This completes the release of the coracohumeral ligament without creating separate tissue flaps. D: Following an interval slide in-continuity, mobility of the subscapularis tendon is improved. The subscapularis tear can now be repaired to bone, leaving a U-shaped posterosuperior rotator cuff tear to be repaired. E: The residual U-shaped posterosuperior rotator cuff tear is repaired with side-to-side sutures using the principle of margin convergence. F: The converged margin is then repaired to bone in a tension-free manner. CHL, coracohumeral ligament.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








