Instability Cases
On the darkest night, the stars are brightest.
CASE 1: COMBINED REVERSE HAGL (RHAGL) LESION AND POSTERIOR BANKART LESION
History:
- 21-year-old man who fell onto outstretched arm during a soccer game
- Patient had the sensation of the arm momentarily slipping out of joint.
Exam:
- Apprehension in position of combined flexion, adduction, and internal rotation; positive posterior load and shift; 2+ posterior drawer at 45° abduction
Imaging:
- X-rays are normal; MRI shows posteroinferior labral disruption.
Arthroscopic Findings:
- Posterior Bankart lesion; reverse HAGL (RHAGL) lesion (Fig. 27.1A)
Procedures Performed:
- Arthroscopic posterior Bankart repair with suture anchors in glenoid
- Arthroscopic RHAGL repair with suture anchors in humerus (Fig. 27.1B)
Key Points:
- Visualization of muscle deep to posterior capsule is pathognomonic of RHAGL lesion.
- Humeral bone bed for RHAGL repair (posterior) is much more accessible than humeral bone bed for HAGL repair (anterior) due to (a) the retroversion of the proximal humerus (presenting a favorable angle for anchor insertion; and (b) the fact that there is no posterior bone structure equivalent to the coracoid that would block access to the bone bed.
- Prepare a 2- to 3-mm bare strip of bone at the glenoid margin for insertion of suture anchors.
- Insert glenoid suture anchors through a posterolateral portal.
- Insert humeral suture anchors through a posterior portal.
- Prepare a 2- to 3-mm bare strip of bone at the glenoid margin for insertion of suture anchors.
CASE 2: COMBINED HAGL LESION AND BANKART LESION
History:
- 42-year-old man who fell 4 feet from ladder onto outstretched left arm. He felt the shoulder dislocate
- After 5 minutes, a coworker pulled on the arm and reduced it.
- After 4 weeks in a sling followed by 6 weeks of physical therapy, the patient continues to have pain and apprehension with any overhead activities.
Exam:
- Positive apprehension in abduction plus external rotation
- Positive load and shift test
- Normal strength
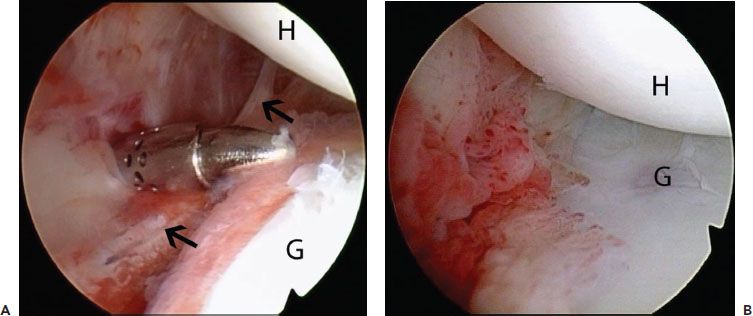
Figure 27.1 A: Left shoulder, anterosuperolateral viewing portal, demonstrates a reverse HAGL (RHAGL) (blackarrows). B: Appearance following suture anchor repair. G, glenoid; H, humerus.
Imaging:
- X-rays show small Hill-Sachs lesion.
- MRI shows Bankart lesion (nondisplaced).
Arthroscopic Findings:
- Bankart lesion
- HAGL lesion
- Shallow Hill-Sachs lesion (Fig. 27.2A)
Procedures Performed:
- Arthroscopic Bankart repair
- Arthroscopic HAGL repair (Fig. 27.2B)
Key Points:
- Bankart lesion and HAGL lesion can both occur simultaneously from a single anterior dislocation event, and must both be looked for.
- The key to diagnosing a HAGL lesion is identifying exposed muscle deep to the anterior capsule.
- Fix the Bankart lesion first, then the HAGL lesion.
- Use a spinal needle to identify the proper angle of approach for the humeral suture anchors for HAGL repair. We call this the “killer angle” because of its acute obliquity to the humeral surface that is a result of: (a) the anatomic position of the humeral bone bed, which is rather inferior; and (b) the necessity to pass the instruments and implants inferolateral to the coracoid, which lies directly in the way of a direct pass. This necessitates a transtendon approach through the subscapularis.
- There will be only a 5° to 10° “window” of allowable angle of approach to permit successful insertion of suture anchors into the humerus. We believe that achieving this “killer angle” of approach is one of the most difficult maneuvers in arthroscopic shoulder surgery. If the surgeon is unable to successfully achieve this angle, he must proceed to an open repair of the HAGL lesion.
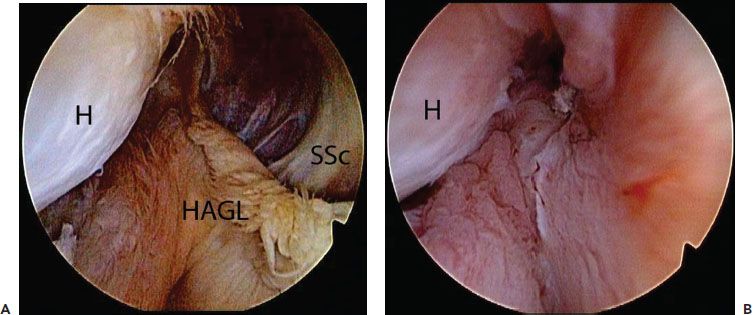
Figure 27.2 A: Left shoulder, anterosuperolateral viewing portal, demonstrates a humeral avulsion of the glenohumeral ligaments (HAGL). B: Appearance postrepair. H, humerus; SSc, subscapularis tendon.
CASE 3: COMBINED ANTERIOR INSTABILITY (AFTER FAILED BANKART REPAIR) AND TEAR OF UPPER SUBSCAPULARIS TENDON WITH SUBLUXATION OF LONG HEAD OF BICEPS
History:
- 32-year-old man who tripped at work and fell onto outstretching right arm
- He felt the shoulder “slip out”
- History of arthroscopic Bankart repair 1 year earlier
Exam:
- Apprehension and pain with combined abduction and external rotation
- Positive bear-hug test
- Positive belly-press test
Imaging:
- X-rays show Hill-Sachs lesion.
- MRI shows Bankart lesion, torn upper subscapularis tendon, and medial subluxation of biceps.
Arthroscopic Findings:
- Recurrent Bankart lesion (Fig. 27.3A)
- 3 mm ´ 7 mm area of grade 4 glenoid chondromalacia adjacent to Bankart lesion
- Shallow nonengaging Hill-Sachs lesion (Fig 27.3B)
- Tear of upper 40% of subscapularis (Fig 27.3C)
- Medial subluxation of long head of biceps
Procedures Performed:
- Arthroscopic revision Bankart repair (Fig 27.4A)
- Arthroscopic subscapularis repair (Fig 27.4B)
- Arthroscopic biceps tenodesis
Key Points:
- Order of steps should be
- Exteriorize the biceps and place whipstitch in preparation for tenodesis. Do this first, before swelling makes it impossible.
- Repair the Bankart lesion, advancing the capsule over the cartilage defect of the anteroinferior glenoid to achieve a biologic resurfacing.
- Repair subscapularis with FiberTape-SwiveLock technique.
- Perform biceps tenodesis with BioComposite Tenodesis screw.
- The Bankart lesion is repaired before the other structures because it represents the tightest working space.
- Knotless repair of tears up to 50% of the superior-to-inferior dimension of the subscapularis with FiberTape-SwiveLock is our preferred technique. For tears of greater than 50% of the inferior-to-superior dimension, we prefer to tie knots with double-loaded BioComposite Corkscrew suture anchors.
- In cases with peripheral glenoid cartilage loss, capsulolabral advancement should be done to provide biologic resurfacing of the damaged glenoid.
CASE 4: TRAUMATIC ANTERIOR AND POSTERIOR BANKART LESIONS SUPERIMPOSED ON PREEXISTING HYPERLAXITY
History:
- 24-year-old female
- Former college swimmer
- Injured shoulder diving for a ball in a softball game
Exam:
- 3+ generalized laxity
- Shoulder is painful with any motion; cannot get a meaningful exam
Imaging:
- X-rays normal
- MRI shows nondisplaced Bankart lesion; no Hill-Sachs lesion.
Arthroscopic Findings:
- Anterior and posterior Bankart lesions (Figs. 27.4A, B)
- Patulous posterior and inferior capsule
Procedures Performed:
- Arthroscopic Bankart repair
- Arthroscopic posterior Bankart repair
- Arthroscopic capsular plication incorporated into capsulolabral repair to suture anchors (Fig. 27.4C)
Key Points:
- Perform anterior Bankart repair before posterior Bankart repair, since working space is more limited anteriorly.
- In hyperlax individuals, plicate capsule to suture anchors using a two-pass technique to gather two separate segments of capsule and more precisely reduce the capsular volume.
- Use a posterolateral portal for placing the posterior glenoid anchors.
- Prepare a 2-mm bare strip of glenoid in order to shift the capsule slightly onto the face of the glenoid.
- Close the posterior portal at the conclusion of the case after all cases of posterior instability repair.
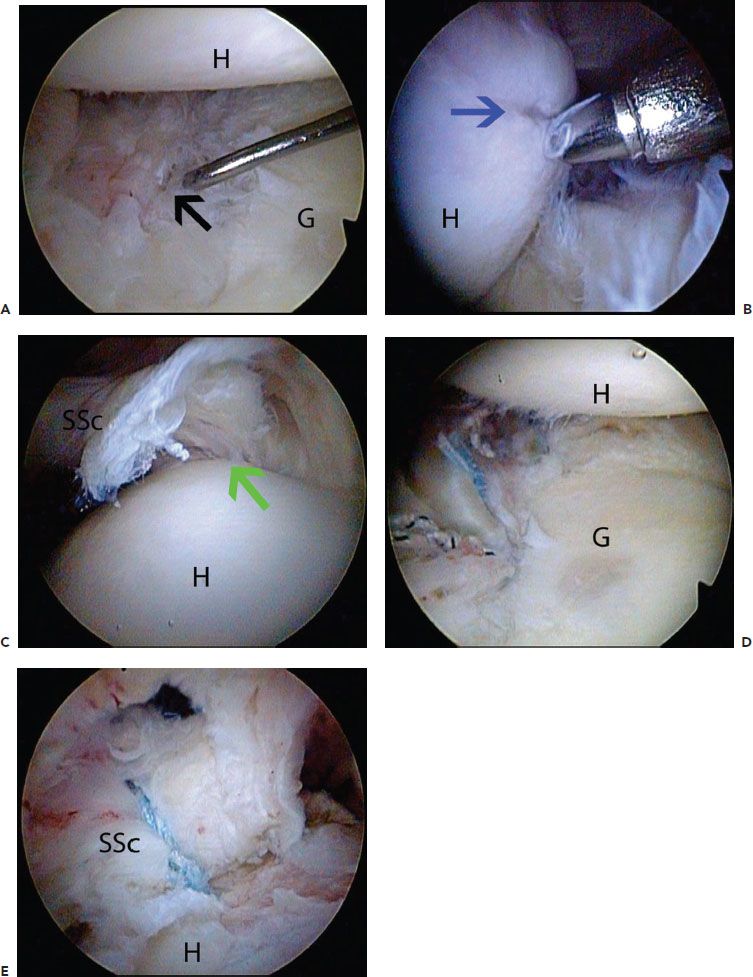
Figure 27.3 A: Left shoulder, anterosuperolateral viewing portal, demonstrates a recurrent Bankart tear (blackarrow). B: Same viewing portal demonstrates a small Hill-Sachs lesion (blue arrow). C: Posterior viewing portal with a 70° arthroscope demonstrates a subscapularis tendon tear (green arrow). D: Anterosuperolateral viewing portal demonstrates appearance post-Bankart repair. E: Posterior viewing portal with a 70° arthroscope demonstrates appearance postsubscapularis tendon repair. G, glenoid; H, humerus; SSc, subscapularis tendon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








