Fig. 4.1
The ball-and-socket hip joint is comprised of the femoral head (ball) and acetabulum (socket). The articular surface is lined with hyaline cartilage. The fibrocartilaginous labrum runs circumferentially around the rim of the acetabulum conforming to the femoral head through effectively sealing the femoroacetabular articulation and regulating the lubrication of the joint surfaces. A thick fibrous capsule reinforced with capsular ligaments encloses the joint
The hip joint possesses greater intrinsic bony stability than other joints due to the congruent coupling between the femoral head and acetabulum. Additional extrinsic stability is provided by a thick fibrous capsule which envelops the hip joint extending from the periphery of the acetabulum to the intertrochanteric line of the femur anteriorly and the femoral neck posteriorly [11]. The iliofemoral and pubofemoral ligaments reinforce the anterior capsule while the ischiofemoral ligament reinforces the posterior capsule. These ligaments coil around the femoral neck and tighten with hip extension enhancing the screw-home stabilizing effect during stance and ambulation [7, 12]. The extracapsular ligamentum teres arises from within the cotyloid fossa to attach to the femoral head fovea.
The fibrocartilaginous labrum runs circumferentially around the rim of the acetabulum effectively sealing the joint. The labrum deepens the acetabular socket expanding its volume and further enhances hip joint stability through maintenance of negative intraarticular pressure [13]. The elasticity of its fibrocartilaginous structure allows the labrum to conform to the femoral head throughout the hip range of motion. This allows it to promote lubrication of the articular surfaces, sustain a vacuum seal that resists joint distraction, and dissipate contact forces across the joint [13]. Similar to the meniscus in the knee, labral fibers are oriented longitudinally parallel to the acetabular rim with a peripheral blood supply that diminishes toward the free margin [10]. Nerve fibers within the labrum provide proprioception and nociception [14]. The labrum is contiguous with the transverse acetabular ligament which crosses the inferior aspect of the acetabulum [10].
History
Some athletes are at increased risk for developing an intraarticular hip injury by virtue of the sports in which they participate [9, 15–17]. Sports such as ice hockey, soccer, and rugby that expose the hip to persistent and intense lateral and rotational movements may generate forces that lead to acute injury or chronic damage [12, 18–23]. Sports that require extremes of range of motion such as dance, gymnastics, and martial arts may exceed the functional limits of the hip [12, 15, 17, 19, 24].
Elements of the injury history may implicate the joint as the source of hip pain (Table 4.1). Intraarticular pain generally localizes to the anterior groin although athletes will often demonstrate the “C-sign” cupping their hand over the lateral hip to describe deep interior hip pain (Fig. 4.2) [25, 26]. The pain may be associated with mechanical symptoms such as clicking, popping, or loss of motion. The athlete with an intraarticular hip injury may tolerate straight-plane activities such as straight-ahead walking or even running while twisting, pivoting, and lateral movement exacerbate the pain [25, 27]. Deep flexion is usually problematic, and the athlete may describe difficulty squatting, putting on shoes and socks, or getting out of a low car seat [27].

• Symptoms worse with activity |
• Straight-plane activities relatively well tolerated |
• Activities on level surfaces better tolerated than on inclines |
• Torsional activities less well tolerated (i.e., twisting such as turning and changing directions) |
• Seated position may be uncomfortable (especially with hip flexion) |
• Rising from seated position often painful (may experience catching sensation) |
• Difficulty ascending and descending stairs |
• Difficulty with shoes, socks, hose, and so forth |

Fig. 4.2
C-sign. (a) This term reflects the shape of the hand when a patient describes deep interior hip pain. (b) The hand is cupped above the greater trochanter with the thumb posterior and the fingers gripping deep into the anterior groin (all rights are retained by Dr. Byrd) [25]
The onset of symptoms in an athlete with an intraarticular hip problem is variable and is dependent upon the etiology. A traumatic injury to a morphologically normal hip may occur with direct impact or after a forceful pivoting, hyperflexion, or traction event. Those athletes generally have no history of hip problems until the trauma. Frequently, hip pain develops insidiously from the repetitive stress of recurrent supraphysiologic demands imposed on the hip. These athletes may loosely associate their hip pain with the increasing training intensity or introduction of new exercises.
Morphological abnormalities of the femoroacetabular articulation predispose the athlete to hip dysfunction. Most do not appreciate a problem with their hip until they suffer an injury. On further questioning, they may recall recurrent groin strains or other non-specific symptoms suggestive of unrecognized intraarticular pathology. They may also present with secondary symptoms seemingly unrelated to the hip such as low back pain or lower abdominal pain. These athletes often report that they lacked the flexibility demonstrated by their teammates but their restricted motion never posed a functional issue [28]. The secondary findings and inflexibility are suggestive of an underlying femoroacetabular impingement (FAI) that limits the hip from achieving extremes in range of motion. While the hip pain may be uncovered or aggravated by an acute event, the damage to the hip joints in these athletes results from the cumulative effects of repetitive injury from an incongruent joint [29].
Examination
A systematic physical examination is central to the evaluation of a suspected intraarticular hip problem (Table 4.2). The athlete should be examined in the standing position from behind to evaluate spinal alignment, pelvic obliquity, and symmetry. Leg length discrepancy may be assessed by comparing the distances between the anterior superior iliac spine and the medial malleolus. During stance, the athlete with a painful hip tends to shift body weight to the unaffected limb and may hold the hip and ipsilateral knee in a slightly flexed position [25]. An antalgic gait may be present as the athlete shortens the stance phase of gait on the affected side and avoids hip extension. Shifting the upper body over the affected hip during ambulation moves the center of gravity closer to the axis of the hip reducing joint reactive forces.
• Groin, anterior, and medial thigh pain |
• “C-sign” characteristic of interior hip pain: hand gripped above greater trochanter |
• Logrolling of leg back and forth: most specific indicator of intraarticular abnormality |
• Forced flexion/internal rotation or abduction/external rotation: more sensitive measure of hip joint pain; reproduces symptoms that patient experiences with activities |
The examiner should adopt a consistent and reproducible method for recording hip range of motion in order to detect subtle abnormalities or asymmetry and follow an athlete with a hip injury [30]. Stabilization of the pelvis during examination negates compensatory pelvic or lumbar spine motion that may be present in an athlete with hip motion restrictions [31]. The presence of a flexion contracture is assessed with the Thomas test (Fig. 4.3). Positions and motions that produce pain, crepitus, or clicking should be noted. Maximum hip flexion, abduction, and adduction are recorded in the supine position while internal and external rotation may be measured in full extension and with the hip flexed at 90°. Alternatively, evaluation of hip rotation may be performed in the prone position or with the athlete seated as this position ensures the ischium is stabilized against the table [31]. Hip extension is measured in the lateral or prone position.


Fig. 4.3
Thomas test. To check extension or presence of a flexion contracture, the unaffected hip is brought into maximal flexion and held by the patient, locking the pelvis. The affected hip is then brought out toward extension and motion recorded (all rights are retained by Dr. Byrd) [25]
Localizing pain to the hip joint during physical examination is challenging due to complex surrounding anatomy. The depth of the hip joint precludes thorough direct palpation and the examiner must use indirect methods to illicit pain from an irritable joint. Logrolling the relaxed lower extremity isolates the hip as the femoral head rotates within the acetabulum without stressing the surrounding soft tissue structures [25]. Pain with resisted straight-leg raise raises suspicion for an intraarticular process as this maneuver applies force across the articular surface [25].
Groin pain with forceful deep flexion, adduction, and internal rotation of the hip is suggestive of impingement morphology as this position generates pathological contact between the femoral head or neck with the acetabulum (Fig. 4.4). Also known as the “impingement test” or “FADDIR” test, this maneuver is not specific to FAI as it usually provokes discomfort in an irritable hip regardless of the underlying pathology [25]. Posterior rim impingement may be detected with forceful hip extension, abduction, and external rotation. Dynamic internal and external rotatory impingement tests are performed by taking the hip through a wide arc of rotation in the adducted and abducted position, respectively [31]. The position of the hip when pain is reproduced provides information about the location of impingement pathology.


Fig. 4.4
Impingement or FADDIR test. Forced flexion combined with adduction and internal rotation is often very uncomfortable and usually elicits symptoms associated with even subtle degrees of hip pathology (all rights are retained by Dr. Byrd) [25]
Intraarticular injection of local anesthetic helps to localize the hip joint as the source of pain [26]. Ultrasound-guided injections may be performed in the office setting or local anesthetic may be administered simultaneously with contrast for an arthrogram. Documentation of the patient’s symptoms before and after the injection elucidates the contribution of intraarticular pathology to groin discomfort. In many cases, the athlete needs to perform the activity that normally produces pain to obtain an accurate determination of the response to the injection.
Coexistent or associated pathology is common in athletes with intraarticular hip disease and should be evaluated particularly when an intraarticular injection fails to or incompletely alleviates symptoms. Potential secondary conditions include tendinitis or strains of the iliopsoas, hip abductors, adductors, external rotators, or abdominal musculature, greater trochanteric or iliopsoas bursitis, athletic pubalgia, osteitis pubis, sacroiliitis, and lumbar radiculopathy.
Imaging
Plain Radiography
A well-centered anteroposterior (AP) pelvis radiograph provides the foundation for the radiographic evaluation of intraarticular hip disease (Fig. 4.5) [31, 32]. Special attention should be paid to ensuring that the coccyx is centered approximately 1–3 cm above the pubic symphysis and the obturator foramina and radiographic teardrops are symmetrical as even slight malrotation or tilting of the pelvis may cloud interpretation of the hip joint.


Fig. 4.5
Anteroposterior pelvis radiograph. The coccyx should be centered approximately 1–2 cm above the pubic symphysis. Iliac wings, acetabular teardrops, and obturator foramina should be symmetrical. This view allows assessment of acetabular inclination and depth, anterior and posterior wall orientation, proximal femur morphology and head sphericity, femoral neck-shaft angle, and bone quality. Additionally, the sacroiliac joints and pubic symphysis are visualized
On the AP radiograph, a number of architectural factors may be assessed including bone density and trabecular patterns, pelvic obliquity and functional leg lengths, acetabular depth and orientation, and proximal femoral morphology [32]. Radiographic indicators of arthritis including joint space narrowing, sclerosis, and osteophyte formation suggest advanced joint damage and portend unfavorable prognosis. The condition of the pubic symphysis and sacroiliac joints should be noted as well as the visualized lumbar spine.
Additional plain radiographic views are needed to fully characterize the osseous anatomy. The frog-leg lateral radiograph provides an orthogonal view of the femoral neck and can provide a comparison lateral view of the contralateral femoral neck (Fig. 4.6). Alternative views used to assess the femoroacetabular joint include the cross-table lateral, 45° and 90° Dunn views, and false profiles. Some surgeons advocate at least one of the radiographs in the series should be weight-bearing to assess for degree and location of joint space narrowing.


Fig. 4.6
Frog-leg lateral hip radiograph. An orthogonal view of the proximal femur morphology and further analysis of the sphericity of the femoral head is afforded by this radiographic view. A cross-table lateral or false profile is needed to further image the acetabulum
Cross-Sectional Imaging
Pathology involving the complex three-dimensional articulation of the femoroacetabular joint is best characterized by cross-sectional imaging such as magnetic resonance imaging (MRI) or computed tomography (CT).
Advantages of MRI include depiction of intraarticular soft tissue structures, in particular the labrum, visualization of the surrounding soft tissue envelope, and demonstration of secondary findings including intraosseous and soft tissue edema, paralabral and subchondral cysts, and effusions [24, 33]. MRI is not optimal for assessing osseous anatomy and may underestimate the severity of articular cartilage injury [26]. Additionally, the modality is only as good as the strength of the magnet and poor resolution images are difficult to interpret [34]. High resolution small field of view images necessitate at least a 1.5-Tesla magnet with surface coils [26].
MR arthrography (MRA) after injection of intraarticular gadolinium improves the sensitivity and specificity of MRI, but the contrast prevents detection of an effusion and obscures edema in the surrounding tissues (Fig. 4.7) [26]. Pre- and post-contrast studies increase the diagnostic capabilities of MRI.
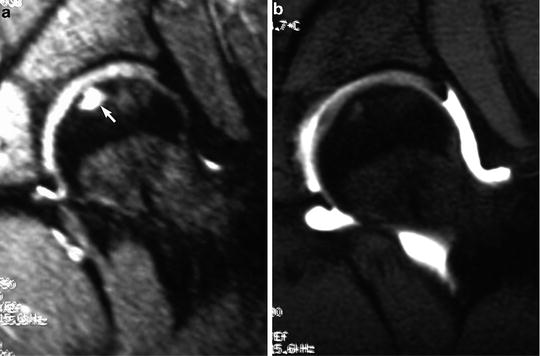
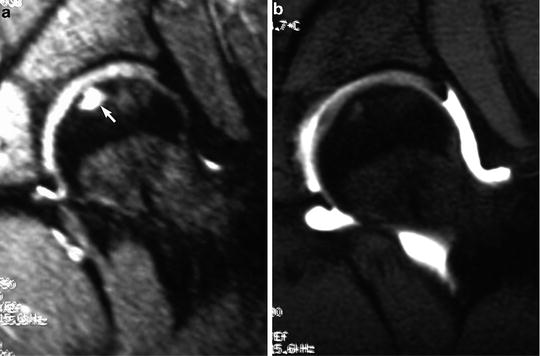
Fig. 4.7
Magnetic resonance imaging. (a) Conventional MRI is an excellent imaging modality to diagnose intraarticular pathology. In this image, subchondral signal changes are demonstrated in the femoral head (arrow). (b) Intraarticular contrast enhances visualization of the labrum but obscures the subchondral changes
Computed tomography has gained widespread application for imaging of the hip, in particular for the characterization of the anatomy underlying FAI. CT is superior to MRI for clearly defining the bony architecture of the acetabulum, and reformatting with three-dimensional reconstructions provides the clearest view of the proximal femoral morphology (Fig. 4.8) [28, 35]. The primary disadvantage of CT is the exposure to ionizing radiation [35].


Fig. 4.8
Three-dimensional CT. Excellent demonstration of acetabular and proximal femoral morphology is afforded by CT with 3-D reconstruction
Arthroscopy
Compared to the rapid implementation of arthroscopy for the shoulder and the knee, the adoption of hip arthroscopy has been more deliberate. Historically, the tight articulation between the femoral head and acetabulum posed an inherent anatomical obstacle to achieving any meaningful surgical correction with arthroscopic technique and required a more methodical evolution of instrumentation and methods [36]. Additionally, unlike the multiple indications for shoulder and knee arthroscopy, intraarticular hip pathology amenable to arthroscopic intervention has only been recently recognized and understood. Advances in techniques, such as the use of traction and the development of specialized instrumentation, have allowed improved access to the hip and generated increasing interest in hip arthroscopy as an alternative to more invasive open procedures, in particular for the young, athletic population [37–39].
Hip arthroscopy has now emerged as the gold standard for surgical management of intraarticular pathology in the athletic hip [27, 37, 40]. The proliferation of hip arthroscopy has been self-perpetuated as the technique has revealed previously unrecognized etiologies of hip pain that can be treated arthroscopically [40]. Conditions amenable to arthroscopic intervention include labral tears, loose bodies, chondral injuries, ligamentum teres ruptures, snapping hip, capsular laxity, and intraarticular proliferative disorders (Fig. 4.9) [10, 15, 41, 42]. Osteoplasty of the acetabulum and/or femoral head in athletes with FAI may also be performed arthroscopically and offers the advantage of improved visualization over mini-open techniques, and less exposure-related morbidity compared to mini-open and surgical dislocation techniques [15, 34, 43, 44].
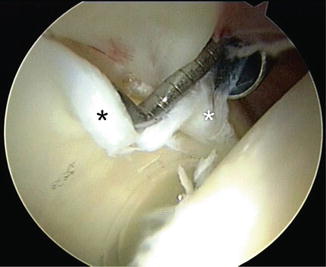
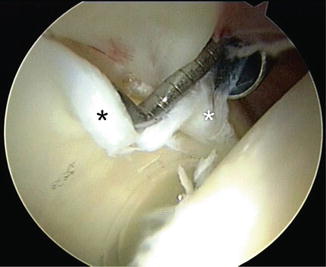
Fig. 4.9
Arthroscopic appearance of a labral tear associated with pincer femoroacetabular impingement.
Despite the advances and proliferation of hip arthroscopy, strict adherence to the diagnostic and treatment algorithm is critical for successful application of the technique. Patient selection is paramount for ensuring a successful hip arthroscopy and reasonable expectations should be set. Prior to hip arthroscopy, an athlete should undergo a conservative treatment protocol aimed at reducing inflammation and optimizing pelvic biomechanics. Acute intraarticular injuries, mechanical symptoms, and correctible structural abnormalities carry the best prognosis for arthroscopic intervention [10, 16, 25, 35]. Patients with chronic pain, advanced arthritis, avascular necrosis, and/or significant dysplasia likely will not benefit from arthroscopy [38, 41, 45]. Potential complications include nerve injury from portal placement, traction-related neurapraxia, compression of perineal structures, iatrogenic chondral or labral injury, and fluid extravasation [38, 40, 46].
Femoroacetabular Impingement
Essentially all hip range of motion is rotational, the absolute limits of which are defined by position of the joint when the femoral neck contacts the acetabular rim [11]. The arc of motion reflects the depth and orientation of the acetabulum within the pelvis and the relative size, shape, and orientation of the femoral head and neck [11]. Impingement occurs when a mismatch between the ball and socket causes abnormal contact between the proximal femur and the acetabulum during a physiologic arc of motion [5]. The significance of the mismatch is influenced by the severity of the deformity and the demands upon the joint. A mild deformity that may be asymptomatic to an average person may be poorly tolerated by an athlete that requires extremes in hip motion.
Ultimately, the pathological biomechanics result in chondral and labral damage and predisposes the hip to osteoarthritis [5]. Additionally, secondary pathology often develops in athletes with FAI in response to the restricted range of motion and intraarticular pain. Abnormal compensatory motion within the ipsilateral hemipelvis and lumbosacral spine may lead to muscle strains, tendinitis, bursitis, arthritis, and/or athletic pubalgia [17, 47, 48]. The athlete may develop a reflexive gait alteration in an attempt to unload the painful hip joint that disrupts the sagittal and coronal plane balance within the pelvis [15].
Two mechanisms of FAI have been described based on the location of the pathology. Pincer impingement is caused by an acetabular deformity in which the rim of the acetabulum abnormally contacts the femoral neck restricting motion [5]. Cam impingement is caused by a deformity of the femoral head–neck junction that results in conflict between the nonspherical ball rotating within the socket [5, 29]. Frequently, deformities on both the acetabular and femoral side contribute to impingement resulting in a mixed type [5, 49]. A recent epidemiological study of 1,130 hips with FAI reported isolated cam impingement in 47.6 %, isolated pincer in 7.9 %, and mixed cam/pincer impingement in 44.5 % of cases [50].
Pincer Impingement
Pincer impingement is characterized by acetabular overcoverage of the femoral head that impedes terminal hip motion by premature contact between the acetabular rim and the femoral neck (Fig. 4.10) [51]. The pathology underlying pincer impingement is usually localized anteriorly on the acetabulum leading to contact with hip flexion. As the femoral neck collides with the acetabular rim, the labrum is trapped between the bony structures and becomes damaged with repetitive trauma. With further hip flexion, the acetabular rim acts as a fulcrum upon which the femoral neck levers the head from the socket. The resulting impact of the posteromedial femoral head on the posteroinferior acetabulum leads to chondral damage in these locations. Reactive changes and cyst formation may also occur on the femoral neck in response to persistent contact with the acetabular rim.
Fig. 4.10
Pincer impingement. (a) Acetabular overcoverage leads to pathological contact with the femoral neck. (b) The labrum is trapped between the two bony surfaces leading to damage with repetitive impingement
Morphological features of the acetabulum that result in pincer impingement include abnormal rim shape, acetabular retroversion, or excessive acetabular depth (coxa profunda or protrusio). Prominence of the anterior inferior iliac spine has also been reported as a potential etiology for pincer impingement [52]. More commonly found in females, pincer impingement appears to have a genetic element. Siblings of patients with pincer deformity have a relative risk of 2.0 of having the same deformity [53].
Range of motion deficits may be subtle and reflect the magnitude of the deformity. The athlete may be able to unintentionally avoid the position of impingement by simultaneously externally rotating the hip with deep flexion [51]. While asymptomatic with routine activity, increasing athletic activity overcomes this protective mechanism and produces symptomatic impingement [54]. Mechanical symptoms such as clicking or popping arise with progressive labral pathology. Restricted range of motion may be detected on examination and impingement maneuvers reproducibly provoke groin discomfort [51].
Radiographic markers of pincer impingement on an AP pelvic radiograph include decreased acetabular inclination, a cross-over sign, and coxa profunda (Fig. 4.11) [32, 55]. Prominence of the ischial spine is associated with acetabular retroversion [56]. Sclerosis and cystic changes on the femoral neck may be suggestive of herniation pits from repetitive impingement [51]. Anterior overcoverage is demonstrated by an increased center-edge angle on a false-profile radiograph [32]. Cross-sectional imaging findings characteristic of pincer impingement include increased acetabular depth and acetabular retroversion [33]. Labral tears and herniation pits associated with pincer impingement may be demonstrated on MRI [24, 55].
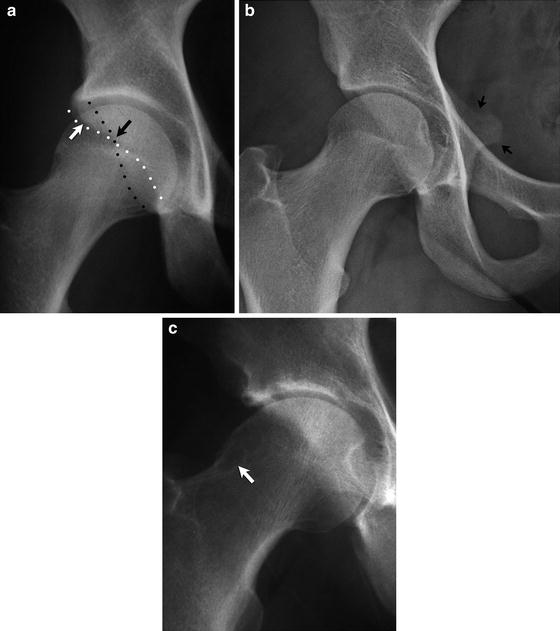
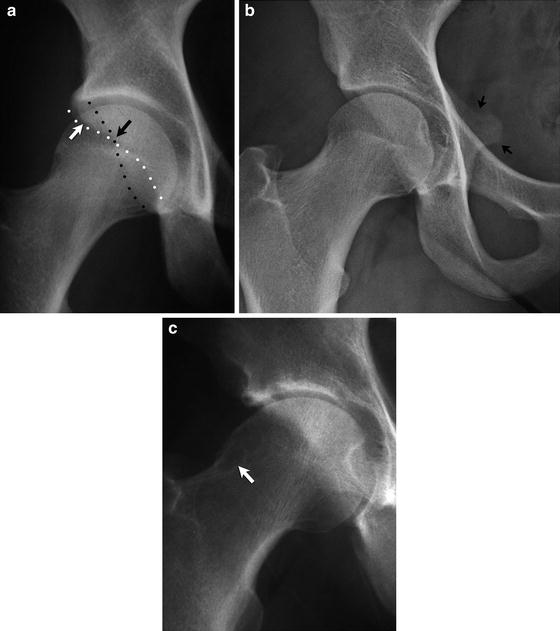
Fig. 4.11
(a) Cross-over sign. Anterior overcoverage or acetabular retroversion that may predispose to pincer impingement is characterized by a cross-over sign on an AP radiograph in which the anterior acetabular rim (white arrow) crosses over the posterior rim (black arrow). (b) A prominent ischial spine suggests acetabular retroversion. (c) Repetitive pathological contact with the acetabular rim may produce cystic changes on the superolateral femoral neck
Cam Impingement
Cam impingement is characterized by an abnormal prominence of the femoral head/neck junction that results in a nonspherical shape and as a result an incongruent joint (Fig. 4.12) [29, 57]. The size and location of the cam lesion is variable but generally it involves the anterior or anterolateral femoral head/neck junction and engagement occurs with hip flexion and internal rotation [29, 57]. Articular incongruity and loss of the femoral head/neck offset restrict motion [16]. The cam effect produced as the prominence engages the acetabulum leads to shear at the articular surface, and chondral delamination and failure of the articular surface occurs with forceful and/or repetitive motion [29, 57]. The pathological contact of cam impingement is within the acetabular vault and as a result the labrum is often preserved initially although secondary damage may occur with disease progression [57].
Fig. 4.12
Cam impingement. The nonspherical femoral head creates a cam effect with hip rotation. The prominence of the head/neck junction engages the acetabulum resulting in shear forces across the articular surface and cartilage damage and delamination
Cam impingement affects male athletes approximately three times more frequently than their female counterparts [29]. Siblings of patients with cam deformity have been shown to have a relative risk of 2.8 of having the same deformity [53]. Vigorous athletic activity during adolescence has been proposed as a risk factor due to the stresses on the developing hip joint [58]. Asymmetrical closure of the capital femoral epiphysis may produce the pistol grip deformity that underlies cam impingement [58]. Slipped capital femoral epiphysis or physeal fracture may also be responsible for the deformity.
Like pincer impingement, cam impingement is frequently asymptomatic in athletes until increasing demands of the sport uncover the abnormal hip anatomy. Consequently, age of onset is influenced by participation in athletics [29]. In individuals with cam-type morphology who do not participate in athletics, symptoms may not present until middle-age when elements of osteoarthritis have developed [29].
The pistol grip deformity suggestive of cam impingement may be evident on the AP pelvis radiograph although frequently the anatomy responsible for cam impingement is more subtle [59]. The location of the cam lesion is variable and multiple views of the proximal femur may be necessary to adequately visualize it [57]. The deformity is usually most clearly demonstrated on a lateral view and is characterized by an increased alpha-angle representative of loss of femoral head sphericity (Fig. 4.13) [32]. Femoral head–neck offset can also be quantified on a lateral radiograph [32].
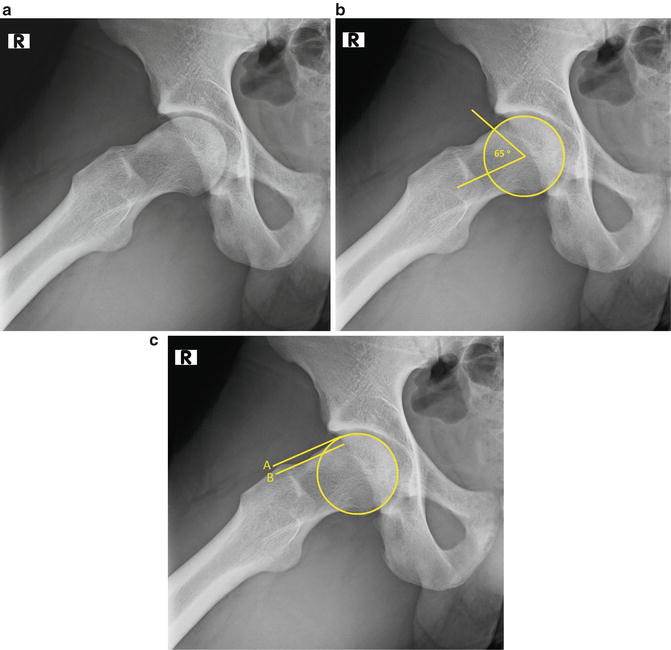
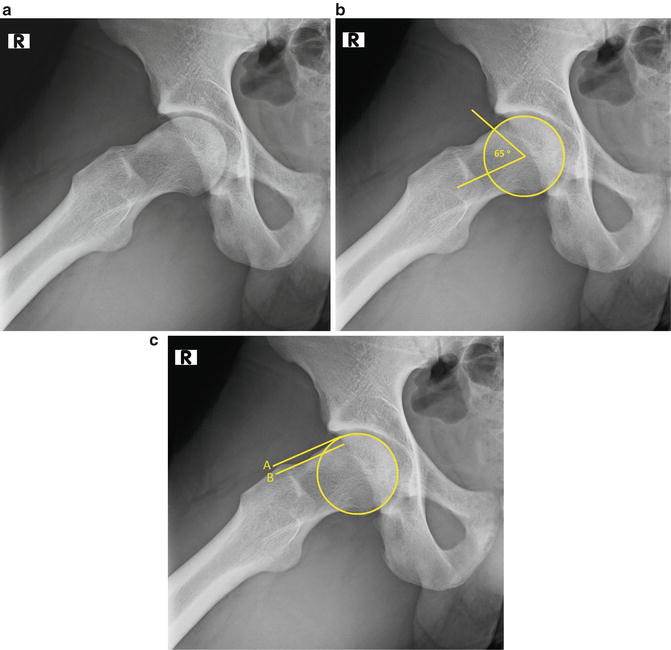
Fig. 4.13
(a) Prominence of the femoral head/neck junction is demonstrated on this frog-leg lateral radiograph. (b) Alpha angle. A circle is placed over the femoral head on a lateral radiograph. The alpha angle is formed by a line along the long axis of the femoral neck and a line from the center of the femoral head to the point at which the bony contour exits the circle. An alpha angle greater than 55° is associated with cam impingement. (c) Head–neck offset. Two lines parallel to the long axis of the femoral neck are drawn, line A through the most anterior aspect of the femoral head and line B through the most anterior aspect of the femoral neck. The femoral head–neck offset ratio is calculated by measuring the distance between the two lines and dividing by the diameter of the femoral head. A ratio of <0.17 is associated with cam deformity
Cross-sectional imaging is necessary to fully characterize the cam lesion and should be used to supplement plain radiographs. Computed tomography or MRI allow improved localization of the deformity and afford more precision in measurement of alpha angle and femoral head/neck offset. Computed tomography with three-dimensional reconstructions provides the most accurate representation of the size, shape, and location of the cam lesion and is a powerful preoperative tool for osteoplasty planning (Fig. 4.14) [57].
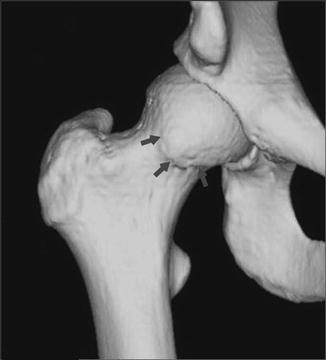
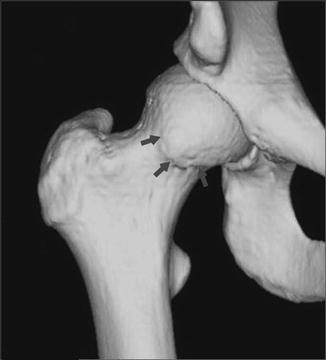
Fig. 4.14
Three-dimensional CT helps to demonstrate the size, shape, and location of the cam lesion
Treatment of FAI
The initial management of an athlete with FAI should emphasize optimizing the biomechanics of the hip joint through a systematic non-operative algorithm. In most cases, the athlete has become symptomatic because of the increased demands on the hip from training or participation in his or her sport. Activity modification is central to conservative management, and successful treatment may be as simple as correctly identifying and avoiding the offending activity [57]. An individualized physical therapy program is formulated through an analysis of athletic demands, hip range of motion, compensatory changes in the pelvis and lumbar spine, posture, and muscular strength and flexibility [16]. Functional improvement in hip biomechanics may be obtained by core and hip muscle strengthening, postural adjustments, and stabilization of the pelvis [60]. Non-steroidal anti-inflammatories may be used to control symptoms, and the judicious use of intraarticular steroid injections has utility as a diagnostic and therapeutic tool [61].
While conservative treatment may improve symptoms, the fundamental anatomical deformity that underlies FAI frequently requires surgery to address the articular mismatch [34]. Delay in surgical correction may accelerate disease progression, particularly in those athletes with more significant deformities [5, 16, 34]. Surgical intervention involves osteoplasty of the acetabulum and/or proximal femur to correct the anatomical factors that contribute to the mechanical conflict between the two surfaces (Fig. 4.15) [5]. Additionally, secondary pathology including labral tears and chondral damage may be addressed. Although the primary objective of surgery is to eradicate pain and return the athlete to play, a secondary but perhaps more important objective is to prevent future degenerative changes associated with impingement [16, 35].
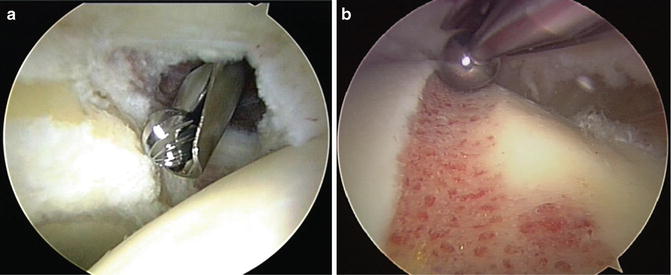
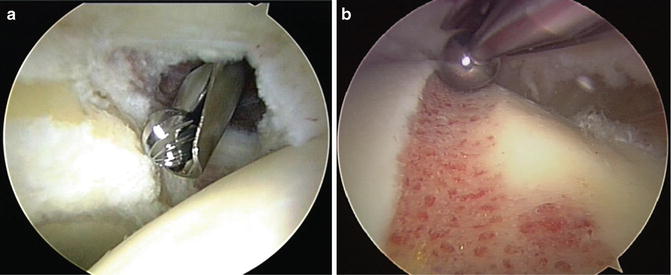
Fig. 4.15
(a) Arthroscopic correction of pincer lesion of the acetabular rim. (b) Arthroscopic femoroplasty to address a pathological cam lesion
Open surgical dislocation provides outstanding exposure for reshaping of the proximal femur and/or acetabulum and good outcomes with reliable return to play have been reported [62]. While effective surgical correction can be obtained, the potential complications and exposure-related morbidity limit widespread utilization in athletes [44, 63]. Less invasive open approaches have been introduced with less exposure-related morbidity, but poor access to the joint may result in inadequate correction and need for revision [44, 64].
The evolution of arthroscopic instrumentation and techniques has established hip arthroscopy as a mainstay of treatment for FAI [39]. Correction of the impingement deformity has been demonstrated to be equivalent to open surgical dislocation [65, 66]. Arthroscopy also has been shown to have equal to or better outcomes than open methods with minimal exposure-related morbidity and fewer complications [44]. In a study of 47 athletes with FAI, Nho et al. demonstrated a significant improvement in hip functional outcome and a 79 % rate of return to play at a mean of 9.4 months post-operatively. Philippon et al. [43] report high patient satisfaction and 100 % return to play at an average of 3.8 months in 28 professional hockey players who underwent arthroscopic treatment of FAI. Byrd and Jones [67] report return to previous level of competition in 95 % of professional athletes and 85 % of collegiate athletes among 116 athletes studied.
Labral Tears
Labral tears are common in athletes with hip pain and are a leading indication for hip arthroscopy [22, 41]. Athletes who participate in sports that require repetitive pivoting or deep hip flexion such as ice hockey, soccer, dance, and football are at increased risk [1, 10, 38, 68, 69]. Isolated acute traumatic labral tears in a structurally normal hip are uncommon but may result from a subluxation event or severe pivoting force [70]. More commonly, an underlying structural abnormality such as FAI, hip dysplasia, capsular laxity, or hip hypermobility predisposes the labrum to injury [69, 70]. In a recent study of 1,076 patients with FAI, more than 90 % were found to have labral tears during arthroscopy [50].
Groin pain with associated mechanical symptoms is a hallmark of labral injury [10]. The athlete may correlate onset of pain to a specific traumatic injury but frequently symptoms develop insidiously with episodic activity-related exacerbations [1]. The presentation is variable and often concomitant symptoms from secondary conditions such as adductor or iliopsoas tendinitis obscure the diagnosis [1]. Physical examination will demonstrate an irritable hip with positive impingement signs. Motion abnormalities suggest underlying FAI or acetabular dysplasia. Reproducible clicking with hip rotation may indicate an unstable labral tear, but this finding may also be present with an incidental extra-articular cause such as a snapping iliopsoas tendon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







